Translate this page into:
Generalized lichen nitidus: Successful treatment with systemic isotretinoin
2 Department of Pathology, Okmeydani Research and Training Hospital, Istanbul, Turkey
Correspondence Address:
Ilteris Oguz Topal
Department of Dermatology, Okmeydani Research and Training Hospital, Istanbul
Turkey
| How to cite this article: Topal IO, Gokdemir G, Sahin IM. Generalized lichen nitidus: Successful treatment with systemic isotretinoin. Indian J Dermatol Venereol Leprol 2013;79:554 |
Sir,
Lichen nitidus (LN) is a chronic inflammatory skin disease characterized by a large number of skin-colored or erythematous millimetric papules. Lesions are typically distributed on the penis, genital area, abdomen, and extremities. Various clinical forms of the disease such as confluent, vesicular, hemorrhagic, palmoplantar, follicular, perforating, linear are often defined in children and young adults, and the generalized form of the disease is rare. [1],[2] Herein, we present a young girl with generalized LN who was successfully treated with systemic isotretinoin.
A 15-year-old female patient came to our outpatient clinic complaining of a rash on her body. The patient said that the red papules had first appeared on her body 1 year earlier and that these papules had spread to her arms and back within the last few weeks. She was treated with topical steroids and given a short-term systemic steroid therapy (prednisolone 1mg/kg for 1.5 month). No regression was seen in the patient′s lesions, but there was also no improvement. Her dermatological examination showed bright, diffuse follicular papular lesions which were skin-colored or partially light pink in color. They were 1-2 mm in diameter and distributed on her body and back as well as her arms and legs [Figure - 1]a. Nail and oral mucosal examinations were normal. A punch biopsy sample was taken from a papule on the back which showed a focal, well-circumscribed infiltrate of the lymphocytes that was closely attached to the epidermis and the melanophages in the papillary dermis. The epidermis revealed that there was flattening and a partial coalescence of rete ridges in the epidermis, and the ones on the margins of the granuloma were elongated, creating the image of a claw-like configuration [Figure - 2]. The patient was diagnosed with LN according to these findings, and phototherapy was recommended. However, the patient did not accept this treatment because she lived outside of town. Laboratory examinations of the patient were normal; therefore, treatment with 40 mg/day (0,8 mg/kg) of isotretinoin was started. Laboratory tests were repeated every month. When the patient was followed up 4 months afterward, the lesions had significantly regressed [Figure - 1]b, and her treatment was discontinued. The 10-month follow-up did not show any recurrence.
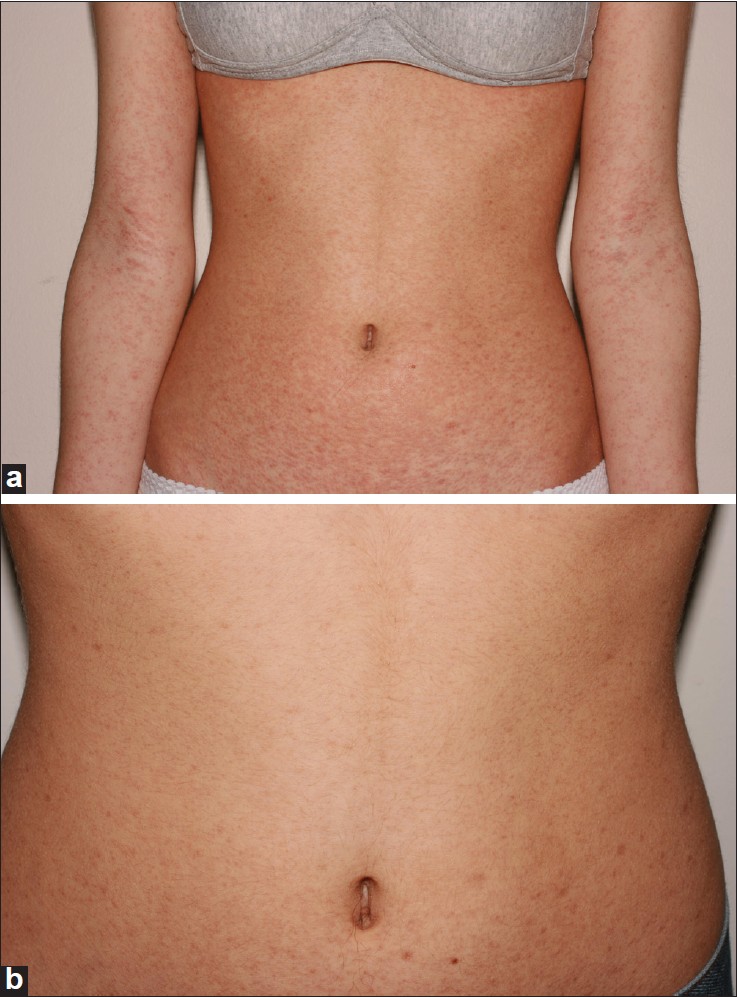 |
| Figure 1: (a) Diffuse skin-colored shiny papular lesions on the body and on the arms, (b) Most of the papules had completely disappeared after the use of systemic isotretinoin |
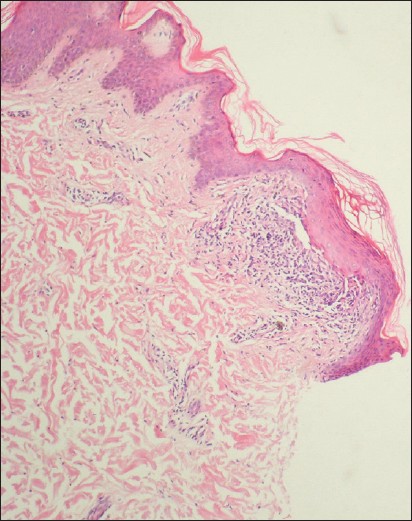 |
| Figure 2: Biopsy of a papule shows a focal, well-circumscribed infiltrate of the lymphocytes extending to the epidermis and the downward extension of the rete ridges at the lateral margin of the infiltrate, which produces a typical "claw-like" configuration and the melanophages in the papillary dermis (H and E, × 100) |
