Translate this page into:
Generalised primary cutaneous anaplastic large cell lymphoma: A diagnostic challenge
Corresponding author: Dr. Lin Wang, Department of Dermatology and Venereology, West China Hospital, Sichuan University, Chengdu, China. lkzwl@126.com
-
Received: ,
Accepted: ,
How to cite this article: Chen Y, Zhou X, Dang Zeng Z, Zhou P, Zhang X, Wang L. Generalised primary cutaneous anaplastic large cell lymphoma: A diagnostic challenge. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_1676_2024
Dear Editor,
A 57-year-old man presented with a two-year history of multiple papules, plaques, nodules and masses on his trunk and extremities, accompanied by significant itching and pain. Ulcers had gradually developed on these cutaneous lesions six months ago. Notably, he had no constitutional symptoms such as fever, night sweats, diarrhoea or weight loss. The patient reported exposure to a region with a high incidence of leprosy and mentioned contact with a sewer four years ago. An initial diagnosis of atypical mycobacteriosis was made and treatment with levofloxacin and rifampicin for three months yielded mild improvement. Physical examination revealed numerous papules, plaques, nodules, and masses (the largest approximately 5 × 3 cm) on the trunk, buttocks, and extremities, with elevated borders, central ulcerations and increased skin temperature [Figures 1a-c].
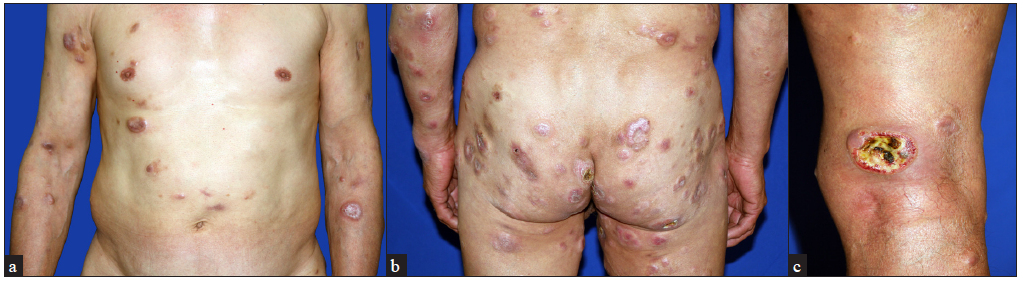
- Multiple well-demarcated papules, coin-sized plaques and nodules (a) on the trunk and upper extremities, (b) on the buttocks and (c) an ulcer with a purulent coating over the right leg.
Laboratory investigations including routine blood tests, biochemical analyses, HBV, HCV, HIV, Epstein-Barr virus DNA screenings, coagulation studies, urinalysis, stool evaluations, and metagenomic next-generation sequencing (mNGS) were unremarkable. A repeat skin biopsy revealed mild epidermal hyperplasia and a diffuse infiltrate of numerous large histiocyte-like cells, lymphocytes, eosinophils, neutrophils and nuclear dust in the dermis and subcutaneous tissue [Figures 2a-b]. Large cells with transparent cytoplasm and occasional mitotic figures were noted. Immunohistochemistry showed positivity for CD2, CD3, CD5, CD43, CD4, LCA, Ki67 (+,40%) and strong CD30 (>75%) expression [Figures 3a-3h] but negativity for CD7, CD8, CD56, CD20, CD79a, TIA-1, granzyme B, S100, CD1a, CD207, CD68 (PGM-1), CD163, PCK, CD31, GATA3, anaplastic lymphoma kinase (ALK), epithelial membrane antigen (EMA). Epstein-Barr virus-encoded RNA (EBER1/2) in situ hybridisation, periodic acid-Schiff, Gomori methenamine silver and acid-fast stains were negative. T cell receptor γ gene rearrangement was identified. Bone marrow aspiration and flow cytometry were unremarkable. DUSP22-IRF4 gene translocation was not detected. A positron emission tomography/computed tomography scan showed an elevated 18F-fluoro-deoxyglucose (18F-FDG) value with a maximal standardised uptake value of 18.6 in skin and subcutaneous lesions. Elevated 18F-FDG values (8.6 and 8.16, respectively) in the axillae and inguinal lymph nodes were noted. The remaining organs are unremarkable.
