Translate this page into:
Gardner-Diamond syndrome: Psychogenic purpura with premenstrual flare
Corresponding author: Dr. Maria Ansari, Department of Dermatology, A. J. Institute of Medical Sciences and Research Centre, AJIMS, Kuntikana, Mangalore, India. maria.ansari9@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Ansari M, P N Girish, K M Fathima Fyma, Abdul Salam AQ, Bhat M, Aithal N. Gardner-Diamond syndrome: Psychogenic purpura with premenstrual flare. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1209_2024
Dear Editor,
Gardner-Diamond syndrome or autoerythrocyte sensitisation syndrome is a rare psychodermatological disorder characterised by recurrent painful ecchymoses triggered by emotional stress or trauma. It is seen predominantly in young women, and it’s exact prevalence remains low. This case report delineates an atypical presentation marked by a correlation with the patient’s menstrual cycle and systemic symptoms – factors that are seldom reported and may significantly complicate the diagnosis.
A 16-year-old girl presented with multiple painful ecchymotic patches on her arms, chest, and thighs for the past seven months. These episodes, occurring intermittently, were associated with polyarthralgia and generalised weakness, each lasting seven to eight days. The lesions were preceded by prodromal pain on the skin and healed without any post-inflammatory changes. She also reported a history of premenstrual flares. Additionally, she experienced blood in her urine and recurrent urinary tract infections over the past three months. Her family was concerned due to these urinary symptoms, given a family history of renal failure in her father.
There was no history of trauma, self-infliction of skin lesions, abdominal pain, diarrhea, fever, weight loss, breathlessness, mucosal bleeding, or photosensitivity. However, the patient’s psychiatric history revealed symptoms of low mood and fearfulness, particularly following her grandmother’s death. She experienced occasional crying spells, difficulty accepting her grandmother’s death, auditory hallucinations of her grandmother’s voice, and episodic fearfulness associated with palpitations and tremors. The psychiatrist diagnosed her with prolonged grief disorder.
Cutaneous examination revealed multiple, well to ill-defined, scattered purpura and ecchymoses, ranging from 0.5 cm to 6 cm, present over the anterior aspect of her both upper limbs [Figure 1] and lower limbs with mild tenderness. No secondary changes like scaling, scabbing, atrophy, or ulceration were noted. The patient was kept under observation in the hospital for one week to rule out any factitious cause.

- Multiple, well- to ill-defined, scattered purpura and ecchymoses present on the left arm.
Investigations showed raised ESR (erythrocyte sedimentation rate), reduced prothrombin time, haematuria, and albuminuria without pus cells. Platelet count, coagulation profile, renal function tests, and complement levels (C3 and C4) were within normal limits. The Antinuclear antibody (ANA) profile was negative. Skin biopsy from the ecchymotic patch on the right arm revealed extravasated erythrocytes in the dermis without any evidence of vasculitis [Figure 2]. Direct immunofluorescence was negative. A positive autoerythrocyte sensitisation test (AEST), performed with intradermal injection of 0.1 mL of washed autologous RBCs, showed approximately 40% extension of ecchymosis after 24 hours, which confirmed the diagnosis of Gardner-Diamond syndrome [Figure 3].
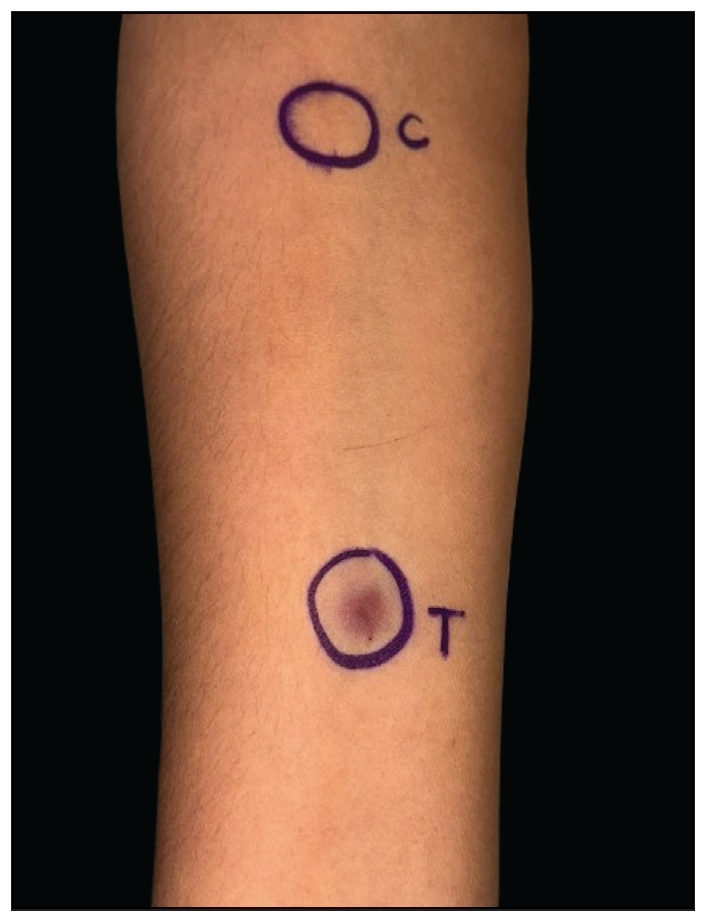
- Positive autoerythrocyte sensitisation test (AEST) after 24 hours, as seen on the flexor aspect of the right forearm (C-control, T-test).
