Translate this page into:
Giant purplish tumour on the leg of a healthy woman
Corresponding author: Dr. Ivânia Soares, Department of Dermatology, Lisbon North Hospital Center, Santa Maria Hospital, Av. Professor Egas Moniz, Lisbon, Portugal. ivaniaalexsoares@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Soares I, De Vasconcelos P, Filipe PL. Giant purplish tumour on the leg of a healthy woman. Indian J Dermatol Venereol Leprol. 2024;90:829-30. doi: 10.25259/IJDVL_1074_2023
A 32-year-old woman, with skin phototype III, presented with concerns regarding the progressive growth of a mass on her left leg for six months. The lesion intermittently exhibited exudation. Upon clinical assessment, an indurated purplish tumour measuring 5 × 3 cm was discerned on the left anterior shin [Figure 1]. Additionally, the patient reported pain associated with a marked increase in the lesion’s size over the past month. She denied any family history of cutaneous neoplasms. A complete surgical excision was done and the subsequent histopathological analysis showed a moderately cellular, poorly demarcated, dermal, fibrohistiocytic proliferation with peripheral cytoplasmic deposits [Figures 2a and 2b]. Perl’s stain was intensely positive [Figure 2c].
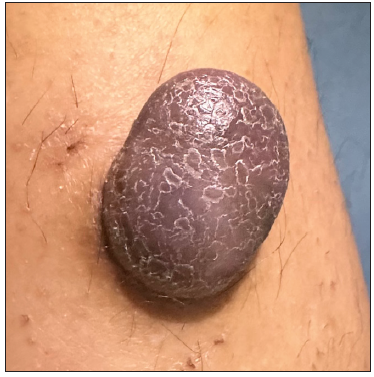
- Purple exophytic scaly tumour (5 × 3 cm) on the left lower leg.
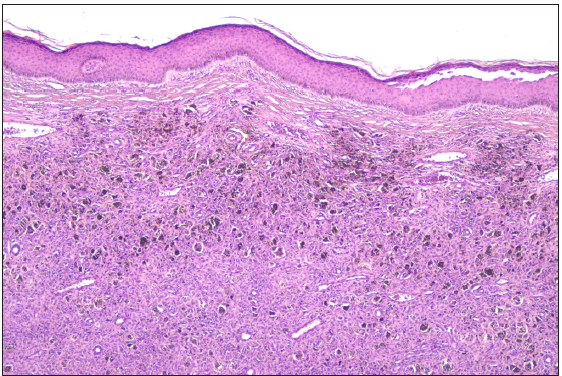
- Intradermal cellular proliferation of fusiform fibrohistiocytic cells. (Haematoxylin & eosin, 40x).
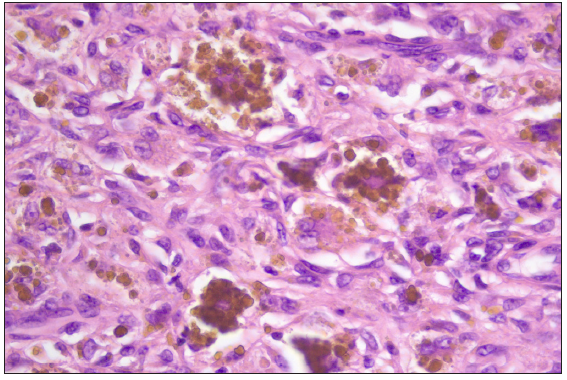
- Intracellular and interstitial hemosiderin deposits. (Haematoxylin & eosin, 400x).
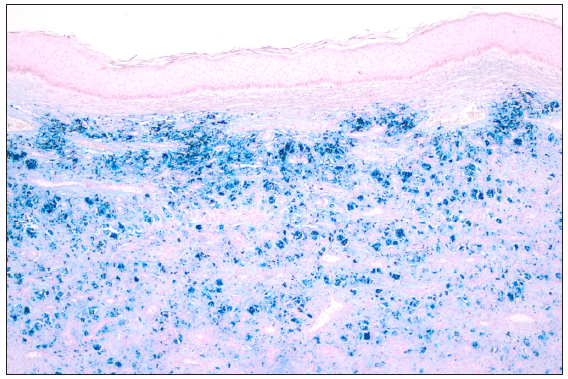
- Positive Perls’ staining. (40x).
Question
What is the diagnosis?
Answer
Giant haemosiderotic histiocytoma.
Discussion
Haemosiderotic histiocytoma (HH) is a variant of dermatofibroma, a benign dermal tumour which is not a rare subtype. However, the interesting point about this case is the large size thus qualifying for a giant haemosiderotic DF, which is indeed extremely rare. The unusual size (5 cm or above), pedunculated appearance (not always present), and classical histopathologic features of dermatofibroma confirmed the diagnosis.1
Since it must be differentiated from other skin and soft tissue neoplasms, it is important to consider clinical, histopathological, and eventually immunohistochemical features. In our case, immunohistochemistry was not performed, but Perls stain was done, which was intensely positive [Figure 2c]. These findings ruled out melanocytic origin and concluded the tumour to be of fibrohistiocytic nature.
Giant HH typically manifests as a slow-growing, solitary nodule most commonly observed on the lower extremities of women. Clinically, it poses a diagnostic challenge due to its resemblance to melanoma, malignant soft tissue tumours, and other vascular lesions. Thus, a meticulous approach to diagnosis is imperative, incorporating both clinical evaluation and histopathological examination.2
Histopathologically, HH is characterised by a proliferation of histiocytic cells and spindle-shaped fibroblasts within a hemosiderin-rich stroma. The presence of hemosiderin-laden macrophages is a hallmark feature, which can be identified through histochemical staining, such as the Perls Prussian blue reaction or immunohistochemical staining for CD68 and Factor XIIIa.3
Differential diagnosis of HH includes nodular melanoma, vascular lesions such as Kaposi sarcoma or angiokeratoma, and other fibrohistiocytic tumours like dermatofibroma protuberans. Distinguishing HH from nodular melanoma is paramount due to their differing clinical courses and management strategies. Careful assessment of cytologic atypia, mitotic activity, immunohistochemical, and special staining patterns helps delineate between the two entities.
Moreover, understanding the relationship between HH and its variants, such as aneurysmal fibrous histiocytoma (AFH), is crucial. While HH is generally considered benign with a low risk of recurrence, AFH presents a higher risk of local non-destructive recurrence, Thus, recognising this spectrum of lesions aids in appropriate patient management and prognostication.4
In conclusion, HH represents a unique diagnostic challenge owing to its clinical mimicry of melanoma and difficulty in differentiation from other cutaneous lesions such as AFH. Awareness of the clinical and histopathological features and immunohistochemical staining patterns can improve diagnostic accuracy and allow better clinical decision-making.
Acknowledgement
The author would like to thank to Dr. Miguel Duarte Reis and Professor Dr. Luís Soares de Almeida.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of AI-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Giant haemosiderotic dermatofibroma: The largest giant dermatofibroma reported to date. Am J Dermatopathol. 2015;37:778-82.
- [CrossRef] [PubMed] [Google Scholar]
- Unusual variants of malignant melanoma. Mod Pathol. 2006;19:41-70.
- [CrossRef] [PubMed] [Google Scholar]
- Histiocytic tumors. In: Bolognia JL, Schaffer JV, Cerroni L, eds. Dermatology (4th ed). Elsevier; 2018. p. :2069-72.
- [Google Scholar]
- Giant aneurysmal benign fibrous histiocytoma (dermatofibroma) J Cutan Pathol. 2018;45:774-6.
- [CrossRef] [PubMed] [Google Scholar]





