Translate this page into:
Giant eccrine porocarcinoma in an unusual location
2 Department of Plastic and Reconstructive Surgery, Faculty of Medicine, Celal Bayar University, Manisa, Turkey
3 Department of Dermatology, Bursa State Hospital, Bursa, Turkey
4 Department of Pathology, Faculty of Medicine, Celal Bayar University, Manisa, Turkey
Correspondence Address:
Aylin Türel Ermertcan
Department of Dermatology, Faculty of Medicine, Celal Bayar University, 45010 Manisa
Turkey
| How to cite this article: Ermertcan AT, Evrenos M K, Öztürk F, Temiz P. Giant eccrine porocarcinoma in an unusual location. Indian J Dermatol Venereol Leprol 2018;84:521 |
Sir,
Eccrine porocarcinoma, also known as malignant eccrine poroma, is an extremely rare type of skin cancer arising from the intraepidermal ductal portion of eccrine sweat glands.[1],[2] Lesions of eccrine porocarcinoma occur on the lower extremities in 60% of cases. Typically, these tumors arise in midlife occurring equally in males and females and have been observed in all races. They are characterized clinically as firm asymptomatic nodules, erythematous to violaceous in color and are usually <2 cm in size.[3] The differential diagnosis of the disease includes basal cell and squamous cell carcinoma, pyogenic granuloma, nevus, verruca vulgaris and melanoma. Dermoscopy should be of value in the differential diagnosis of these lesions. If there is suspicion of eccrine porocarcinoma, the biopsy of choice should be excisional. A local recurrence rate after wide excision of 20%, a distant metastasis rate of 12% and a mortality rate of >50% have been reported with this tumor. Early diagnosis of this tumor is essential to ensure a benign course.[4]
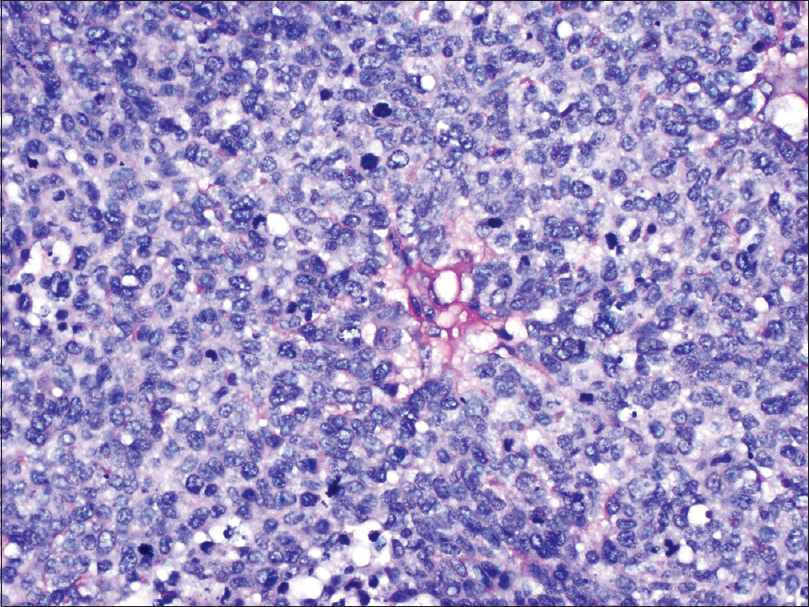
An 87-year-old woman applied to our outpatient clinic with the complaint of a red painless mass on the cheek for 6 months. She explained that her mass had grown rapidly in the last month. On dermatological examination, a pink, shiny tumor 4 cm × 4 cm in size was observed on her right cheek [Figure - 1]. According to clinical view, we considered squamous cell carcinoma or amelanotic melanoma first. Dermoscopic examination revealed large, brownish-red, whitish and yellowish structureless areas in the central part, white scaling and linear and dotted irregular vessels at the periphery [Figure - 2]. Our dermoscopic diagnosis was amelanotic melanoma. Hence, we referred the patient for total excision of the lesion to the Department of Plastic and Reconstructive Surgery. Wide local excision was performed with 1 cm margin by surgeons and the defect was closed primarily. On histopathological examination, a tumor showing continuity with its ulcerated epidermis was revealed. The tumor was characterized by broad anastomosing epithelial trabeculae with comedo necrosis [Figure - 3]. The tumor had a pushing margin at the lower border. Ductal differentiation and intracytoplasmic lumen formation were observed [Figure - 4]. The tumor cells had pleomorphism and brisk mitotic activity [Figure - 5]. Ductal and luminal structures were highlighted with carcinoembryonic antigen and periodic acid–Schiff positivity [Figure - 6] and [Figure - 7]. Epithelial membrane antigen and cytokeratin 7 were focal positive in tumor cells [Figure - 8] and [Figure - 9].
