Translate this page into:
Giant, mutilating facial lupus vulgaris due to long-term misdiagnosis
Corresponding Author:
Li Li
Department of Dermatology, West China Hospital, Sichuan University, Chengdu, Sichuan 610 041
China
lily2058@126.com
| How to cite this article: Xue L, Li W, Lv X, Li L. Giant, mutilating facial lupus vulgaris due to long-term misdiagnosis. Indian J Dermatol Venereol Leprol 2017;83:412 |
Sir,
Cutaneous tuberculosis is an uncommon disease in many parts of the world. We report the case of an elderly man with giant, mutilating facial lupus vulgaris which was misdiagnosed for 42 years.
A 54-year-old farmer presented with a 42-year history of a non-healing mutilating plaque on his face which was triggered by trauma. At presentation, he had a well-marginated, large, dark red plaque, predominantly involving the left side of his face with overlying telangiectases, scaling and scarring, predominantly involving the left side of his face [Figure - 1]. The left eyebrow was sparse, he had left-sided facial paralysis and could not shut his left eye. Both eyes showed conjunctival congestion and decreased visual acuity. The nasal bridge was collapsed with bilateral nasal atrophy and most of the left pinna had disappeared. He had lost his hearing in the left ear 14 years earlier. He had been diagnosed to have conjunctivitis, otitis media and facial dermatitis at various local hospitals but the suggested treatments did not work. He had no other illnesses or any known contact with tuberculosis.
 |
| Figure 1: (a) Large red plaque involving the whole face. (b) Most of the left pinna had disappeared. (c) Resolving lesion after treatment. (d) The ear healed partially |
The hearing test showed moderate sensori-neural deafness in the right ear and severe mixed deafness in the left ear. Ear endoscopy revealed a perforated eardrum in the left ear indicating chronic otitis. The corrected visual acuity was 0.8 and 0.7 for the right and left eyes, respectively. Ophthalmologic evaluation including intraocular pressure, fundoscopy, fundus fluorescein angiography and optical coherence tomography showed no significant abnormalities. The facial nerve function was graded as House–Brackmann grade IV. Nasal endoscopy revealed septal deviation to the left. Complete blood counts, liver and kidney functions, fungal culture of skin samples and computed tomography of the chest did not show any abnormalities. Skin biopsy of the right cheek showed epidermal atrophy and epithelioid cell granulomas with Langhans giant cells and lymphocytic infiltration in the dermis [Figure - 2]. Silver stain, acid-fast stain and periodic acid-Schiff stain were all negative. The tuberculin skin test was strongly positive (20 mm). Qualitative polymerase chain reaction could detect deoxyribonucleic acid fragments of Mycobacterium tuberculosis in the tissues of the right jaw and cheek.
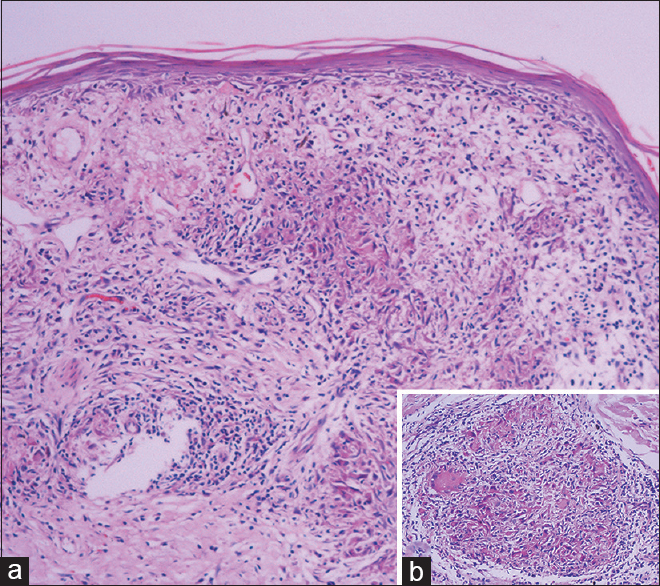 |
| Figure 2: (a) Epidermal atrophy and granulomas in the dermis and (b) epithelioid granulomas with Langhans giant cells (a: H and E, ×40 and b: H and E, ×100) |
Based on the clinical and investigative findings, a diagnosis of lupus vulgaris was made and the patient was treated for 6 months with isoniazid 300 mg daily, rifampicin 450 mg twice weekly, ethambutol 750 mg daily and pyrazinamide 1500 mg daily. The facial plaque almost disappeared after treatment, though mutilation remained. The House–Brackmann grade of facial nerve function improved to III. The sensori-neural hearing loss in the right ear improved from moderate to mild but severe mixed deafness in the left ear persisted. The corrected visual acuity improved to 0.9 and 0.8 for the right and left eyes, respectively. The patient has been following up regularly till date.
Lupus vulgaris is a common type of cutaneous tuberculosis usually caused by hematogenous or lymphatic spread or spread from underlying tuberculosis of an internal organ. Exogenous inoculation by trauma has also been reported.[1] It is important to diagnose lupus vulgaris early because it can result in chronic disfigurement.[2-4] Our patient had a prolonged disease course of 42 years due to misdiagnosis resulting in serious facial mutilation which is very rare in clinical practice. The patient's skin lesion, vision, hearing and facial paralysis improved after anti-tubercular therapy. However, facial mutilation persisted.
Long-term misdiagnosis in our patient might have occurred due to the following reasons: (1) as he lived in a mountainous area, he could not visit a doctor regularly; (2) he had an atypical presentation of lupus vulgaris which could have been easily misdiagnosed as sarcoidosis, discoid lupus erythematosus, deep fungal disease, tuberculoid leprosy or hemangioma; (3) local physicians' knowledge of rare diseases could have been limited, and the findings were perhaps inadequate to make a conclusive diagnosis.[5]
Complete history taking, skin biopsy, tuberculin skin test and qualitative polymerase chain reaction are vital to avoid misdiagnosis or delayed diagnosis and the resultant preventable but irreversible complications. A therapeutic trial of anti-tubercular therapy should be considered when the disease is complicated and tuberculosis is suspected or if no improvement is observed with conventional treatment.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has given his consent for his images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. | van Zyl L, du Plessis J, Viljoen J. Cutaneous tuberculosis overview and current treatment regimens. Tuberculosis (Edinb) 2015;95:629-38. [Google Scholar] |
| 2. | Singal A, Arora R, Pandhi D. Lupus vulgaris leading to perforation of nasal septum in a child. Indian Dermatol Online J 2015;6:196-7. [Google Scholar] |
| 3. | Pilani A, Vora RV. Lupus vulgaris: Unusual presentation on face. Indian J Lepr 2014;86:61-4. [Google Scholar] |
| 4. | Ng How Tseung KS, Zhao JJ, Jia YR, Keyal U, Bhatta AK. Giant facial cutaneous tuberculosis. Indian J Dermatol Venereol Leprol 2015;81:95. [Google Scholar] |
| 5. | Yaldiz M, Erdem T, Dikicier BS, Dilek FH. Lupus vulgaris mimicking hemangioma diagnosed 42 years after onset: A case report. J Med Case Rep 2015;9:215. [Google Scholar] |
Fulltext Views
3,027
PDF downloads
2,118