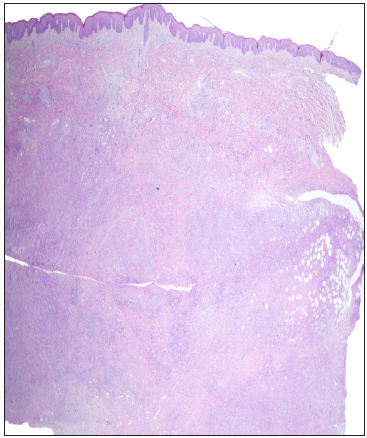
- Mild epidermal hyperplasia and a diffuse infiltrate of numerous inflammatory cells (Haematoxylin and eosin, 12.5x).
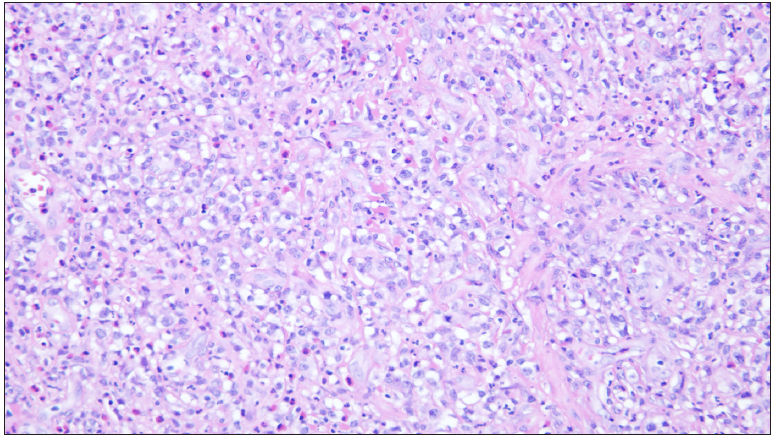
- Large histiocyte-like cells, lymphocytes, eosinophils, neutrophils and nuclear dust in the dermis (Haematoxylin and eosin, 200x).
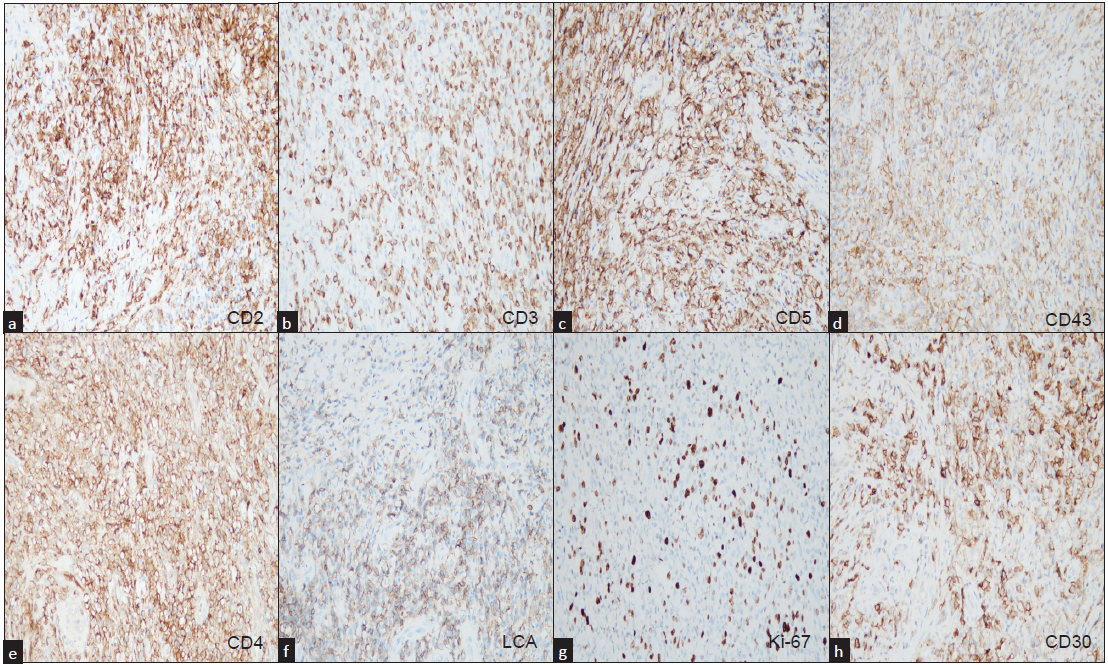
- Positive immunohistochemical staining of large cells with transparent cytoplasm (200×).
