Translate this page into:
Focal ulcero-proliferative gingivitis: A rare presentation of mucosal tuberculosis
Corresponding author: Prof. Aparna Palit, Department of Dermatology, and Venereology, AIIMS, Bhubaneswar - 751 019, Odisha, India. apalit2011@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Patel NH, Padhiyar JK, Patel T, Patel A, Chhibber A, Raval R, et al. Antiphospholipid antibodies in a patient of Lucio phenomenon presenting with the gangrene of digits. Indian J Dermatol Venereol Leprol 2021;87:106-108.
Sir,
A 35-year-old woman presented with a 10-month-old history of a painful non-healing ulcer on the anterior aspect of the lower gum towards the left side. A prior history of trauma or dental procedure was absent. She denied any personal or family history of tuberculosis. There was no history of loss of appetite, weight loss, evening rising of temperature, epistaxis, breathlessness, diarrhea, abdominal pain or any other mucocutaneous lesion. Multiple courses of oral antibiotics and topical antiseptics were tried without any significant improvement. Local examination revealed erythema, erosions and ulcero-proliferative swelling on the anterior aspect of mandibular gingiva towards the left side [Figure 1]. Other general and systemic examinations were within normal limits. Differential diagnoses of Crohn’s disease, Wegner’s granulomatosis, deep fungal and tubercular infections were considered. Her erythrocyte sedimentation rate was 40 mm/hour. Mantoux test read 32 mm at 48 hours. Other investigations were within normal limits. A biopsy from the lesion revealed well-circumscribed foci of epithelioid granulomas cuffed with abundant lymphocytes, admixed with Langhans and foreign body giant cells. Special stains for acid-fast bacilli and fungal elements were