Translate this page into:
“Generalized exanthematous pustular dermatophytid” in a 4-year-old child: A misdiagnosed entity
Corresponding author: Dr. Kamar Belhareth, Department of Dermatology, Fattouma Bourguiba HospitalMonastir, Tunisia. kmar.belhareth@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Belhareth K, Soua Y, Korbi M, Njima M, Youssef M, Belhadjali H, et al. “Generalized exanthematous pustular dermatophytid” in a 4-year-old child: A misdiagnosed entity. Indian J Dermatol Venereol Leprol 2021;87:249-52.
Sir,
A previously healthy 4-year-old child was referred to the dermatology department for an inflammatory, crusted, matted mass over the scalp progressing for 2 weeks [Figure 1].

- Inflammatory and crusted, matted mass on the scalp (kerion)
Direct microscopic examination of the hair sample from the affected area in 10% potassium hydroxide revealed an endothrix pilar invasion with the presence of septate hyaline hyphae. After 4 weeks, Trichophyton tonsurans was isolated from the culture using Sabouraud agar.
The diagnosis of a kerion was made. Three days after oral micronized griseofulvin initiation (22 mg/kg/d), the child presented with a generalized pustular eruption initially localized to the palms and soles which then rapidly spread over the entire body in the next few days. She had no fever and no other constitutional symptoms. On clinical examination, we found multiple, large, non-follicular pustules on a nonerythematous base especially on the palms and soles; also on her face, trunk and arms [Figures 2-4]. Intertriginous areas were spared. Blood analysis showed leucocytosis (12000/µl), neutrophilia (7000/µl) and a slight increase in C-reactive protein (20 mg/l). Bacteriological and mycological cultures of samples obtained from the pustular lesions were sterile. Biopsy revealed a subcorneal pustule containing a small amount of neutrophils. The dermis showed a moderate perivascular, lymphohistiocytic inflammatory infiltrate with the presence of some eosinophils [Figures 5 and 6]. A diagnosis of “generalized exanthematous pustular dermatophytid” was suspected. We opted to maintain griseofluvin at the same dose, and to add a high-potency topical steroid and systemic corticosteroids (dexamethasone sodium phosphate) (0.5 mg/kg/d) to the treatment protocol. The eruption resolved completely within 5 days of starting the treatment [Figure 7]. Systemic corticosteroids were stopped and griseofulvin was continued for 2 months.

- Multiple, large, non-follicular pustules on the palms

- Pustules on the soles

- Generalized pustular eruption on the trunk
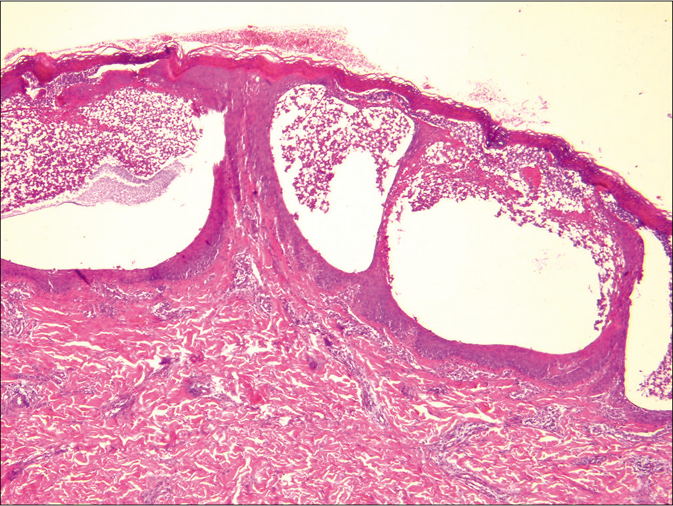
- Subcorneal pustule containing neutrophils (H and E, ×40)

