Translate this page into:
Fox-Fordyce disease: A report of 2 cases responding to topical clindamycin
Correspondence Address:
Anisha George
Department of Dermatology, Christian Medical College, Ludhiana - 141 008, Punjab
India
| How to cite this article: George A, Bhatia A, Thomas E. Fox-Fordyce disease: A report of 2 cases responding to topical clindamycin. Indian J Dermatol Venereol Leprol 2015;81:87-88 |
Sir,
A 15-year-old girl presented with a history of severely itchy persistent lesions under the arms and on the breasts for 2 years; and over the pubic region for 3 months. She was found to have faint erythematous to skin-colored, 2-3 mm sized, firm, smooth, dome-shaped, grouped, yet equidistant papules over the axillae, areolae [Figure - 1] and mons pubis. She also had decreased hair growth over the axillae and mons pubis. The surrounding skin was normal. A clinical diagnosis of Fox-Fordyce disease was made, and she was given topical clindamycin to be applied twice a day, with which, within 2 months she had remarkable improvement.
 |
| Figure 1: Skin colored papules over the left areola |
The second patient was a 22-year-old lady, who presented with itchy lesions over the skin of the axilla for 6 years. Itching was worse in summers. She had no family history of similar disease. Cutaneous examination revealed skin-colored papules throughout the axillae with no terminal hair growth [Figure - 2]. She was initially treated with topical tretinoin, with no response; after which topical clindamycin twice daily was given, with which the lesions reduced.
 |
| Figure 2: Monomorphic papules over the right axilla with no terminal hair growth |
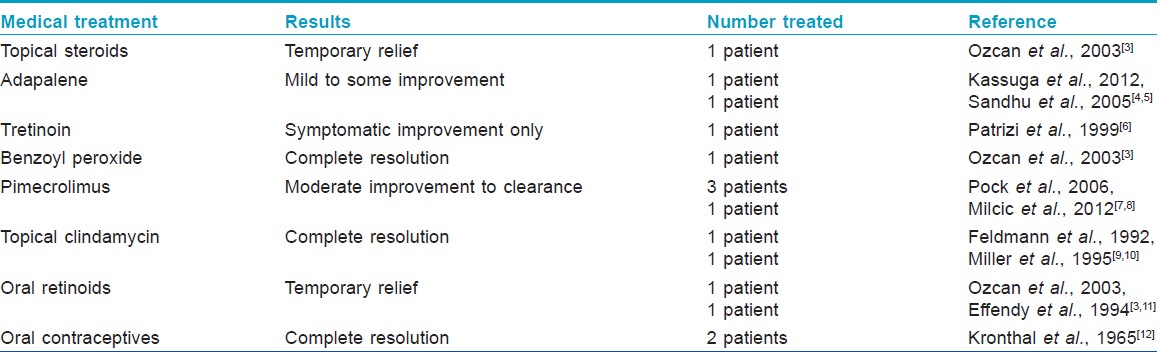
Fox-Fordyce disease, also known as apocrine miliaria, is a rare condition seen in adolescent women, over the apocrine gland-bearing areas like the axillae, groin, areolae and inframammary creases in decreasing order of frequency. It is a chronic, treatment-resistant disorder with characteristic clinical features and non-specific histopathological features. The pathogenesis of this condition, initially thought to be due to hyperkeratosis, was subsequently shown to be caused by detached apo-eccrine secretory cells obstructing the intraepidermal apo-eccrine sweat ducts. [1] The only diagnostic feature, i.e., the "intraepidermal sweat retention vesicle" [2] is rarely seen. Clinical and differential diagnoses which can be considered include Graham-Little-Picardi-Lasseur syndrome and trichostasis spinulosa; however, our patients did not have cicatricial alopecia or lesions elsewhere on the body or mucosa. The lesions in trichostasis spinulosa are usually non-pruritic. Medical therapies reported to have been used in Fox- Fordyce disease are listed in the table [Table - 1]. The mechanism of action of clindamycin in this disease is unknown.
