Translate this page into:
Functional esthetic rehabilitation of a 7-year-female patient with hereditary ectodermal dysplasia using flexible denture
2 Department of Oral Medicine and Radiology, VSPM Dental College and Research Centre, Nagpur, Maharashtra, India
Correspondence Address:
Ritesh Kalaskar
Plot No. 68, Banerjee Layout, Bhagwan Nagar Road, Nagpur - 440 027, Maharashtra
India
| How to cite this article: Kalaskar R, Kalaskar A. Functional esthetic rehabilitation of a 7-year-female patient with hereditary ectodermal dysplasia using flexible denture. Indian J Dermatol Venereol Leprol 2013;79:826-827 |
Sir,
Hypohidrotic ectodermal dysplasia (HED) is a congenital syndrome characterized by sparse hair, oligodontia and reduced sweating. [1] It is caused by mutation in the ectodysplasin A gene, which is inherited as X linked recessive pattern. However, less commonly HED is also caused by mutation in ectodysplasin-A receptor or EDARADD gene, which has an autosomal dominant or autosomal recessive pattern of inheritance. [2],[3] Expression of symptoms are fully blown in affected males, but females are usually carrier. [2],[3] Dental manifestations include conical or pegged shaped teeth, hypodontia or complete anodontia, delayed eruption of permanent teeth, thin alveolus ridge and dry oral mucous membrane. [1] Children with HED have problems with mastication, speech, esthetic and psychology: Affecting their quality of life. [1] To restore the lost functions and to improve self-confidence removable partial denture, complete denture, implant supported complete denture and over denture can be given. [3] We hereby, describe the oral management of a female child with HED using the flexible over denture.
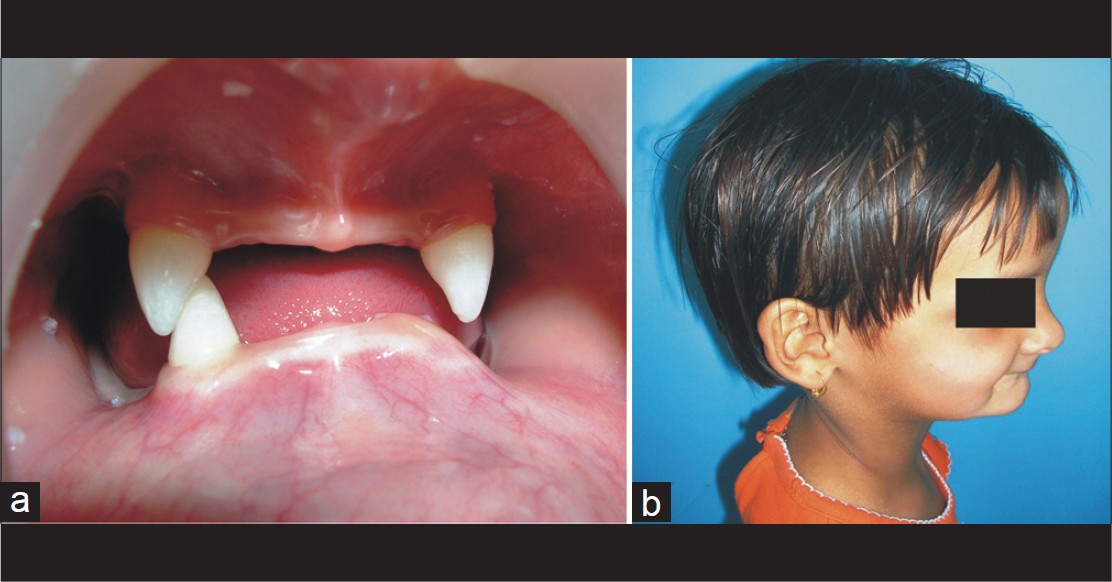 |
| Figure 1: (a) Intra-oral photograph showing oligodontia and cone shaped teeth. (b) Clinical photograph showing dysmorphic facial features |
A 7-year-old girl with HED reported with the complaint of inability to masticate, unesthetic appearance and teasing from her peer group. Patient gave a history of decreased sweating, dry oral mucosa and skin and raised body temperature. She was born of a normal delivery and her psychomotor development was normal. Patient′s family history revealed that the mother′s cousin brothers had similar problems. Intra-oral examination revealed dry oral mucosa, conical shaped teeth, oligodontia and thin alveolar ridges [Figure - 1]. Extra-oral examination showed sparse hair, frontal bossing, depressed nasal bridge, sunken cheeks and everted lips [Figure - 1]. Nails appeared normal. Systemic examinations were within the normal limit. Based on history and clinical examination a diagnosis of HED was made. At the age of 7 years, skeletal maturity is incomplete hence flexible removable over dentures were given to reestablish occlusion, mastication, speech and esthetic [Figure - 2]. Primary impressions of both jaws were made with irreversible hydrocolloid impression material. Custom trays were prepared and border molding was carried out with a heavy body polyvinyl siloxane material. The final impressions were made with medium and light body type of rubber base impression material. Maxillo-mandibular relation was recorded and teeth were arranged according to a balanced occlusal scheme. Maxillary and mandibular prostheses were fabricated in Valplast resin by injection molding technique. Prior to insertion, the valplast partial denture was immersed for a minute in warm water. The heat exposure assures a very smooth initial insertion and allows the denture to adapt to the underlying tissue. The dentures were then inserted in patient′s mouth [Figure - 2]. Patient was educated about proper insertion, removal and hygiene of the over denture. Future visits were scheduled for 6 months to monitor bone growth and for denture relining.