negative [Figures 2a and b]. A cartridge-based nucleic acid amplification test by gene Xpert Mycobacterium tuberculosis/rifampicin assay from mucosal tissue was positive for Mycobacterium tuberculosis DNA. A diagnosis of tubercular gingivitis was made, and the patient was started with category-I antitubercular therapy consisting of isoniazid, rifampicin, pyrazinamide and ethambutol for 2 months followed by isoniazid and rifampicin for 4 months. Her oral lesions improved gradually and complete healing occurred by 6 months [Figure 3].

- Ulcero-proliferative gingivitis
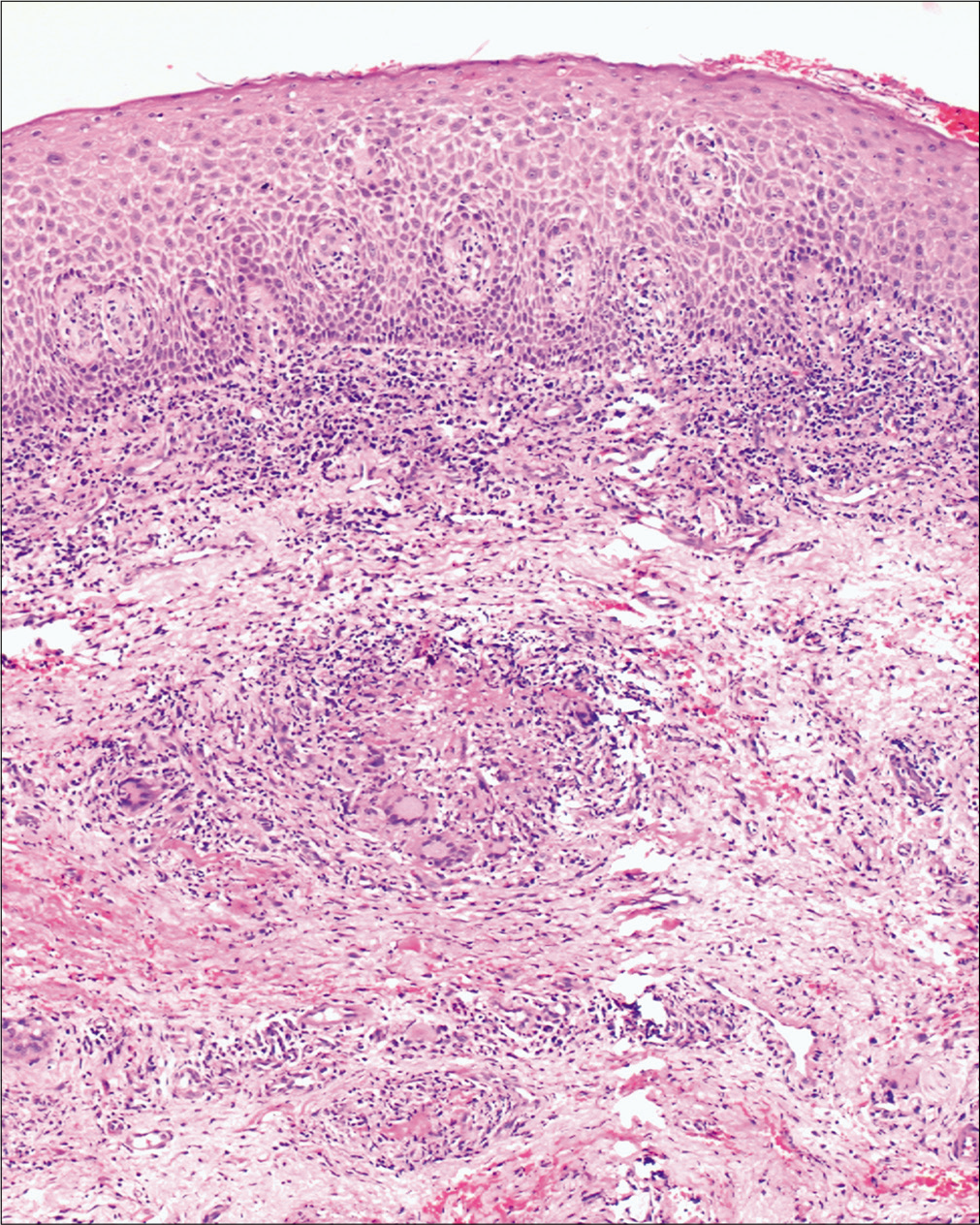
- Epithelioid granuloma with giant cells surrounded by lymphocytes (hematoxylin and eosin, ×100)
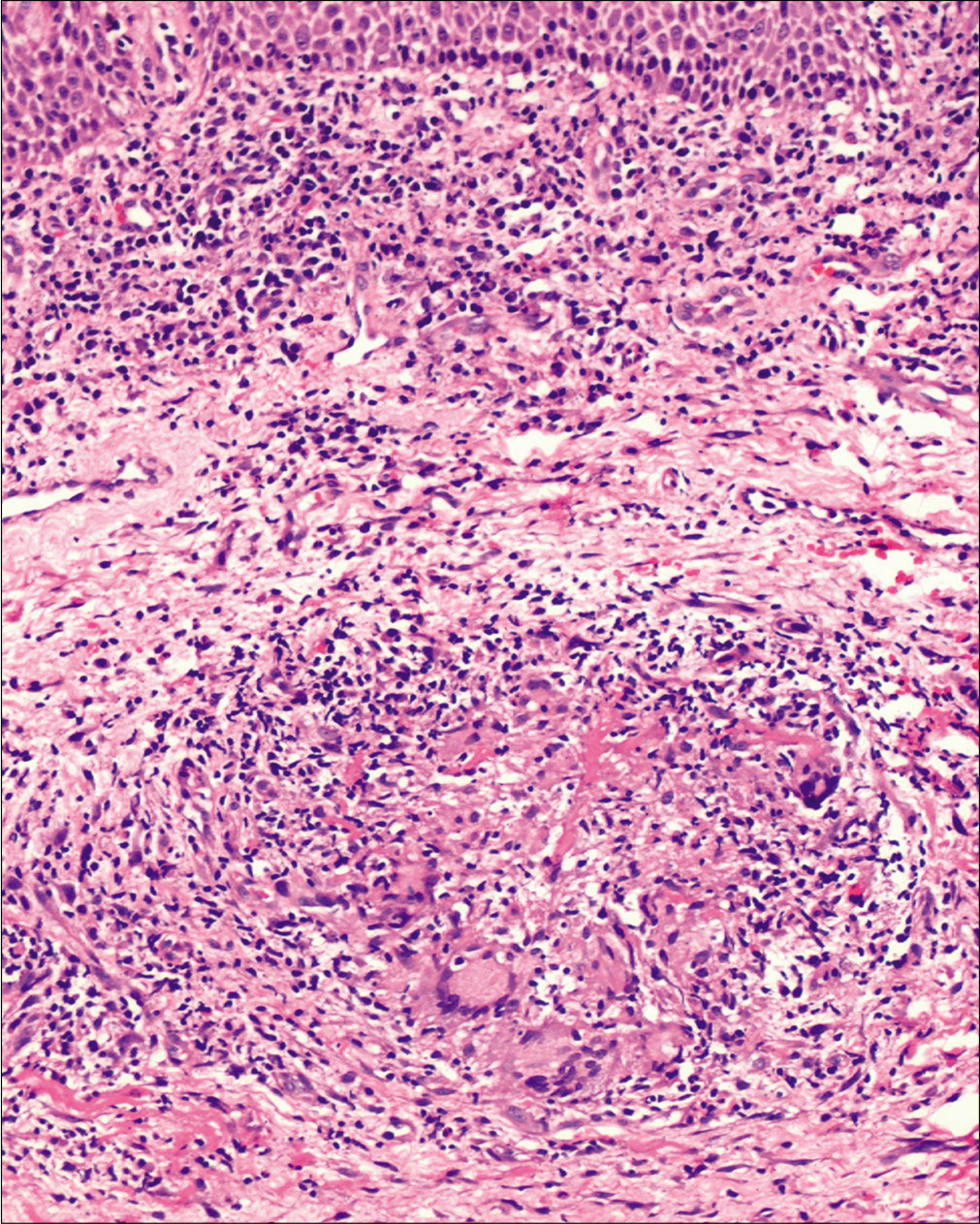
- Epithelioid granuloma with giant cells surrounded by lymphocytes (hematoxylin and eosin, ×400)

- Healed ulcero-proliferative gingivitis following antitubercular therapy
India accounts for one-third of the World’s Mycobacterium tuberculosis infection. With the emergence of the HIV epidemic and the use of various immunosuppressive drugs, the incidence of extrapulmonary tuberculosis is on the rise. Tuberculosis of the oral cavity is relatively rare, accounting for 0.1–5% of extrapulmonary tuberculosis. 1 Despite frequent exposure, the oral cavity is less prone to mycobacterial colonization, probably because of the protective nature of saliva, presence of saprophytes, thick covering epithelium and resistance of striated muscle to bacterial invasion. Factors such as poor oral hygiene, local trauma, irritation, oral leukoplakia and dental extraction may predispose to oral tuberculosis. Besides, the virulence of Mycobacterium tuberculosis and HIV coinfection are other predisposing factors for oral involvement. Oral tuberculosis