Translate this page into:
Frontal fibrosing alopecia and lichen planopilaris in HLA-identical mother and daughter
2 Department of Immunology, Complejo Asistencial Universitario de Le�n, Spain
Correspondence Address:
Mar�a Mercedes Otero Rivas
Department of Dermatology, Complejo Asistencial, Universitario de Le�n, C/Altos de Nava sn CP: 24071 Le�n
Spain
| How to cite this article: Rivas MO, Antol�n SC, Sambucety PS, Gonz�lez ES, Ru�z de Morales JG, Prieto MR. Frontal fibrosing alopecia and lichen planopilaris in HLA-identical mother and daughter. Indian J Dermatol Venereol Leprol 2015;81:162-165 |
Abstract
Frontal fibrosing alopecia (FFA) is a lymphocyte-mediated scarring alopecia thought to be a variant of lichen planopilaris (LPP). We present a 67-year-old woman with frontal fibrosing alopecia whose daughter was diagnosed to have lichen planopilaris. Both patients had identical human leukocyte antigen (HLA) D types, supporting a phenotypical relationship between the two clinical entities. Interestingly, our patient also had of autoimmune chronic atrophic gastritis, a previously unreported association.INTRODUCTION
Frontal fibrosing alopecia (FFA), first described in 1994 by Kossard, [1] is considered a clinical variant of lichen planopilaris (LPP). Only seven familial cases have been reported, [2] in contrast with familial lichen planus, in which several pedigrees have been described. Here, we report a mother and a daughter, affected by two related but distinct types of lymphocyte-mediated scarring alopecia: classic lichen planopilaris and frontal fibrosing alopecia.
Case Report
A 67-year-old female with a history of diabetes mellitus, hyperlipidemia, and hypertension presented to our clinic with fronto-temporal hair loss. She was receiving treatment with atorvastatin, metformin, and candesartan cilexetil. Upon examination, there was decreased hair density in a male pattern and a complete loss of hair in the frontal area. The affected frontal scalp was smooth and shiny without evidence of follicular ostia. Some visible hair follicles were surrounded by a halo of erythema and scaling. A hair pull test was negative. There was slight sparsening of the eyebrows. The rest of the physical examination was completely normal; no facial papules were noted. Body hair and oral and genital mucosae were normal. Dermoscopy of the affected scalp revealed markedly reduced follicular ostia, erythema, and perifollicular blue-gray dots [Figure - 1]. A diagnosis of female androgenetic alopecia Ludwig grade II and frontal fibrosing alopecia was made. Skin biopsy showed that follicular units were diminished in number with presence of some fibrous tracts. This was accompanied by a moderately dense lymphocytic inflammatory infiltrate surrounding the follicular infundibulum and destroying the outer root sheaths of the upper part of the follicles [Figure - 2]. She was treated with 5% minoxidil twice daily and a compound preparation of 0.025% retinoic acid with 0.05% bethametasone dipropionate in oil/water for nightly application on the fronto-temporal hairline with moderate results, stopping partially the spread of disease.
 |
| Figure 1: (a) Frontal hair loss with subtle scale of the remaining hairs (b) Temporal hair loss (c) Dermoscopy showed reduced follicular ostia and erythema |
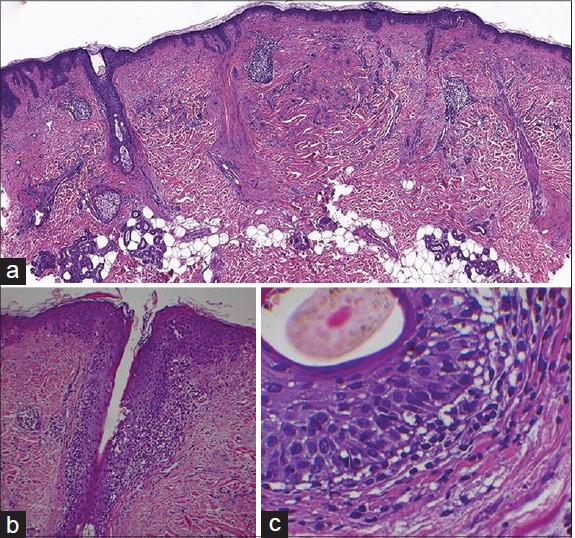 |
| Figure 2: (a) Loss of follicular units and fibrous tracts (H and E, x 0) (b) Inflammatory infiltrate composed of lymphocytes surrounding a hair follicle with damage of the epithelium (H and E, x100) (c) Lymphocytes destroying the outer root sheath of the hair follicle (H and E, x400) |
The patient′s 38-year-old daughter presented a few weeks later with small parieto-occipital patches of alopecia. Hair pull test was negative in the surrounding hair. On examination, the patient had a patch of cicatricial alopecia with fine scaling. [Figure - 3] Some hyperkeratosis was appreciated in some follicles at the edges of the patches. Pubic and axillary hair were normal and oral and genital mucosae were unaffected.
 |
| Figure 3:(a) Interparietal patches of alopecia (b) Dermoscopy revealed erythema of the follicular ostia (c) Note the cicatricial aspect of the scalp |
On histopathologic examination, the hair follicles were replaced with fibrous tracts with some laminated fibrotic rims around them. A sparse lymphocytic infiltrate could be appreciated around the infundibulum and the isthmus [Figure - 4]. A diagnosis of lichen planopilaris in a late stage, resembling pseudopelade, was made. Topical therapy with 0.1% tacrolimus ointment twice daily was prescribed with minimal improvement.