 |
| Figure 1: Pink, shiny nodule with erythema, crusting and scaling 4 cm × 4 cm in size on the right cheek |
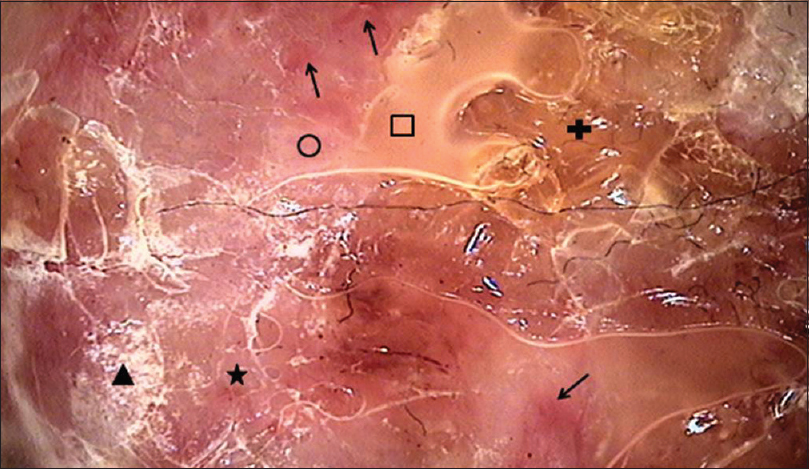 |
| Figure 2: Brownish-red (plus shape), whitish (circle shape) and yellowish (box shape) structureless areas at the central part; white scaling (triangle shape), linear (arrows) and dotted (star shape) irregular vessels at the periphery, MoleMax 3 (computerized digital dermoscopy system), ×40 |
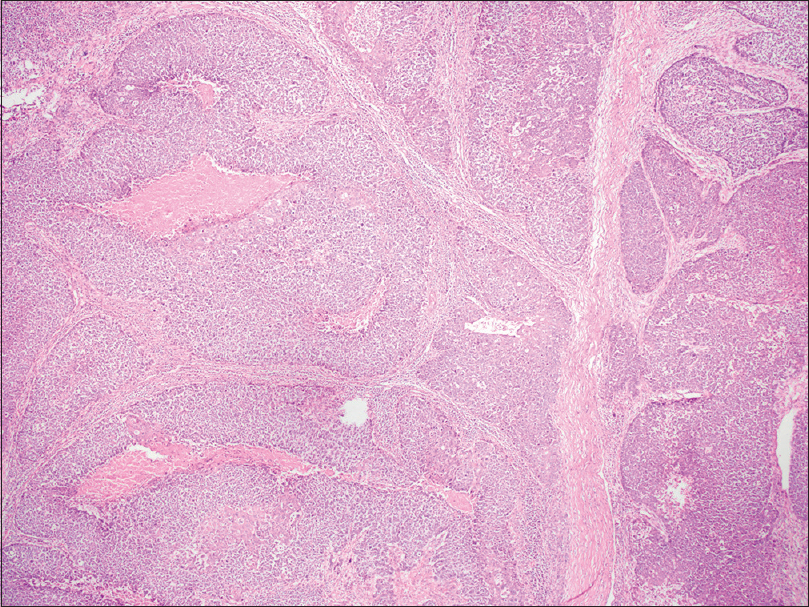 |
| Figure 3: The broad anastomosing epithelial trabeculae with comedo necrosis in tumor (H and E, ×400) |