can be either primary or secondary. The tongue is the most frequent site of involvement. Other common sites involved are palate and buccal mucosa. Besides ulcer, other morphological presentations are erosion, patch, nodule, plaque, vesicles, tuberculoma, fissures, periapical granuloma or lesions within jaw.1-4 Primary lesions are relatively uncommon and characterized by a solitary painless ulcer with regional lymphadenopathy. Children and adolescents are affected more than adults. The common sites are gingiva, buccal folds or near sites of tooth extraction.5,6 The more common secondary form is usually associated with pulmonary disease and presents with a slowly enlarging irregular, painful ulcer with minimal induration. The base may be granular or covered with pseudomembrane. Middle-aged and older people are commonly affected. The dorsum of the tongue is the frequently involved site, followed by the palate, buccal mucosa and lips.5,6 Although, in our case, all the investigations for identifying an underlying focus of tuberculosis was negative, the following findings suggest the lesion be secondary to hidden active focus or healed disease rather than primary; late onset of the disease in an endemic country like India, immunocompetent adult, lack of history of prior trauma or dental procedure and absence of regional lymphadenopathy. Gingival involvement, especially ulceration, in tuberculosis, is rare. Besides, at times the presentation can be nonspecific, like diffuse erythematous papillary or nodular lesion, marginal periodontitis, diffuse gingival enlargement with loss of teeth and can be modified due to immunosuppression.4 In this case, the patient was immunocompetent and presented with ulcero-proliferative gingivitis that remained undiagnosed for nearly 10 months.