- Complete resolution of the eruption
The diagnosis of generalized exanthematous pustular dermatophytid was established based on the presence of a mycologically documented dermatophyte infection (kerion), the absence of dermatophytes in distant pustular lesions and the resolution of all symptoms after maintaining antifungal therapy and initiating systemic corticosteroid therapy.
This entity is a rarely reported form of dermatophytids, which are immunologically mediated dermatologic reactions secondary to dermatophyte infections commonly seen in patients with tinea pedis and typically described as a vesicular eruption. Dermatophytids secondary to kerion are less common. A recent prospective study revealed that 13 of 19 patients (68%) with kerion celsi developed dermatophytid reactions1. The main clinical manifestations of these reactions are: eczematous eruptions (36.8%), pruritic papules (15.8%), eczematous eruptions, excoriated papules and pustules (10.5%) and angioedema-like reaction (5.3%).1 According to literature, only four cases of generalized exanthematous pustular dermatophytid have been reported [features of all reported cases are summarized in Table 1].2,3 Three of those reported cases occurred within 2-3 days of griseofulvin intake and in one case, the eruption occurred spontaneously. All cases were characterized with a pustular eruption predominating initially in the cephalic region then spreading to the entire body. Fever was present in two cases and only one case was complicated with inflammatory chondritis. The palmoplantar onset of the rash, as noted in our case, had never been previously reported.
| Reported cases | Age (years) | Sex | Lesion/ Causative agent | Clinical appearance | Time to 'id' eruption | Laboratory parameters | Treatment |
|---|---|---|---|---|---|---|---|
| Liu et al., 20113 | 8 | Female | Multiples kerion/TM | Widespread pustules, head+Fever 38.9 | 17 days after kerion | Leucocytosis 20,300/mm3 Blood cultures (−) |
Oral itraconazole (5 mg/kg/day) + low-dose Dexamethasone (0.075 mg/kg/day) |
| Ronjat 20152 | 11 | Male | Kerion/TT | Fever 39 Widespread pustules, head+Lymphadenopathy Bilateral chondritis |
2 months after kerion 2 days after Griseofulvin |
Polynucleosis 7200/mm3 Monocytosis 1200/mm3 Eosinophilia 500/mm3 CRP: 28 mg/L |
Oral corticosteroid 0.75 mg/kg/day + amoxicillin/clavulanic acid + griseofulvin (25 mg/kg/day) |
| Ronjat 20152 | 6 | Male | Kerion/TS | Widespread pustules, head+ | 6 weeks after kerion 2 days after Griseofulvin |
Normal | High-potency topical steroids + griseofulvin (20 mg/kg/day) |
| Ronjat 20152 | 6 | Female | Kerion/TM | Widespread pustules, head+Eczematous eruption Lymphadenopathy |
8 weeks after kerion 3 days after Griseofulvin |
Normal | High-potency topical steroids + griseofulvin (19 mg/kg/day) |
| Our case | 4 | Female | Kerion/TM | Widespread pustules, palms and soles++ | 2 months after kerion 3 days after Griseofulvin |
Leucocytosis 12,000/mm3 CRP: 15 mg/L |
Griseoulvin + high-potency topical steroids + oral corticosteroid (0.5mg/kg/day) |
TM: Trichophyton mentagrophyte, TT: Trichophyton tonsuran, TS: Trichophyton soudanense, CRP: C-reactive protein
The most concerning differentials diagnosis of generalized pustular psoriasis was ruled out because of the clinical and pathological findings. The main differential diagnosis in our case was acute generalized exanthematous pustulosis. The lack of diffuse erythema, the absence of the involvement of intertriginous areas and the favorable evolution despite continued griseofluvin treatment made this diagnosis unlikely. Moreover, griseofulvin-induced acute generalized exanthematous pustulosis has not been previously reported. The typical histopathology of acute generalized exanthematous pustulosis shows spongiform subcorneal and/ or intraepithelial pustules, an edematous papillary dermis and perivascular infiltrates with neutrophils and some eosinophils. In some cases, necrotic keratinocytes and leucocytoclastic vasculitis can also be found. In our case, histopathological aspect was not different from acute generalized exanthematous pustulosis. We were unable to find any previous reports with histological description of generalized exanthematous pustular dermatophytid. Thus, we cannot conclude on the existence of a distinctive criteria to differentiate between these two entities. Further histological studies may be helpful to identify possible histologic characteristics of generalized exanthematous pustular dermatophytid.
The exact mechanism of generalized exanthematous pustular dermatophytid is still unknown. To the best of our knowledge, no case of terbinafine-associated generalized exanthematous pustular dermatophytid has been reported. Some authors have linked the flare of dermatophytid reaction after the administration of griseofulvin or terbinafine to the release of fungal antigens as a result of antimycotic therapy.4,5 Others suggest a local immunological response to systemically absorbed fungal antigen, especially some zoophilic species.3 The treatment of generalized exanthematous pustular dermatophytid is non-codified, due to the scarcity of reported cases. Oral corticosteroid treatment and/or high-potency topical steroids given as an adjunct to griseofulvin treatment (19 to 23 mg/kg/d) were used with a favorable resolution in the reported cases.2,3
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Are dermatophytid reactions in patients with kerion celsi much more common than previously thought? A prospective study. Pediatr Dermatol. 2015;32:635-40.
- [CrossRef] [PubMed] [Google Scholar]
- Generalized exanthematous pustular dermatophytid, a rare clinical presentation of dermatophytid reaction. Ann Dermatol Venereol. 2015;142:270-5.
- [CrossRef] [PubMed] [Google Scholar]
- Severe kerion with dermatophytid reaction presenting with diffuse erythema and pustules. Mycoses. 2011;54:e650-2.
- [CrossRef] [PubMed] [Google Scholar]
- Erythema nodosum induced by kerion celsi of the scalp in a child: A case report and mini-review of literature. Mycoses. 2013;56:200-3.
- [CrossRef] [PubMed] [Google Scholar]
- Dermatophytid in tinea capitis: Rarely reported common phenomenon with clinical implications. Pediatrics. 2011;128:e453-7.
- [CrossRef] [PubMed] [Google Scholar]





