Translate this page into:
Generalized morphea developing in a patient previously affected with eosinophilic fasciitis
2 Department of Dermatology, Venereology and Leprosy, Shri Bhausaheb Hire Government Medical College, Dhule, Maharashtra, India
Correspondence Address:
Resham J Vasani
A/1 Sharad Kunj, Dr. Moose Road, Thane (west)
India
| How to cite this article: Vasani RJ, Medhekar SV. Generalized morphea developing in a patient previously affected with eosinophilic fasciitis. Indian J Dermatol Venereol Leprol 2012;78:654-656 |
Sir,
A forty-four-year-old female presented with diffuse swelling with brownish tender induration of forearms and legs for the past one month. She had no history of fever, joint pains, mucosal lesions, dysphagia, dyspnoea, Raynaud′s phenomenon or proximal muscle weakness.
The clinical examination showed minimally erythematous areas of induration distributed symmetrically over flexors of forearms and legs [Figure - 1]a. On raising the forearm, there was linear furrowing along the blood vessels suggestive of dry river bed sign. A clinical diagnosis of eosinophilic fasciitis (EF) was made.
Investigations showed the presence of peripheral eosinophilia (absolute eosinophil count -1206), raised ESR (105 mm at the end of 1 h), raised IgG levels of 2000 IU/ml (N- 700-1700 IU/ml), positive ANA (1:100 in a speckled pattern), Anti Scl 70 and Anti centromere antibodies were negative. The hepatic, renal, thyroid profiles and chest radiograph were normal. The histopathological examination showed the presence of normal epidermis with the dermis showing widening of the fascial planes and septae with predominant eosinophilic infiltrate [Figure - 1]b and c. Thus, the diagnosis of EF was established.
The patient was started on oral prednisolone at the dose of 60 mg and gradually tapered over three months with subjective and objective improvement of the skin lesions.
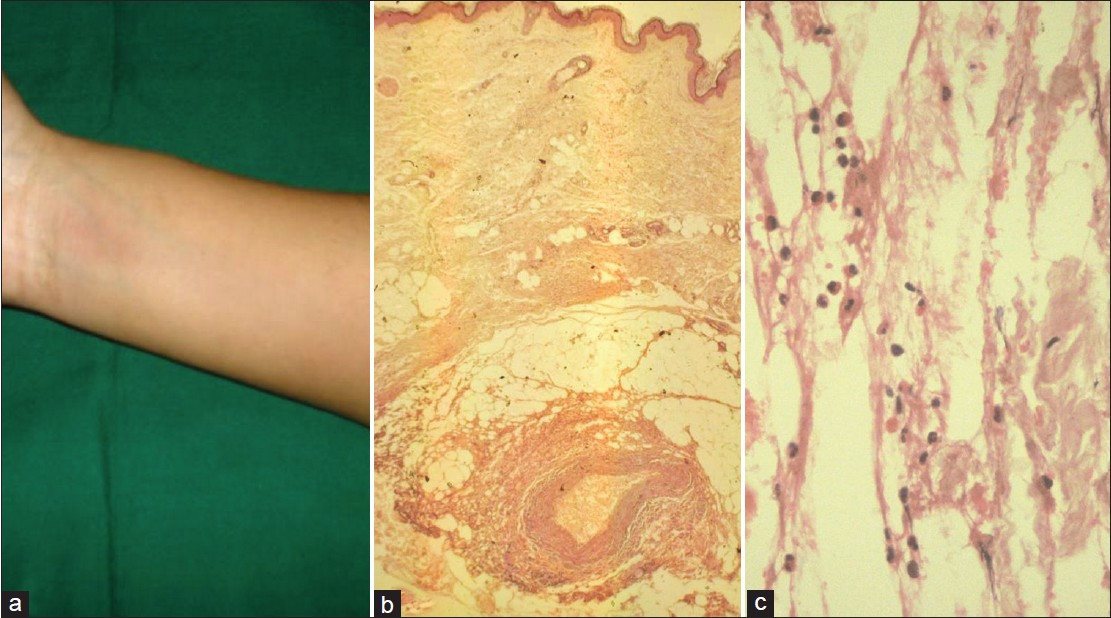 |
| Figure 1: (a) Ill-defined area of induration with overlying skin showing mild erythema over the flexor aspect of the forearm. (b) (H and E, ×4) - Normal epidermis and dermis with thickened fascial planes showing mixed infiltrate. (c) (H and E, ×40) - Predominance of eosinophils in the fascial infiltrate |
One year later, the patient presented with symptoms of multiple reddish to dark colored lesions on the trunk. The lesions were associated with itching and tightness overlying the lesions. Similar lesions were also present over the forearms and legs giving rise to restricted movements at the bilateral wrist joints.