Lasers, including fractional CO2 laser, [13] have been used for recalcitrant lesions with a remarkable response in 3 months. However, lasers for axillary hair removal have been shown to induce Fox-Fordyce disease. [14] Surgical intervention is a definitive treatment and includes areolar dermal detachment safeguarding the nipple, apocrine sweat gland excision and fixation of the areola like a flap. [15]
| 1. |
Kamada A, Saga K, Jimbow K. Apoeccrine sweat duct obstruction as a cause for Fox-Fordyce disease. J Am Acad Dermatol 2003;48:453-5.
[Google Scholar]
|
| 2. |
Böer A. Patterns histopathologic of Fox-Fordyce disease. Am J Dermatopathol 2004;26:482-92.
[Google Scholar]
|
| 3. |
Ozcan A, Senol M, Aydin NE, Karaca S, Sener S. Fox-Fordyce disease. J Eur Acad Dermatol Venereol 2003;17:244-5.
[Google Scholar]
|
| 4. |
Kassuga LE, Medrado MM, Chevrand NS, Salles Sde A, Vilar EG. Fox-Fordyce disease: Response to adapalene 0.1%. An Bras Dermatol 2012;87:329-31.
[Google Scholar]
|
| 5. |
Sandhu K, Gupta S, Kanwar AJ. Fox fordyce disease in a prepubertal girl. Pediatr Dermatol 2005;22:89-90.
[Google Scholar]
|
| 6. |
Patrizi A, Orlandi C, Neri I, Fanti PA, Mazzanti L. Fox-Fordyce disease: Two cases in patients with Turner syndrome. Acta Derm Venereol 1999;79:83-4.
[Google Scholar]
|
| 7. |
Pock L, �vrèková M, Macháèková R, Hercogová J. Pimecrolimus is effective in Fox-Fordyce disease. Int J Dermatol 2006;45:1134-5.
[Google Scholar]
|
| 8. |
Milcic D, Nikolic M. Clinical effects of topical pimecrolimus in a patient with Fox-Fordyce disease. Australas J Dermatol 2012;53:e34-5.
[Google Scholar]
|
| 9. |
Feldmann R, Masouyé I, Chavaz P, Saurat JH. Fox-Fordyce disease: Successful treatment with topical clindamycin in alcoholic propylene glycol solution. Dermatology 1992;184:310-3.
[Google Scholar]
|
| 10. |
Miller ML, Harford RR, Yeager JK. Fox-Fordyce disease treated with topical clindamycin solution. Arch Dermatol 1995;131:1112-3.
[Google Scholar]
|
| 11. |
Effendy I, Ossowski B, Happle R. Fox-Fordyce disease in a male patient--response to oral retinoid treatment. Clin Exp Dermatol 1994;19:67-9.
[Google Scholar]
|
| 12. |
Kronthal HL, Pomeranz JR, Sitomer G. Fox-Fordyce disease: Treatment with an oral contraceptive. Arch Dermatol 1965;91:243-5.
[Google Scholar]
|
| 13. |
Ahmed Al-Qarqaz F, Al-Shannag R. Fox-Fordyce disease treatment with fractional CO2 laser. Int J Dermatol 2013;52:1571-2.
[Google Scholar]
|
| 14. |
Tetzlaff MT, Evans K, DeHoratius DM, Weiss R, Cotsarelis G, Elenitsas R. Fox-Fordyce disease following axillary laser hair removal. Arch Dermatol 2011;147:573-6.
[Google Scholar]
|
| 15. |
Chavoin JP, Charasson T, Bernard JD. Surgical treatment of hidradenitis and Fox-Fordyce disease of the nipples. Ann Chir Plast Esthet 1994;39:233-8.
[Google Scholar]
|
Fulltext Views
7,210
PDF downloads
2,474





