Translate this page into:
Fuchs syndrome or erythema multiforme major, uncommon or underdiagnosed?
2 Department of Pathology, Postgraduate Institute of Medical Education and Research, Chandigarh, India
Correspondence Address:
Muthu Sendhil Kumaran
Assistant Professor, Department of Dermatology, PGIMER, Chandigarh
India
| How to cite this article: Mangal S, Narang T, Saikia UN, Kumaran MS. Fuchs syndrome or erythema multiforme major, uncommon or underdiagnosed?. Indian J Dermatol Venereol Leprol 2015;81:403-405 |
Sir,
Fuchs syndrome, initially described by the Germans, is mucositis associated with Mycoplasma pneumonia (M. pneumoniae). Various terminologies like incomplete Steven-Johnson syndrome (SJS), atypical SJS, or erythema multiforme major are also used to describe the same condition. [1] Although the condition is not uncommon, it is either under-evaluated or under-reported. We were unable to find many previous reports of the condition.
A 12-year-old schoolboy presented with a 6-day history of fever along with crusted and swollen lips. Two weeks ago, he developed cough, sore throat, and high grade fever and received oral amoxycyllin and clavulanic acid combination for 4 days from private practitioners without much improvement. Four days later, there was soreness over lips followed by erosions and crusting. Mucositis worsened despite stopping antibiotics and he was unable to eat. Initially, he was treated with acyclovir with a suspicion of herpetic stomatitis. He was not known to be allergic to amoxycllin-clavulanic acid and had received multiple doses of the tablets in the past. There was no history of collagen vascular disease.
Clinically, the patient was febrile (39.8°C), dehydrated, and had swollen lips with hemorrhagic crusting [Figure - 1]. Conjunctival congestion and multiple erosions over soft palate were present. Skin and genitalia were unaffected. There was no cervical lymphadenopathy. Tzanck smear from erosions did not show acantholytic or giant cells. Routine laboratory investigations including chest radiography were normal except for raised erythrocyte sedimentation rate (55 mm; 1 h). Serological investigations for herpes simplex virus (type 1 and 2) were negative; however, IgM for M. pneumoniae was positive on serology and immunoblotting. Also, M. pneumoniae was detected from throat swab by polymerase chain reaction (PCR). Oral mucosal biopsy showed mixed dermal inflammatory infiltrate with apoptotic epithelial cells suggestive of erythema multiforme [Figure - 2]. Ophthalmology consultation suggested changes of early Steven Johnson syndrome. The patient was started on oral azithromycin (10 mg/kg/day) for 5 days along with supportive therapy which resulted in substantial improvement.
 |
| Figure 1: Hemorrhagic crusting of the lips with erosions over hard palate |
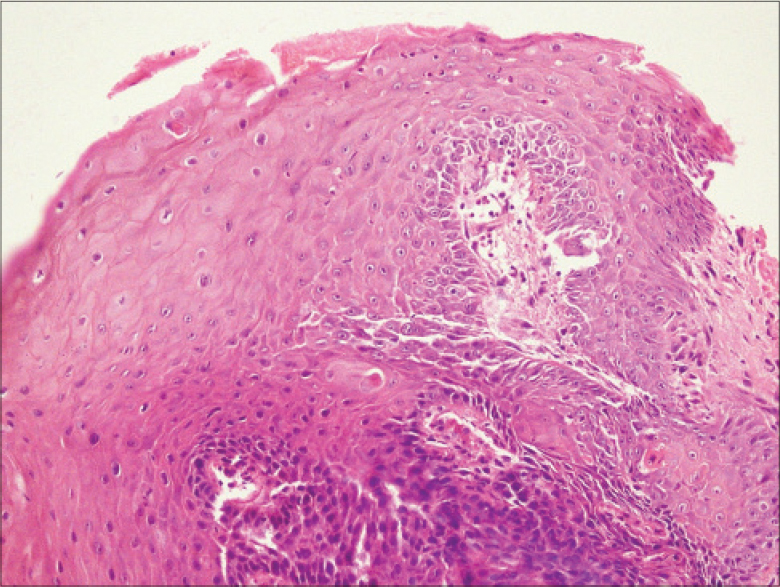 |
| Figure 2: Microphotograph showing apoptotic keratinocytes in epidermis along with mixed inflammation in the dermis and edema of basal layer on H and E (20×) |
Steven Johnson syndrome with mucosal involvement in the absence of skin lesions has been described as Fuchs syndrome and is believed to be a variant of erythema multiforme major. Mucositis with fever is commonly seen and in the majority of the cases, it is treated as herpetic stomatitis or incomplete Steven Johnson syndrome or erythema multiforme, with acyclovir or steroids, without adequate work up to identify the cause.
Fuchs syndrome has been described more frequently in children and adolescents, [2] although adult cases have been reported. [3] Most cases are triggered by infections, herpes simplex and M. pneumoniae being the most common. According to a retrospective analysis, M. pneumoniae seems to be the most frequent infectious cause in children. [4]
M. pneumoniae may cause the condition with or without cutaneous involvement. [5] Even in the presence of cutaneous involvement, mucosal lesions predominate. Oral mucosa is almost always affected. Ocular and genital lesions occur in two-thirds and three-fourths of the cases, respectively. In the absence of classic targetoid skin lesions, it is likely that the correct diagnosis is missed and appropriate therapy delayed. In our patient, apart from oral and conjunctival lesions, the rest of the examination was unremarkable.
In most cases, the diagnosis of M. pneumoniae in Fuchs syndrome has been made by serology in the absence of significant radiological changes. Treatment consists of antibiotics such as macrolides (especially clarithromycin and azithromycin), quinolones, and tetracyclines (except in children younger than 8 years) along with supportive therapy. Our patient showed considerable improvement with azithromycin.
We found only a few previous reports of severe M. pneumoniae-associated mucositis in the absence of skin lesions. [1],[5] We suggest that severe mucositis in the background of respiratory illness should prompt consideration for M. pneumoniae as a potential causative agent. Confirmation by serology or polymerase chain reaction is useful. The prognosis is excellent with timely management. It is probably under-reported or under-diagnosed due to lack of consensus on the diagnostic label used to describe this condition and usage of multiple terminologies adds to the confusion. We believe the term erythema multiforme major is sufficient to describe the condition.
| 1. |
Latsch K, Girschick HJ, Abele-Horn M. Stevens-Johnson syndrome without skin lesions. J Med Microbiol 2008;56:1696-9.
[Google Scholar]
|
| 2. |
Ravin KA, Rappaport LD, Zuckerbraun NS, Wadowsky RM, Wald ER, Michaels MM. Mycoplasma pneumoniae and atypical Stevens-Johnson syndrome: A case series. Pediatrics 2007;119:e1002-5.
[Google Scholar]
|
| 3. |
Li K, Haber RM. Stevens-Johnson syndrome without skin lesions (Fuchs Syndrome): A literature review of adult cases with mycoplasma cause. Arch Dermatol 2012;148:963-4.
[Google Scholar]
|
| 4. |
Havliza K, Jakob A, Rompel R. Erythema multiforme majus (Fuchs syndrome) associated with Mycoplasma pneumoniae infection in two patients. J Dtsch Dermatol Ges 2009;7:445-8.
[Google Scholar]
|
| 5. |
Meyer Sauteur PM, Gansser-Kälin U, Lautenschlager S, Goetschel P. Fuchs syndrome associated with Mycoplasma pneumoniae (Stevens- Johnson syndrome without skin lesions. Pediatr Dermatol 2011;28:474-6.
[Google Scholar]
|
Fulltext Views
7,170
PDF downloads
3,243