Both general and systemic examination were normal. Dermatological examination showed the presence of multiple ill-defined, depressed, hyperpigmented plaques with thinned out; atrophic, shiny skin overlying them [Figure - 2]a. The plaques varied from 2 cm to 30 cm in their greatest dimensions. They were present over the back, chest, abdomen and proximal extremities. Rest of the cutaneous areas including the acral areas, palms, soles and mucosae were normal.
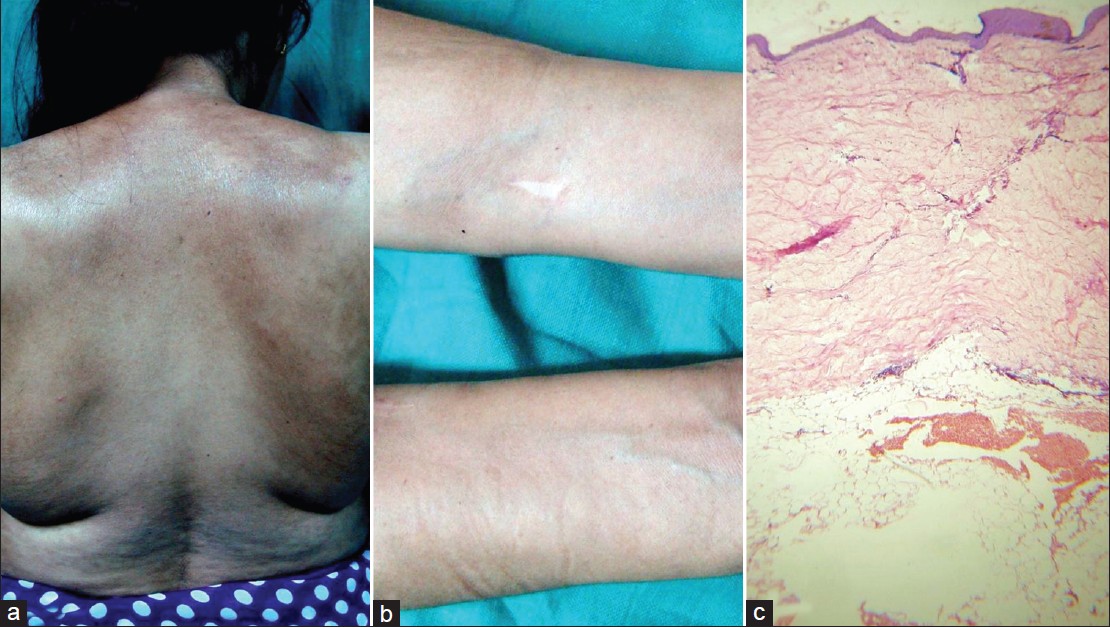 |
| Figure 2: (a) Multiple ill-defined, depressed, hyperpigmented plaques with thinned out, atrophic, shiny skin on the back and proximal extremities of generalized morphea. (b) Previous site of eosinophilic fasciitis showing residual depression of the affected areas with prominence of the veins traversing the area. (c) (H and E, ×4) - Atrophic epidermis, thick, deeply eosinophilic, closely packed bundles of collagen in the reticular dermis and subcutis s/o morphea |
The areas on the forearms and legs which showed changes of EF earlier, now showed residual depression of affected areas with prominence of veins traversing the area [Figure - 2]b. The clinical diagnosis was generalized morphea (GM).
