Translate this page into:
Foam sclerotherapy in various vascular and lymphatic malformations
Correspondence Address:
G R Ratnavel
Department of Dermatology, Venereology and Leprosy, Government Stanley Medical College and Hospital, Chennai - 1
India
| How to cite this article: Ratnavel G R. Foam sclerotherapy in various vascular and lymphatic malformations. Indian J Dermatol Venereol Leprol 2011;77:336-338 |
Sir,
Sclerotherapy is the procedure in which chemical energy delivered intravascularly is capable of denaturating biological molecules in the vessel wall. Foam sclerotherapy, in which the sclerosant is mixed with air or physiological gases, is more efficacious than direct injection of sclerosant, [1] as air in the foam prolongs the contact of the agent with the endothelium. Hence, maximum sclerosant action can be obtained at a lesser concentration and quantity. The foamed agent exerts its effect at microcirculation, which is inaccessible to other procedures. We here share our experience in treating varicose veins, hemangiomas and lymphangiomas with foam sclerotherapy.
After ethical clearance, informed and written consent, we enrolled 20 patients with varicose veins (legs), seven with hemangioma (tongue, gluteal region, hand, trunk of size from a minimum of 3 cm x 2 cm to a maximum of 12 cm x 8 cm) and one with lymphangioma (posterior one-third of the tongue) of the mean age group of 32.7 years (14-54 years) of both sexes for a study period of 1 year from April 2009 to April 2010.
Patients with primary varicose veins (varicosities due to incompetent valves in the veins without perforator or junctional incompetencies), telangiectasias, patients unfit for surgery or with recurrence after surgery and those after surgical ligation of major refluxes were included. Those with deep venous thrombosis, reflux from major junctions, perforator incompetence, coagulation abnormalities, hypersensitivity to the sclerosant, pregnant or lactating women and those who were on oral contraceptive pills or hormone replacement therapy were excluded.
Duplex Doppler ultrasonogram of the vascular system, ultrasonogram of the abdomen and pelvis and coagulation profile were performed. In hemangiomas and lymphangiomas, in addition, contrast-enhanced computed tomography (CT) scan and magnetic resonance imaging were performed.
Sodium tetradecyl sulfate 3% (STS), an EDA- and FDA-approved detergent sclerosant was diluted with normal saline. Quantity per session and concentration used were based on the diameter of the vessel, size of the hemangioma and response to therapy. The concentration of the injected sclerosant is determined mainly by the mural thickness of vein, which is directly correlated with lumen diameter as given below.
- <0.5 mm - 0.1%
- 0.6-1.5 mm - 0.25%
- 1.5-4 mm - 0.5-1%
- 4-6 mm - 1-2%
Calculation of dilution volumes are as given below.
C f = C i [ V s / (V s + V d )]
C f - final concentration (in %) of sclerosant
C i - initial concentration (in %) of sclerosant
V s - initial volume (in ml) of undiluted sclerosant
V d - diluent volume (in ml) of 0.9% saline solution
After diluting, foaming of the sclerosant was done by the "Tessari" method, [2] in which a 5-ml syringe was filled with room air, another syringe was filled with 1 ml of the diluted sclerosant and the two syringes were connected to a 3-way stop cock [Figure - 1]. Foaming was done by a to and fro movement of both the syringes. The vein was cannulated using a scalp vein set from the distal end and the hemangiomatous mass [3] was cannulated at the base and, after ensuring that blood was coming out through the cannula, the vein was emptied by elevation of the limb and the foam sclerosant was slowly introduced. Compression bandaging was performed, which was to be worn for 2 weeks, and the patients were advised to be ambulant, to keep their legs elevated, to avoid strenuous exercise and standing still for long periods.
 |
| Figure 1: Foaming by the "Tessari": method and hemangioma-tongue being cannulated |
They were followed-up every 2 weeks and the procedure was repeated after every 4 weeks depending on the clinical response (fibrosis of vessels, reduction in the size of the hemangioma). Doppler ultrasonogram was repeated every 2 months.
