Translate this page into:
Generalized multinucleate cell angiohistiocytoma with involvement of palms and soles: An unusual manifestation
Correspondence Address:
Suthinee Rutnin
Division of Dermatology, Faculty of Medicine, Ramathibodi Hospital, Mahidol University, 270 Rama VI Road, Ratchathewi, Bangkok, 10400
Thailand
| How to cite this article: Nimmannitya K, Jerasutus S, Rutnin S. Generalized multinucleate cell angiohistiocytoma with involvement of palms and soles: An unusual manifestation. Indian J Dermatol Venereol Leprol 2018;84:468-470 |
Sir,
We describe a case of a Thai male diagnosed with generalized multinucleate cell angiohistiocytoma, along with lesions presenting on palms and soles. Such a case has not been documented in the literature yet.
A healthy 42-year-old male presented with an 8-year history of multiple disseminated asymptomatic lesions on his trunk and extremities. The lesions began on his trunk which subsequently spread to the upper and lower extremities. Physical examination showed multiple dark-red-to-violaceous, dome-shaped papules of varying size, with a smooth surface, scattered on the trunk, arms and legs, including palms and soles [Figure - 1] and [Figure - 2]. The lesions developed slowly over the years with partial regression of some lesions. Rest of the physical examination was unremarkable. The initial clinical impressions were multiple angioma, multiple eruptive dermatofibroma, eruptive microvenular hemangioma and Kaposi's sarcoma. Biopsy from the lesion on his back demonstrated proliferation of thick-walled small blood vessels in association with scattered stellate fibroblasts, bizarre shaped and angulated cytoplasm of multinucleate giant cells, infiltrate of lymphocytes and plasma cells in the entire dermis [Figure - 3]. Overlying epidermis also showed hyperplasia and hyperpigmentation. Immunohistochemically, vascular endothelial cells expressed vimentin and CD34. Mononucleated spindle cells expressed vimentin and factor XIIIA but not CD68 and estrogen receptor. Multinucleate cells were positive for vimentin [Figure - 3], but negative for factor XIIIA, CD68 and estrogen receptor. HHV-8 stain was also negative. The final diagnosis of generalized multinucleate cell angiohistiocytoma was made. There was no evidence of other systemic disease. The patient was lost to follow-up.
 |
| Figure 1: Multiple scattered dome-shaped erythematous to violaceus papules on trunk and extremities |
 |
| Figure 2: The papules on palms and soles |
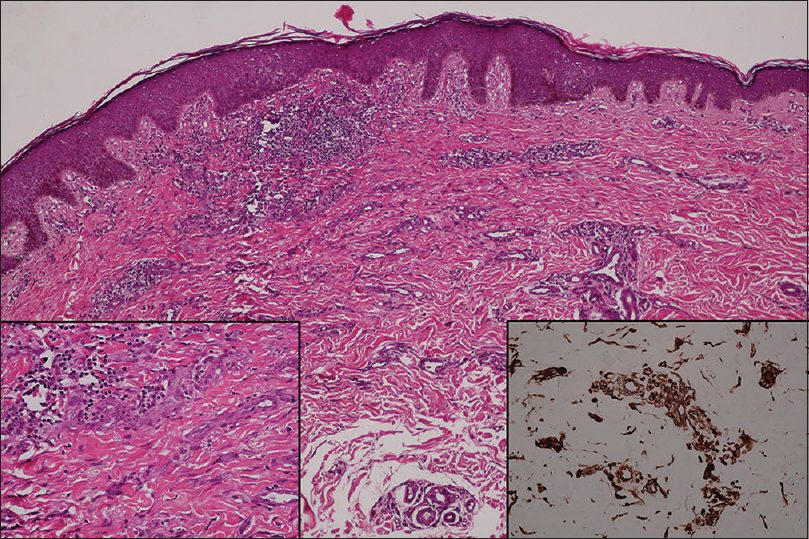 |
| Figure 3: Epidermal hyperplasia and hyperpigmentation with proliferation of thick-wall small blood vessels (H and E, ×100). Multinucleate cells with bizarre shaped and angulated cytoplasm (H and E, ×400, left inset), highlighted by vimentin (×400, right inset) |
Multinucleate cell angiohistocytoma was first described by Smith and Wilson-Jones in 1985. Since then, less than 150 cases have been reported in the literature with a female predominance.[1] It is a benign vascular proliferation of unknown pathogenesis, characterized by multiple, firm, circumscribed, red-to-violaceous papules often grouped on an anatomic area, particularly the limbs, in middle-aged to elderly woman. The lesions develop more frequently on the dorsal part of the hands or wrists. Less commonly, they occur on the face including eyelids and lip, mucosa and trunk.[1] Usually asymptomatic, some papules may be pruriginous. Linear, bilateral and generalized distribution have also been described.[2],[3] We found only 12 previous case reports of generalized multinucleate cell angiohistiocytoma.[3] It may be underdiagnosed owing to under-recognition by clinicians and pathologists. Our case also demonstrates the exceptional presentation on palms and soles. In generalized multinucleate cell angiohistiocytoma, no associations with other cutaneous or systemic disease have been reported.