LN is a self-limited disease, and the lesions usually resolve spontaneously. [3] Medical treatment should be considered if the lesions are persistent and diffuse or if they cause itching or cosmetic discomfort in the patient. Topical and systemic steroids, ultraviolet A and B treatment, and immunotherapy with dinitrochlorobenzene or dinitrocyclopropenon are currently being used to combat this disease along with agents such as retinoids, selective H1 antagonist, itraconazole, and isoniazid. [2]
Retinoids are thought to suppress inflammation, especially by modulating the effects on lymphocytes and reducing the migration of neutrophils and eosinophils to the epidermis. In addition, the production of antiproliferative effects also makes them effective in the treatment of LN. [4]
Our patient had cosmetic fears because of the diffuse lesions along with complaints of itching. For this
reason, we decided to administer a systemic agent. Ultraviolet therapy was not started because the patient lived far from the phototherapy center. Instead, treatment with isotretinoin 40mg/day was begun, and a significant regression in the lesions occurred after 4 months.
The major limiting factor for the use of isotretinoin has revolved around the risks associated with potential adverse effects, the most common of which include cheilitis, xerosis, myalgia, and arthralgia. In addition, the mucous membranes and eyes can also be affected; however, all of these adverse effects are dose-dependent and reversible. Isotretinoin treatment may also promote premature epiphyseal plate closure and stop normal growth in some children, but these occurrences are rare. In the future, a careful follow-up of young patients who are being treated with retinoids is required. [5]
We found no case reports regarding the use of systemic isotretinoin for generalized LN in the literature. However, acitretin has been previously reported to be successful for treating the palmoplantar forms of this disease, as evidenced by Thibaudeau et al. who described an 53-year-old woman with palmoplantar LN that was successfully treated with this medication. [6]
Among oral retinoids, isotretinoin appears to have the advantage of a shorter half-life, which minimizes the possibility of adverse events. In our patient, at the 10-month follow-up after the cessation of treatment, no permanent adverse events or recurrences were noted.
In conclusion, our patient, who had the generalized form of LN, had a dramatic response to isotretinoin treatment, and this drug should be considered as a safe, rapid-acting option for others with this disease.
| 1. |
Chen W, Schramm M, Zouboulis CC. Generalized lichen nitidus. J Am Acad Dermatol 1997;36:630-1.
[Google Scholar]
|
| 2. |
Agarwal S, Guglani V, Kumar B. Down's syndrome with lichen nitidus and segmental vitiligo. Indian J Dermatol Venereol Leprol 2009;75:627-9.
[Google Scholar]
|
| 3. |
Do MO, Kim MJ, Kim SH, Myung KB, Choi YW. Generalized lichen nitidus successfully treated with narrow-band UVB phototherapy: Two cases report. J Korean Med Sci 2007;22:163-6.
[Google Scholar]
|
| 4. |
Sekula-Gibbs S, Uptmore D, Otillar L. Retinoids. J Am Acad Dermatol 2004;50:405-15.
[Google Scholar]
|
| 5. |
Rademaker M. Adverse effects of isotretinoin: A retrospective review of 1743 patients started on isotretinoin. Australas J Dermatol 2010;51:248-53.
[Google Scholar]
|
| 6. |
Thibaudeau A, Maillard H, Croué A, Belperron P, Avenel Audran M, Verret JL. Palmoplantar lichen nitidus: A rare cause of palmoplantar hyperkeratosis. Ann Dermatol Venereol 2004;131:822-4.
[Google Scholar]
|
Fulltext Views
5,822
PDF downloads
1,602