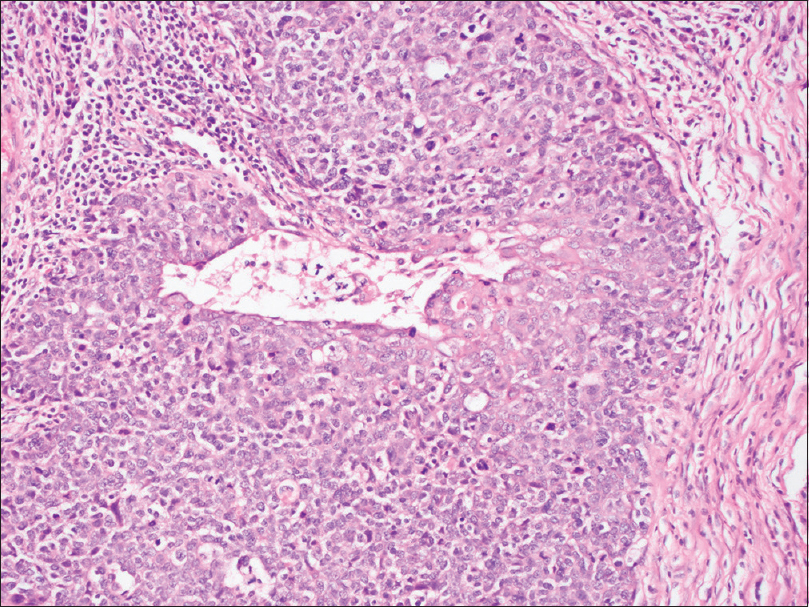 |
| Figure 4: Intracytoplasmic luminae in tumor cells (H and E, ×100) |
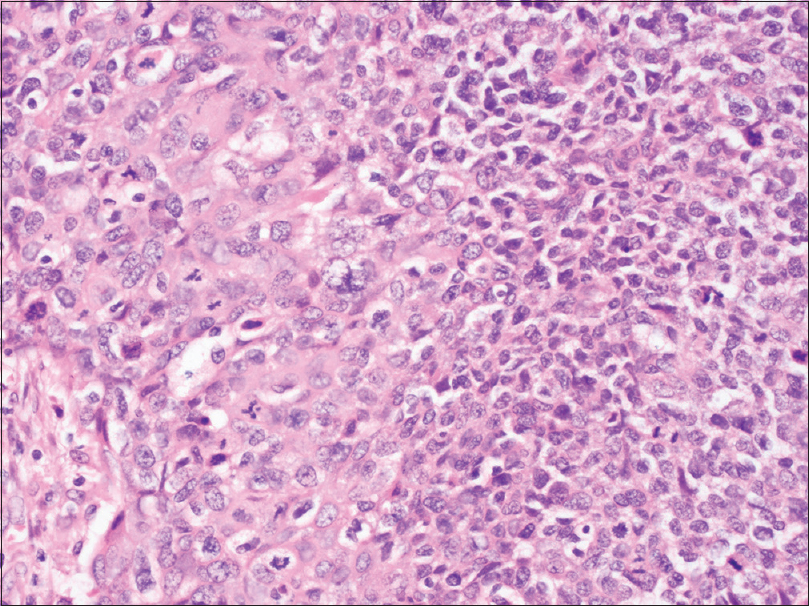 |
| Figure 5: Pleomorphism and mitotic activity in tumor cells (H and E, ×200) |
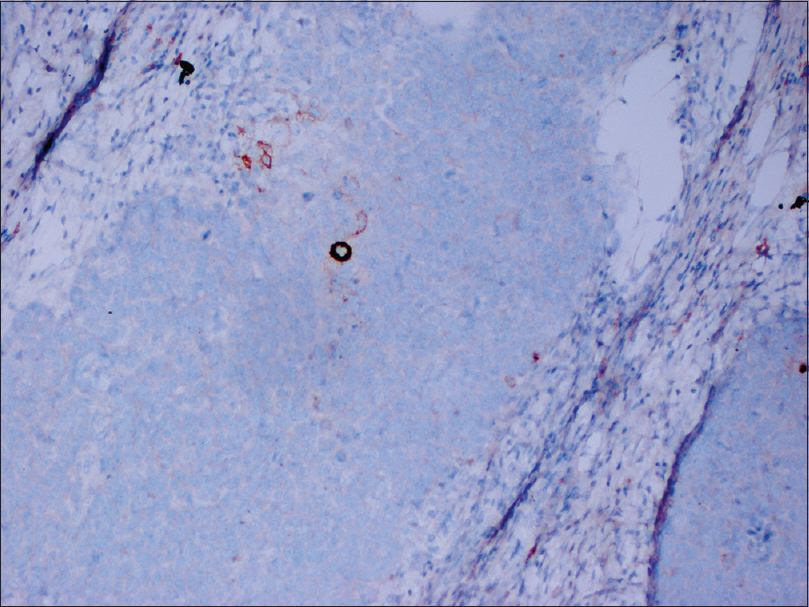 |
| Figure 6: Carcinoembryonic antigen positivity shows ductal differentiation (×100) |
 |
| Figure 7: Periodic acid–Schiff positivity in the luminal border of the tumoral duct (×200) |
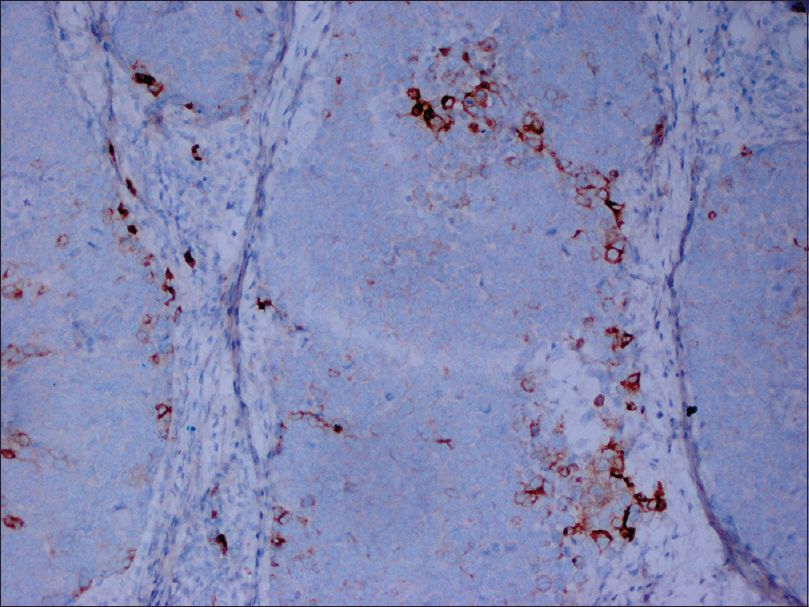 |