Diagnosis of gingival tuberculosis is challenging for a dermatologist as many mucosal disorders such as pemphigus, erosive lichen planus, mucous membrane pemphigoid, Crohn’s disease and Wegner’s granulomatosis may present with similar morphology. Strawberry gingivitis is a well-known presentation of Wegner’s granulomatosis, while Crohn’s disease may present with gingival cobblestoning, pustules, erosion, “snail-track” ulcers and hypertrophy.5,6 In both of the above conditions, the gingivitis may be an initial manifestation, preceding the systemic features. Other mimickers are aphthous ulcer, traumatic ulcer, syphilitic ulcer, actinomycosis, deep fungal infection, sarcoidosis, orofacial granulomatosis, drug-induced hypertrophy, leukemic infiltrate and Kaposi’s sarcoma.7-10
A definitive diagnosis mandates a deep mucosal biopsy to demonstrate epithelioid granuloma. Demonstration of acid-fast bacilli may not be feasible due to the relative paucity of bacilli. A superficial biopsy may fail to aid diagnosis due to epithelial hyperplasia. At times multiple biopsies may be required to prove the diagnosis.1 Although not widely available in India, a gene Xpert Mycobacterium tuberculosis/ rifampicin assay may help in the rapid diagnosis of the condition as in our case.
In conclusion, in endemic countries like India, a differential diagnosis of tuberculosis should be considered in patients with therapy-resistant gingivitis. A detailed clinical examination, along with histopathology, will provide a clue to this treatable condition.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal the identity but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Oral manifestations of tuberculosis: Step towards early diagnosis. J Clin Diagn Res. 2014;8:ZE18-21.
- [CrossRef] [PubMed] [Google Scholar]
- Primary gingival tuberculosis diagnosis: A difficult endeavor. J Contemp Dent Pract. 2013;14:137-9.
- [CrossRef] [PubMed] [Google Scholar]
- Extrapulmonary tuberculosis: Atypical presentation in otorhinolaryngology. BMJ Case Rep. 2018;2018:bcr2018224802?.
- [CrossRef] [PubMed] [Google Scholar]
- Orofacial tuberculosis: Clinical manifestations, diagnosis and management. J Fam Med Prim Care. 2015;4:335-41.
- [CrossRef] [PubMed] [Google Scholar]
- Oral mucosal ulceration: A manifestation of previously undiagnosed pulmonary tuberculosis. J Am Dent Assoc. 2004;135:336-40.
- [CrossRef] [PubMed] [Google Scholar]
- Primary oral tuberculosis. BMJ Case Rep. 2013;2013:bcr2013010276.
- [CrossRef] [PubMed] [Google Scholar]
- Strawberry gingivitis as the first presenting sign of Wegener's granulomatosis: Report of a case. Eur J Med Res. 2011;16:331-4.
- [CrossRef] [PubMed] [Google Scholar]
- Gingival involvement in Crohn disease. J Am Dent Assoc. 2007;138:1574-81.
- [CrossRef] [PubMed] [Google Scholar]
- Gingival manifestations of orofacial granulomatosis. Arch Dermatol. 2008;144:1627-30.
- [CrossRef] [PubMed] [Google Scholar]
- Sarcoidosis presenting as isolated gingival enlargement: A rare case entity. J Clin Diagn Res. 2014;8:ZD25-6.
- [CrossRef] [PubMed] [Google Scholar]