Histology shows increase in dermal vessels, with prominent endothelial cells and enlarged lumina. The dermal collagen bundle can be thickened. Numerous spindle-shaped cells and multinucleate cells of bizarre shape and angulated cytoplasm are located within the dermis. A perivascular infiltration consisting of lymphocytes, occasional plasma cells and neutrophils can be present. Epidermal hyperplasia and hyperpigmentation may be present. Immunohistochemical finding are variable depending on the cases reviewed. Multinucleate cells tend to be positive for vimentin, variably positive for CD68 and occasionally factor XIIIa. Mononucleated spindle cells are positive for factor XIIIA and CD68 and are occasionally positive for vimentin and MAC387. The endothelial cells stain positively for vimentin, CD34 and factor VIII. A recent study also reported estrogen receptor alpha expression in multinucleate cell angiohistiocytoma, particularly in interstitial and perivascular spindle cells, and occasionally in multinucleate cells.[4] We found that the multinucleate cells do not stain with antibodies against factor XIIIa and CD68, which has been consistently reported in previous studies and might be related to their functional alteration or degeneration.[1]
Multinucleate cell angiohistiocytoma may be mistaken for other vascular proliferation or reactive conditions. The clinical differential diagnosis of multinucleate cell angiohistiocytoma includes dermatofibroma, microvenular hemangioma, angiofibroma, early Kaposi's sarcoma, and pseudo-Kaposi (acroangiodermatitis). Some can mimic granuloma annulare, lichen planus and even lymphocytoma.[5] For generalized multinucleate cell angiohistiocytoma, the differential diagnosis includes eruptive microvenular hemangioma, generalized eruptive histiocytoma, eruptive leiomyomas, eruptive dermatofibroma, lymphomatoid papulosis, papulonecrotic tuberculid, leukemia and lymphoma with cutaneous involvement.[3]
Multinucleate cell angiohistiocytoma has a benign course. The lesions show slow increase in size and number over the years. They generally persist indefinitely, although spontaneous regression was occasionally observed.[1] Most investigators have suggested an inflammatory or reactive process rather than a neoplasm. The ultrastructural morphology of multinucleate cells in combination with the positive immunohistochemical stain for vimentin and negative for monocyte-macrophage markers provide evidence for a fibroblastic origin, which is consistent with our finding revealing immunohistochemical expression of only vimentin in multinucleate cells.[3] Treatment is not generally recommended except for aesthetic reasons or for disseminated cases. In addition to surgical excision, successful treatment options are argon laser, carbon dioxide laser, cryosurgery, intense pulse light and pulsed-dye laser.[3]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given his consent for his images and other clinical information to be reported in the journal. The patient understand that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Frew JW. Multinucleate cell angiohistiocytoma: Clinicopathological correlation of 142 cases with insights into etiology and pathogenesis. Am J Dermatopathol 2015;37:222-8.
[Google Scholar]
|
| 2. |
Coco V, Guerriero C, Di Stefani A, Pennacchia I, Peris K. Linear and bilateral multinucleated cell angiohistiocytoma (MCAH). J Dermatol Case Rep 2016;10:58-61.
[Google Scholar]
|
| 3. |
Wang M, Abdul-Fattah B, Wang C, Zhao Y, Qu X, Al-Muriesh M, et al. Generalized multinucleate cell angiohistiocytoma: Case report and literature review. J Cutan Pathol 2017;44:125-34.
[Google Scholar]
|
| 4. |
Cesinaro AM, Roncati L, Maiorana A. Estrogen receptor alpha overexpression in multinucleate cell angiohistiocytoma: New insights into the pathogenesis of a reactive process. Am J Dermatopathol 2010;32:655-9.
[Google Scholar]
|
| 5. |
Cribier B, Gambini C, Rainero M, Grosshans E. Multinucleate cell angiohistiocytoma. A review and report of four cases. Acta Derm Venereol 1995;75:337-9.
[Google Scholar]
|
Fulltext Views
2,413
PDF downloads
1,869