| Figure 8: Focal epithelial membrane antigen positivity in tumor cells (×100) |
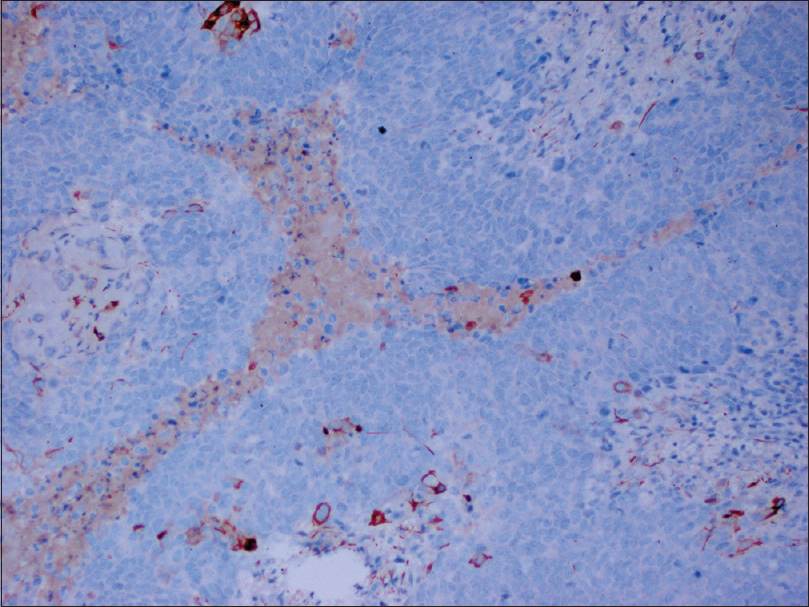 |
| Figure 9: Focal cytokeratin 7 positivity in tumor cells (×100) |
According to the dermoscopic and histopathological findings, the diagnosis was eccrine porocarcinoma. On radiological examination, regional or distant metastasis was not detected with positron emission tomography scan immediately after diagnosis and monthly performed clinical and cervical ultrasonographic examinations during 6 months' follow-up period.