Based on these findings, primary cutaneous anaplastic large cell lymphoma (PcALCL) (T3bNxM0) was diagnosed. Brentuximab vedotin treatment was initiated with a dosage of 1.8mg/kg on a three-week schedule, resulting in excellent improvement after three cycles of brentuximab vedotin without adverse effects.
PcALCL is a relatively common cutaneous T-cell lymphoma (CTCL) and is classified among the cutaneous CD30+ T-cell lymphoproliferative disorders.1 It represents approximately one-third of CTCL cases, along with lymphomatoid papulosis and borderline lesions.1 It predominantly affects males in the sixth decade of life. PcALCL is typically ALK-negative and manifests as a solitary and localised papule or nodule that may ulcerate. Sites of predilection are the face, trunk and extremities.1 Although multifocal lesions are observed in as many as 20% of cases, generalised involvement, as seen in this case, is rare.1 A prior study reported limited involvement in one region for 14% of patients with multifocal lesions.2 In contrast, this case presented with multifocal lesions affecting several anatomical sites.
Multifocal PcALCL can mimic other skin conditions, such as systemic anaplastic large cell lymphoma with cutaneous involvement (s-ALCL), mycosis fungoides with CD30+ large cell transformation (TMF), and atypical mycobacteriosis. s-ALCL typically presents with advanced disease, B-symptoms and a progressive course, affecting younger males, with positive ALK (majority) and EMA immunostaining.3 TMF usually has patch-plaque lesions before the tumour stages. Positivity of GATA3 might help to exclude PcALCL. Notably, TMF has a poor prognosis.1 Atypical mycobacteriosis manifests as disseminated papules, plaques, nodules, and ulcers, often at trauma sites in immunocompromised patients.4 Histopathological examination commonly shows prominent suppurative inflammation with sparse granuloma formation and an abundance of acid-fast bacilli.4 Microbiological culture, mNGS and special stains were negative in our case and the treatment for atypical mycobacteriosis was ineffective.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Primary cutaneous anaplastic large cell lymphoma-A review of clinical, morphological, immunohistochemical, and molecular features. Cancers (Basel). 2023;15:4098.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Clinical spectrum of primary cutaneous CD30-positive anaplastic large cell lymphoma: An analysis of the mannheim cutaneous lymphoma registry. J Dtsch Dermatol Ges. 2012;10:331-9.
- [CrossRef] [PubMed] [Google Scholar]
- ALK-Negative primary cutaneous anaplastic large cell lymphoma with systemic involvement or systemic ALCL with cutaneous lesion A diagnostic dilemma. Am J Dermatopathol. 2022;44:376-9.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and histopathological features of cutaneous nontuberculous mycobacterial infection: A review of 13 cases. J CutanPathol. 2017;44:433-43.
- [CrossRef] [Google Scholar]
- Anaplastic large cell lymphoma: Molecular pathogenesis and treatment. Cancers (Basel). 2022;14:1650.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Primary cutaneous anaplastic large-cell lymphoma: A review of the SEER database from 2005 to 2016. Clin Exp Dermatol. 2021;46:1420-6.
- [CrossRef] [PubMed] [Google Scholar]