Of the 20 patients with varicose veins, 15 (75%) showed remarkable improvement symptomatically and cosmetically (two to five sessions), two (10%) showed partial improvement, two (10%) had complications like staining of the skin and ulceration and one (5%) had recurrence.
Of the seven patients with hemangioma, six (85.7%) showed near-complete resolution (two to eight sessions) and one (14.3%) showed partial resolution. One patient with lymphangioma showed near-complete resolution in four sessions [Figure - 2] and [Figure - 3].
 |
| Figure 2: Before and after treatment photographs - lymphangioma posterior one-third of the tongue and varicose vein-leg |
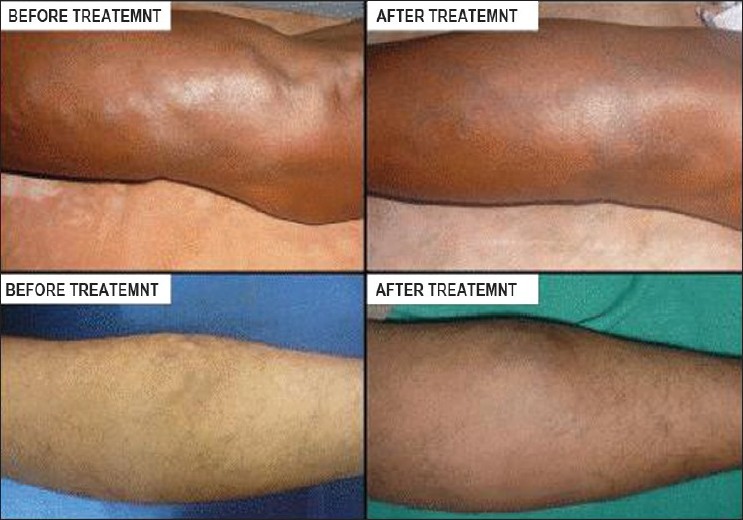 |
| Figure 3: Before and after treatment photographs - varicose veins (leg) |
Although complications like allergic reactions, leg swelling, cutaneous necrosis, thromboplebitis, deep vein thrombosis, transient ischemic attacks and pulmonary embolism have been reported, [4],[5] we noticed only staining of skin and cutaneous ulceration, which healed with conservative management. We observed a faster healing of venous ulcers and stasis eczemas, which usually respond slowly to conservative treatment.
Although other procedures like surgery, laser and radiofrequency ablation and electrodessication are available for the treatment of varicose veins, foam sclerotherapy is a simple, safer, feasible, and affordable office procedure, which has an enhanced success rate over other procedures. It favors quicker healing of venous ulcers and stasis eczemas.
| 1. |
Yamaki T, Nozaki M, Iwasaka S. Comparative study of duplex-guided foam sclerotherapy and duplex-guided liquid sclerotherapy for the treatment of superficial venous insufficiency. Dermatol Surg 2004;30:718-22.
[Google Scholar]
|
| 2. |
Tessari L, Cavezzi A, Frullini A. Preliminary experience with a new sclerosing foam in the treatment of varicose veins. Dermatol Surg 2001;27:58-60.
[Google Scholar]
|
| 3. |
Winter H, Dräger E, Sterry W. Sclerotherapy for treatment of hemangiomas. Dermatol Surg 2000;28:11-5.
[Google Scholar]
|
| 4. |
Scurr JR, Fisher RK, Wallace SB. Anaphylaxis Following Foam Sclerotherapy: A Life Threatening Complication of Non Invasive Treatment for Varicose Veins. EJVES Extra 2007;13:87-9.
[Google Scholar]
|
| 5. |
Campbell B. Varicose veins and their management. BMJ 2006;333:287-92.
[Google Scholar]
|
Fulltext Views
3,320
PDF downloads
2,267