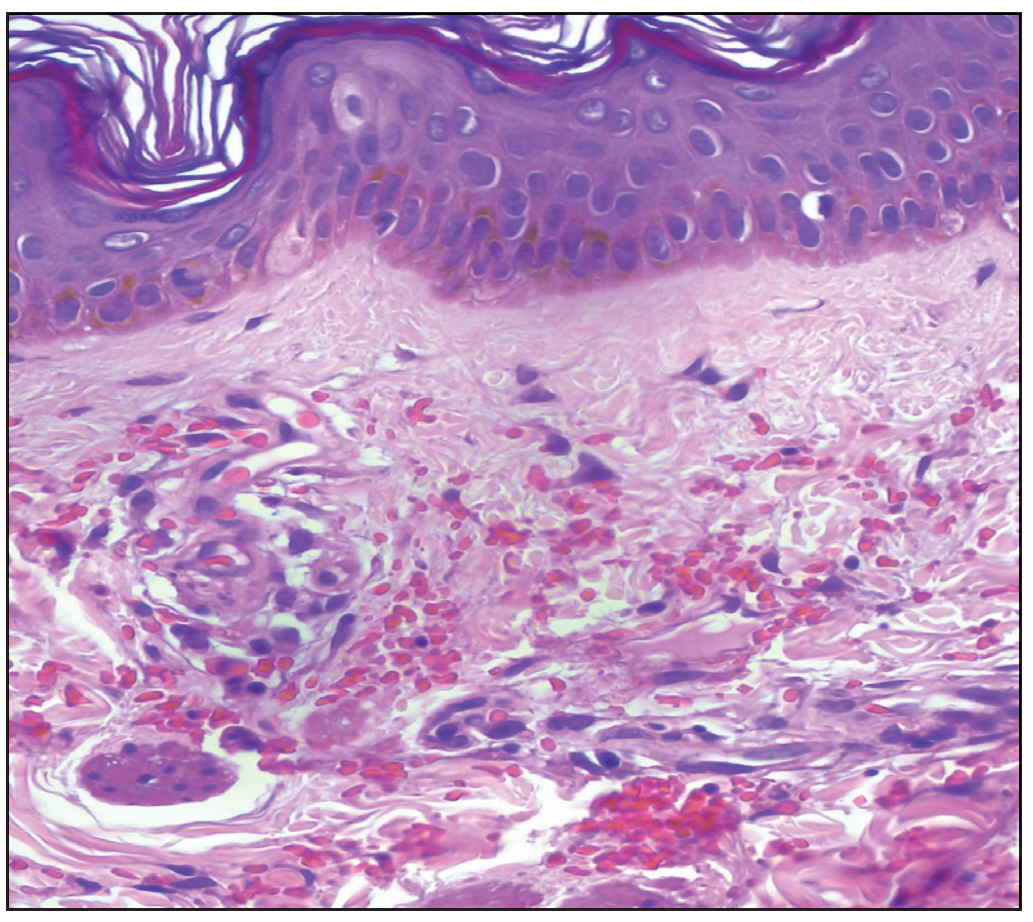
- Histopathology showing extravasation of red blood cells from small dermal vessels without vasculitis (Haematoxylin and eosin, 40x).
Grief resolution therapy and supportive psychotherapy were provided to help the patient cope with emotions triggered by memories, accept the finality of the loss, and design a new life without the deceased. A topical medication (cream) containing glycerin, almond oil, oat extract, and Tasmanian pepper berry extract, among others, was prescribed to the patient. The patient responded well to the psychotherapy alone and was not prescribed any oral medications. The parents did not consent for a renal biopsy.
Gardner-Diamond syndrome or autoerythrocyte sensitisation syndrome is a rare condition marked by the sudden appearance of painful purpura or bruises, often triggered by emotional stress or trauma.1 In addition to skin findings, patients often have a history of mood and anxiety disorders, leading to the term psychogenic purpura. Depression is the most common psychiatric abnormality in these patients.2 Patients develop autoantibodies against elements of the erythrocyte stroma as well as DNA (deoxyribonucleic acid), haemoglobin, and phosphatidylserine.3 The exact mechanism underlying psychiatric disease and autosensitisation to erythrocytes remains unknown, but psychological stress significantly alters haemostatic equilibrium.4
A multidisciplinary approach focusing on improving psychological conditions is crucial for effective treatment. The stress response hypothesis suggests a psychoendocrine model where neuropeptide signaling molecules affect cell surface receptors, altering haemostatic processes via catecholamine and glucocorticoid release.5,6 Alleviating acute stress and addressing psychological factors are key to achieving longer periods of remission.7
Gardner-Diamond syndrome is an exceptionally rare disorder, with only about 280 cases reported worldwide and very few documented in the literature. A multidisciplinary approach involving dermatologists, psychiatrists, and nephrologists is crucial for effective management. This case highlights the critical interplay between hormonal influences (menstrual correlations) and psychological factors. The unusual presence of albuminuria and haematuria suggests potential systemic implications, adding urgency to understanding and treating this condition.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Role of autoerythrocyte sensitization test in the diagnosis of recurrent spontaneous bruising. Indian Dermatol Online J. 2023;14:375-8.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Clinical and psychological patterns in auto-erythrocyte sensitivity. Ann Intern Med. 1965;63:255-65.
- [CrossRef] [PubMed] [Google Scholar]
- Psychogenic purpura (autoerythrocyte sensitization): An unsolved dilemma. Am J Med. 1989;87:16N-21N.
- [PubMed] [Google Scholar]
- Autoerythrocyte sensitization syndrome (Gardner-Diamond syndrome): Review of the literature. J Eur Acad Dermatol Venereol. 2009;23:499-504.
- [CrossRef] [PubMed] [Google Scholar]
- Stress, stigmatization and psychosomatic purpuras. Int Angiol. 1995;14:130-7.
- [PubMed] [Google Scholar]
- Psychogenic purpura (Gardner-Diamond Syndrome) Prim Care Companion CNS Disord. 2015;17
- [CrossRef] [Google Scholar]