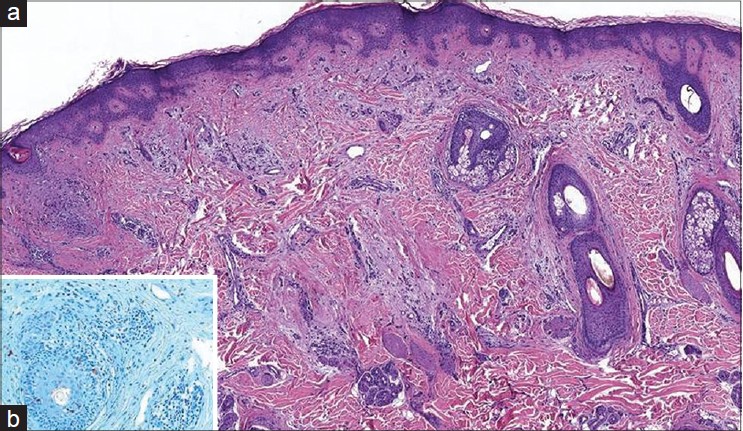 |
| Figure 4: (a) Fibrous tracts replacing ancient hair follicles Some fibrotic tissue can be observed around them admixed with a sparse lymphocytic infiltrate (H and E, x40) (b) Lymphocytic infiltrate localized around the upper portion of the hair follicle causing vacuolar interface changes (Alcian Blue, x100; transverse section) |
To determine if there was any HLA association in this family, similar to that previously reported in familial lichen planus, HLA studies were performed. Using sequence-specific polymerase chain reaction (PCR) primers, HLA DRB1FNx0104,13 and DQB1FNx0103:02,06 were identified in both the patients. This finding of two first degree relatives with the same HLA type, but different expression of two subtypes of lymphocytic scarring alopecia, is novel.
Additional studies including complete blood cell count, hepatic, renal, and iron metabolism profiles were normal. The mother revealed positive antiparietal gastric cell antibodies in a titre of 1:640 as well as reduced levels of vitamin B12 (142 pg/ml). Gastroscopy revealed a mucosal pattern that suggested chronic atrophic gastritis, which was subsequently confirmed histologically. She received injectable intramuscular cyanocobalamin. The daughter did not have any of these laboratory abnormalities.
Discussion
Frontal fibrosing alopecia (FFA) is a form of cicatricial alopecia with a distinctive clinical presentation, that has shown increased prevalence since it was first reported in 1994. [1] It is commonly accepted as a variant of lichen planopilaris, based on shared features in clinical appearance and histopathology. [3] Another lichen planopilaris variant, Piccardi-Lassueur-Graham-Little syndrome (PLGLS), is characterized by widespread follicular keratotic papules on the limbs and trunk and hair loss involving pubic hair, axillary hair, and the eyebrows. A spectrum of patients present with overlapping features of frontal fibrosing alopecia and Piccardi-Lassueur-Graham-Little syndrome [4] and some familial cases of both entities have been reported. [2],[5] Patients with frontal fibrosing alopecia with skin and/or mucosal lesions have been described in the literature, and total or partial eyebrow loss has become a prominently reported feature since the initial report. [3] Hair follicle loss in the body and face is part of the same fibrotic process involving the scalp, so frontal fibrosing alopecia could represent a clinical variant of lichen planopilaris localized to certain areas because of unknown factors. Interestingly, although up to 50% of cases of lichen planopilaris are associated with mucosal lesions, frontal fibrosing alopecia is rarely reported with these. [6]
The reason for selective involvement of intermediate and vellus-like follicles of the frontal margin and the eyebrows is unknown. Frontal fibrosing alopecia may represent a variety of lichen planopilaris with selective involvement of certain androgen-dependent areas. The effectiveness of finasteride to arrest the disease progression in some patients, and the predominance of the disease in postmenopausal women, may imply a hormonal basis for frontal fibrosing alopecia. [7]
Some reports indicate that the epidemiology of frontal fibrosing alopecia strongly suggests a role for environmental factors, and the occurrence in families may simply indicate exposure to common triggers such as dioxine-like chemicals. [2] Withdrawal of candersartan or atorvastatin was not attempted for our patient, as there is a lack of evidence regarding drug involvement in frontal fibrosing alopecia, and they were part of treatment for metabolic syndrome.