This time investigations showed a normal eosinophil count with raised ESR (38 mm at end of 1 h), positive ANA (1:100, speckled pattern), negative anti centromere antibody and Anti Scl 70 antibody. Chest radiograph, liver, renal, thyroid profiles and abdominal ultrasound were normal. Histopathological examination showed atrophic epidermis, thick deeply eosinophilic, closely packed bundles of collagen in the reticular dermis and subcutis with atrophic appendages confirming morphea [Figure - 2]c. The patient was started on methotrexate 10 mg per week, but was lost to follow up thereafter. The final diagnosis was GM developing in an old case of EF.
It is controversial whether GM and EF are two distinct entities, whether EF is a variant of deep morphea [1] or whether EF and morphea represent a continuum of the same disease.
EF is characterized by an acute onset usually precipitated by strenuous exercise. [2] There is diffuse symmetrical involvement, with peripheral eosinophilia and hypergammaglobulinemia. The histology is specific with marked fibrosis and diffuse infiltration of the fascia with eosinophils. It is usually well responsive to oral corticosteroids.
GM usually has an insidious onset, with widespread involvement of more than two anatomic areas with well circumscribed ivory white plaques surrounded by lilac border in early stages and hyperpigmentation as lesions evolve. Poor response to corticosteroid treatment is noted.
There are certain overlapping features as follows. Both EF and morphea show similar sclerosis of skin, immunological pathogenesis, absence of sclerodactyly, visceral involvement and Raynaud′s phenomenon. Although peripheral and tissue eosinophilia and hypergammaglobulinemia are typically seen in EF, they are not the pre requisites for diagnosis [3] and can also be seen in early stages of morphea. The inflammation of the fascia in EF can extend to the adjacent dermis and also the dermal inflammation of morphea extends to the fascia as in the pansclerotic variant. Though presence of fascial inflammation and fibrosis are more consistent features of EF than morphea, it is possible that failure to routinely observe fascial fibrosis in morphea may be due to inadequate depth of biopsy which usually does not involve the subcutis. Concurrent lesions of morphea is noted in 25 to 30% cases of EF. [4] There have been case reports of transition of EF to localized GM [5] and even systemic sclerosis.
Hence to conclude, while clinical presentation in conjunction with histological details in most of the instances will allow one to differentiate EF from scleroderma, there is undeniable evidence that these two entities do share certain morphologic features that in late stages of these diseases may make their separation difficult warranting further study and long-term follow up of these patients.
| 1. |
Naschitz JE, Boss JH, Misselevich I, Yeshurun D, Rosner I. The fasciitis-panniculitis syndromes: Clinical and pathologic features. Medicine (Baltimore) 1996;75:6-16.
[Google Scholar]
|
| 2. |
Lakhanpal S, Ginsburg WW, Michet CJ, Doyle JA, Moore SB. Eosinophilic fasciitis: Clinical spectrum and therapeutic response in 52 cases. Semin Arthritis Rheum 1988;17:221-31.
[Google Scholar]
|
| 3. |
Jensen E, Hess B, Hunziker T, Roos F, Helbling A. Eosinophilic fasciitis (Shulman syndrome). Schweiz Med Wochenschr 2000;130:156-60.
[Google Scholar]
|
| 4. |
Antic M, Lautenschlager S, Itin PH. Eosinophilic fasciitis 30 years after - what do we really know? Report of 11 patients and review of the literature. Dermatology 2006;213:93-101.
[Google Scholar]
|
| 5. |
Jaratt M, Bybee JD, Ramsdell W. Eosinophilic fasciitis: An early variant of scleroderma. J Am Acad Dermatol 1979;1:221-6.
[Google Scholar]
|
Fulltext Views
3,079
PDF downloads
1,919