Poroid neoplasms represent a spectrum of adnexal tumors arising from the intraepidermal portion of the eccrine sweat glands, ranging from benign lesions (hidroacanthoma simplex, poroma and dermal duct tumor) to high-grade malignant carcinomas, termed porocarcinomas. Although eccrine poromas are benign lesions, cases of eccrine porocarcinoma arising on long-standing and untreated eccrine poroma suggest a certain risk of malignant transformation.[5] The clinical appearance is non-specific and a majority of tumors are diagnosed histologically. The lesion often has a pink, moist, shiny surface which can offer a diagnostic clue. It may also appear as a nodule, a dome-shaped, infiltrated or erosive plaque or with polypoidal growth that tends to ulcerate. The tumor usually grows slowly, but it may often show an accelerated growth phase.[6]
Dermoscopy is an essential technique in the diagnosis of pigmented and non-pigmented skin tumors. However, some cases of eccrine porocarcinoma have been reported using dermoscopic images.[2],[5],[7] Pink-white structureless areas and atypical polymorphous vascular pattern mainly consisting of hairpin, linear, glomerular and dotted vessels have been reported as specific dermoscopical findings for the diagnosis of eccrine porocarcinoma.[2],[7] Suzaki et al. mentioned that vessels were more conspicuous and irregular in the eccrine porocarcinoma compared with eccrine poroma. Although it would be difficult to differentiate amelanotic melanoma from eccrine porocarcinoma on dermoscopy alone, the peripheral findings suggesting eccrine poroma, such as whitish structureless area, might be helpful for a diagnosis of eccrine porocarcinoma.[7]
We also observed that yellowish structureless areas and white scaling just represent crusting over the tumor as a non-specific finding on the dermoscopic examination.
The diagnosis of eccrine porocarcinoma is based on histological confirmation. The treatment of eccrine porocarcinoma remains challenging. Most patients are managed by wide local excision. In the last few years, it has been demonstrated that Mohs micrographic surgery may be superior to the standard wide local excision.[8] We performed wide local excision of the tumor and we confirmed the diagnosis of eccrine porocarcinoma with histopathological findings. [Figure - 10] shows the clinical appearance of the patient 6 months after surgery.
 |
| Figure 10: Clinical view of the patient 6 months after surgery |
Eccrine porocarcinoma should be kept in mind in the differential diagnosis of a pink to reddish nodule with an atypical vascular pattern on dermoscopic examination. We suggest that besides pink-white structureless areas and atypical polymorphous vascular pattern, yellowish structureless areas and white scaling can be observed as dermoscopic features of eccrine porocarcinoma.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Song SS, Wu Lee W, Hamman MS, Jiang SI. Mohs micrographic surgery for eccrine porocarcinoma: An update and review of the literature. Dermatol Surg 2015;41:301-6.
[Google Scholar]
|
| 2. |
Edamitsu T, Minagawa A, Koga H, Uhara H, Okuyama R. Eccrine porocarcinoma shares dermoscopic characteristics with eccrine poroma: A report of three cases and review of the published work. J Dermatol 2016;43:332-5.
[Google Scholar]
|
| 3. |
Brown CW Jr., Dy LC. Eccrine porocarcinoma. Dermatol Ther 2008;21:433-8.
[Google Scholar]
|
| 4. |
Johr R, Saghari S, Nouri K. Eccrine porocarcinoma arising in a seborrheic keratosis evaluated with dermoscopy and treated with Mohs' technique. Dermatol Surg 2003;42:653-7.
[Google Scholar]
|
| 5. |
Sgouros D, Piana S, Argenziano G, Longo C, Moscarella E, Karaarslan IK, et al. Clinical, dermoscopic and histopathological features of eccrine poroid neoplasms. Dermatology 2013;227:175-9.
[Google Scholar]
|
| 6. |
Sharathkumar HK, Hemalatha AL, Ramesh DB, Soni A, Revathi V. Eccrine porocarcinoma: A case report. J Clin Diagn Res 2013;7:2966-7.
[Google Scholar]
|
| 7. |
Suzaki R, Shioda T, Konohana I, Ishizaki S, Sawada M, Tanaka M. Dermoscopic features of eccrine porocarcinoma arising from hidroacanthoma simplex. Dermatol Res Pract 2010;2010:192371.
[Google Scholar]
|
| 8. |
Xu YG, Aylward J, Longley BJ, Hinshaw MA, Snow SN. Eccrine porocarcinoma treated by Mohs micrographic surgery: Over 6-year follow-up of 12 cases and literature review. Dermatol Surg 2015;41:685-92.
[Google Scholar]
|
Fulltext Views
2,593
PDF downloads
2,808





