Translate this page into:
Giant linear syringocystadenoma papilliferum of the back
2 Department of Medicine, Midnapur Medical College, West Bengal, India
3 Department of Gynaecology and Obstetrics, Burdwan Medical College, Burdwan, West Bengal, India
Correspondence Address:
Jugal K Kar
B-13 Keranitola, Singha Compound, Paschim Medinipur, West Bengal - 721 101
India
| How to cite this article: Kar M, Kar JK, Maiti S. Giant linear syringocystadenoma papilliferum of the back. Indian J Dermatol Venereol Leprol 2012;78:123 |
Sir,
Syringocystadenoma papilliferum (SCAP) is a rare benign hamartomatous adnexal tumor of the apocrine or eccrine sweat glands. Most patients present with a solitary lesion in the head and neck region. Presentation with multiple lesions is rare, and in those arising outside the head and neck region is even more uncommon. We present a case of SCAP with multiple papulonodular lesions arranged in a linear fashion and located on the lower back.
A 12 year-old boy had four asymptomatic discrete skin-colored papular lesions on the lower back since birth, and they had gradually increased in number and size over the years. They were conglomerated and presented as a single linear lesion. No other cutaneous or systemic complaints were reported. Some local medications were applied but the lesions never subsided.
On examination, a 20-cm-long and 7-cm wide fleshy cauliflower-like erythematous papulonodular lesion arranged in a linear array transversely on the lower back of the boy with obvious increase in vascularity and oozing of sero-sanguinous fluid [Figure - 1] was seen. It had about a 2-cm-wide long narrow pedicle. Some nodules measured up to 1.5 cm in diameter and some of them had surface erosion. The surrounding skin was normal. The base was not indurated and the lesion was not fixed to the deeper fascia and muscles. There was no regional lymphadenopathy. No other skin lesions were noted elsewhere. Although the morphologic profile of the tumor was distinctive, squamous cell carcinoma and basal cell carcinoma of the skin were borne in our mind during the diagnosis. Biopsy from the lesions showed the classical features of SCAP, i.e. epithelial invaginations into the dermis with papillary projections and plasma cells infiltration [Figure - 2].
 |
| Figure 1: Fleshy cauliflower-like papulonodular lesions of syringocystadenoma papilliferum arranged in a linear array on the lower back of the boy with obvious increase in vascularity and oozing of sero-sanguinous fluid |
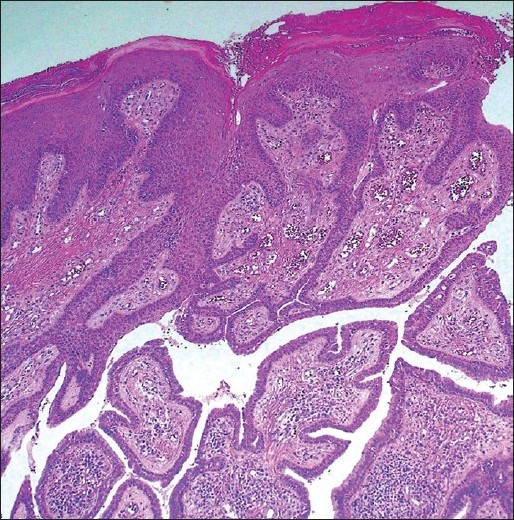 |
| Figure 2: Photomicrograph showing epithelial invaginations into the dermis with papillary projections and plasma cells infiltration (H and E, ×100) |
He was operated under general anesthesia in a prone position. The lesion was excised completely with a normal skin margin of 0.5 cm and depth up to the subcutaneous plane. The skin was closed primarily with undermining of the surrounding skin. The stitches were removed after 2 weeks without gaping and the wound healed completely at 6 weeks. He was followed-up for one and a half years with no recurrence and good cosmetic recovery.
Interestingly, the first case of SCAP was described on the thigh by Stokes in 1917 under the term nevus syringadenomatosus papilliferus. [1] But, SCAP occurs most commonly in the head and neck region, de novo or associated with nevus sebaceous. Uncommon sites of occurrence include chest, arms, breast, eyelids, axilla, scrotum, lower limb and inguino- perineal regions. SCAP is very rare on the back. It is usually first noted at birth or during early childhood, consisting of either one papule, several papules in a linear arrangement or a solitary plaque. At puberty, SCAP may increase in size and become papillomatous and crusted. [2] Most of these are sporadic cases, diagnosed on histopathology, clinical presentation being nonspecific and sometimes misleading. Basal cell carcinomas may occur in up to 10% of the cases. [2]
SCAP is typified microscopically by endophytic invaginations of the epithelium into the dermis. These are duct-like structures leading into the dermal cystic spaces. Papillary projections of variable shape and size protrude into the lumen of these spaces. These are lined by double-layered outer cuboidal and luminal high-columnar epithelium, but these are not unique to this tumor type. Dilated capillaries and a dense infiltrate of plasma cells are noted in the stroma of these papillary projections. Tumor cells show a positive staining reaction with carcinoembryonic antigen and gross cystic disease fluid protein-15. [3]
Syringocystadenocarcinoma papilliferum is the malignant counterpart, characterized by solid areas and cytologically malignant cells. [4]
The treatment is surgical excision, and CO 2 laser may be effective in removing tumors on anatomic sites unfavorable to surgical excision. [3],[5]
| 1. |
Stokes JH. A clinico-pathologic study of an unusual cutaneous neoplasm combining nevus syringadenomatosus papilliferus and a granuloma. J Cutan Dis 1917;35:411-9.
[Google Scholar]
|
| 2. |
Pahwa P, Kaushal S, Gupta S, Khaitan BK, Sharma VK, Sethuraman G. Linear syringocystadenoma papilliferum: An unusual location. Pediatr Dermatol 2011;28:61-2.
[Google Scholar]
|
| 3. |
Malhotra P, Singh A, Ramesh V. Syringocystadenoma papilliferum on the thigh: An unusual location. Indian J Dermatol Venereol Leprol 2009;75:170-2.
[Google Scholar]
|
| 4. |
Narang T, De D, Dogra S. Linear papules and nodules on the neck. Arch Dermatol 2008;144:1509-14.
[Google Scholar]
|
| 5. |
Yap FB, Lee BR, Baba R. Syringocystadenoma papilliferum in an unusual location beyond the head and neck region: A case report and review of literature. Dermatol Online J 2010;16:4.
[Google Scholar]
|
Fulltext Views
3,188
PDF downloads
3,538