 |
| Figure 2: Extra-oral photograph showing denture in place |
Oral care: As there are many oral manifestations, there is no standard formula for dental treatment. Treatment needs may include: Preventive measures against caries, restorations of decayed teeth, partial dentures, over dentures, implant supported denture and timely orthodontic care. In the present case, the child was given flexible removable partial denture. The advantage of flexible partial denture: Improved esthetic, exceptionally strong and flexible, good biocompatibility, free from an allergic reaction, does not irritate the oral mucosa and satisfy daily diet for the child. [4] Implant supported complete denture is avoided until adolescence because of increased risk of implant failure due to insufficient alveolar bone support. Secondly, there is a risk of trauma to tooth germs and interferences in craniofacial growth. [5]
Orthodontic care is one of the major concerns of families with children affected with HED. Because early orthodontic care in such children not only improves alignment of permanent teeth, but also improves facial profile and prevent psychological trauma associated with this condition. Orthodontic treatment using flexible dentures can enhance growth process, maintain favorable maxillomandibular relations and provide a permanent base for prosthetic rehabilitation. This type of combination treatment ultimately benefits stomatognathic function, vertical growth and enhance the facial appearance and profile. In a recent case, authors have incorporated midline jackscrew in removing partial denture to enhance transverse growth and closure of midline diastema. [5] However, combine delivery of orthodontic and prosthodontic treatment can lead to design compromise leading to compromised functional stability. Therefore, such patients require close attention and require frequent replacement of prosthesis.
Patient and parents should be made aware of the importance of denture hygiene maintenance, use of fluoride mouth rinses, application of lubricant to avoid drying, cracking of the oral mucosa and periodic modification in dentures due to growth changes. Individuals are advised to take frequent sip of water through the day.
| 1. |
Bashyam MD, Chaudhary AK, Reddy EC, Reddy V, Acharya V, Nagarajaram HA, et al. A founder ectodysplasin A receptor (EDAR) mutation results in a high frequency of the autosomal recessive form of hypohidrotic ectodermal dysplasia in India. Br J Dermatol 2012;166:819-29.
[Google Scholar]
|
| 2. |
Cluzeau C, Hadj-Rabia S, Jambou M, Mansour S, Guigue P, Masmoudi S, et al. Only four genes (EDA1, EDAR, EDARADD, and WNT10A) account for 90% of hypohidrotic/anhidrotic ectodermal dysplasia cases. Hum Mutat 2011;32:70-2.
[Google Scholar]
|
| 3. |
NaBadalung DP. Prosthodontic rehabilitation of an anhidrotic ectodermal dysplasia patient: A clinical report. J Prosthet Dent 1999;81:499-502.
[Google Scholar]
|
| 4. |
Aswegan AL, Josephson KD, Mowbray R, Pauli RM, Spritz RA, Williams MS. Autosomal dominant hypohidrotic ectodermal dysplasia in a large family. Am J Med Genet 1997;72:462-7.
[Google Scholar]
|
| 5. |
Ioannidou-Marathiotou I, Kotsiomiti E, Gioka C. The contribution of orthodontics to the prosthodontic treatment of ectodermal dysplasia: A long-term clinical report. J Am Dent Assoc 2010;141:1340-5.
[Google Scholar]
|
Fulltext Views
3,130
PDF downloads
1,746