Association of autoimmune diseases with frontal fibrosing alopecia is rare with scarce reports of connective tissue disease and higher frequency of serum autoantibodies such as antinuclear antibodies. [7] Higher frequencies of serum autoantibodies have been detected in patients with oral lichen planus. [8] Thyroid dysfunction and vitiligo are more frequently associated with frontal fibrosing alopecia. [9] We were unable to find any previous reports of atrophic gastritis with positive antiparietal gastric cell antibodies in a patient with frontal fibrosing alopecia. Whether these two immune-mediated diseases are related or if it is merely coincidental is unknown to date and more studies should be performed.
Lichen planopilaris was initially described by Pringle in 1895, and is considered to be the most frequent cause of adult primary scarring alopecia. The classical form commonly involves the vertex, but any region of the scalp can be affected. Typical papules of lichen planus are not observed in the scalp. Frontal fibrosing alopecia and lichen planopilaris cannot be differentiated on histologic or immunohistochemical criteria. [10] Both disorders show an inflammatory lymphocytic infiltrate involving the isthmus and infundibulum of the hair follicles, with some apoptotic cells and concentric fibrosis around the hair follicles, as noted in our case.
Familial lichen planus is uncommon, the prevalence has been reported to be 1.5% [11] and 28 pedigrees have been reported. [12] Copeman et al. [13] found an association of HLA-B7 in familial cases but not in sporadic cases. Other associations include HLA-DR1, which seems to be correlated with peptide anchorage and presentation of specific T helper lymphocytes. [14] HLA testing revealed HLA DRB1FNx01(04,13), DQB1FNx01(03:02,06) in both patients, supporting the idea that these diseases may share a common genetic predisposition, and may represent different clinical variants probably influenced by environmental or hormonal factors.
| 1. |
Kossard S. Post-menopausal frontal fibrosing alopecia: Scarring alopecia in a pattern distribution. Arch Dermatol 1994;130:770-4.
[Google Scholar]
|
| 2. |
Dlova N, Goh CL, Tosti A. Familial frontal fibrosing alopecia. Br J Dermatol 2012;168:220-2.
[Google Scholar]
|
| 3. |
Kossard S, Lee MS, Wilkinson B. Postmenopausal frontal fibrosing alopecia: A frontal variant of lichen planopilaris. J Am Acad Dermatol 1997;36:59-66.
[Google Scholar]
|
| 4. |
Abbas O, Chedraoui A, Ghosn S. Frontal fibrosing alopecia presenting with components of Piccardi-Lassueur-Graham-Little syndrome. J Am Acad Dermatol 2007;57 Suppl 2:S15-8.
[Google Scholar]
|
| 5. |
Viglizzo G, Verrini A, Rongioletti F. Familial Lassueur-Graham-Little-Picardi syndrome. Dermatology 2004;208:142-4.
[Google Scholar]
|
| 6. |
Chew AL, Bashir SJ, Wain EM, Fenton DA, Stefanato CM. Expanding the spectrum of frontal fibrosing alopecia: A unifying concept. J Am Acad Dermatol 2010;63:653-60.
[Google Scholar]
|
| 7. |
Tosti A, Piraccini BM, Iorizzo M, Misciali C. Frontal fibrosing alopecia in postmenopausal women. J Am Acad Dermatol 2005;52:55-60.
[Google Scholar]
|
| 8. |
Chang JY, Chiang CP, Hsiao CK, Sun A. Significantly higher frequencies of presence of serum autoantibodies in Chinese patients with oral lichen planus. J Oral Pathol Med 2009;38:48-54.
[Google Scholar]
|
| 9. |
Vañó-Galván S, Molina-Ruiz AM, Serrano-Falcón C, Arias-Santiago S, Rodrigues-Barata AR, Garnacho-Saucedo G, et al. Frontal fibrosing alopecia: A multicenter review of 355 patients. J Am Acad Dermatol 2014;70:670-8.
[Google Scholar]
|
| 10. |
Poblet E, Jiménez F, Pascual A, Piqué E. Frontal fibrosing alopecia versus lichen planopilaris: A clinicopathological study. Int J Dermatol 2006;45:375-80.
[Google Scholar]
|
| 11. |
Altman J, Perry HO. The variations and course of lichen planus. Arch Dermatol 1961;84:179-91.
[Google Scholar]
|
| 12. |
Singal A. Familial mucosal lichen planus in three successive generations. Int J Dermatol 2005;44:81-2.
[Google Scholar]
|
| 13. |
Copeman PW, Tan RS, Timlin D, Samman PD. Familial lichen planus. Another disease or distinct people? Br J Dermatol 1978;98:573-7.
[Google Scholar]
|
| 14. |
Katzenelson V, Lotem M, Sandbank M. Familial lichen planus. Dermatologica 1990;180:166-8.
[Google Scholar]
|
Fulltext Views
6,843
PDF downloads
2,424





