Translate this page into:
Giant squamous cell carcinoma
Corresponding author: Dr. Shailesh Mohanbhai Kantaria, Kantaria Skin Clinic, Yuganda Road, Porbandar, Gujarat, India. kantariashailesh@yahoo.in
-
Received: ,
Accepted: ,
How to cite this article: Kantaria SM. Giant squamous cell carcinoma. Indian J Dermatol Venereol Leprol 2022;88:652-3.
Sir,
A 42-year-old man, a labourer working in the paint manufacturing industry, presented with a large, slowly progressive lesion on his abdomen of four years duration. The lesion started as an ulceration, for which he was treated at a surgical hospital with no improvement. Since he was relatively asymptomatic and could not afford treatment, the lesion was left uninvestigated and untreated. He did not have any systemic complaints. There was no history of tuberculosis or any known exposure to tuberculosis. He had no other significant medical history. There was no relevant family history. Routine laboratory tests were normal. Serological tests for HIV and the Mantoux test were negative. On examination, there was an erythematous, ulcerated and crusted plaque of 30 × 50 cm size on his abdomen [Figure 1]. It showed atrophy and signs of healing at one end. There was no regional lymphadenopathy. Clinical differentials of lupus vulgaris, deep mycoses and squamous cell carcinoma were considered. An incisional skin biopsy was done from an active margin. Multiple sections of the tissue were studied. The histopathological examination showed nests of mature squamous cells showing mild atypia. Several horn pearls (foci composed of concentric layers of squamous cells with gradually increasing keratinization towards the centre) were present [Figure 2]. There was no granulomatous inflammation to suggest lupus vulgaris. Based on typical histopathological findings, a diagnosis of well-differentiated squamous cell carcinoma was made, and the patient was referred to the oncology department for further evaluation and treatment.

- Giant ulcerated plaque with crusting on the abdomen
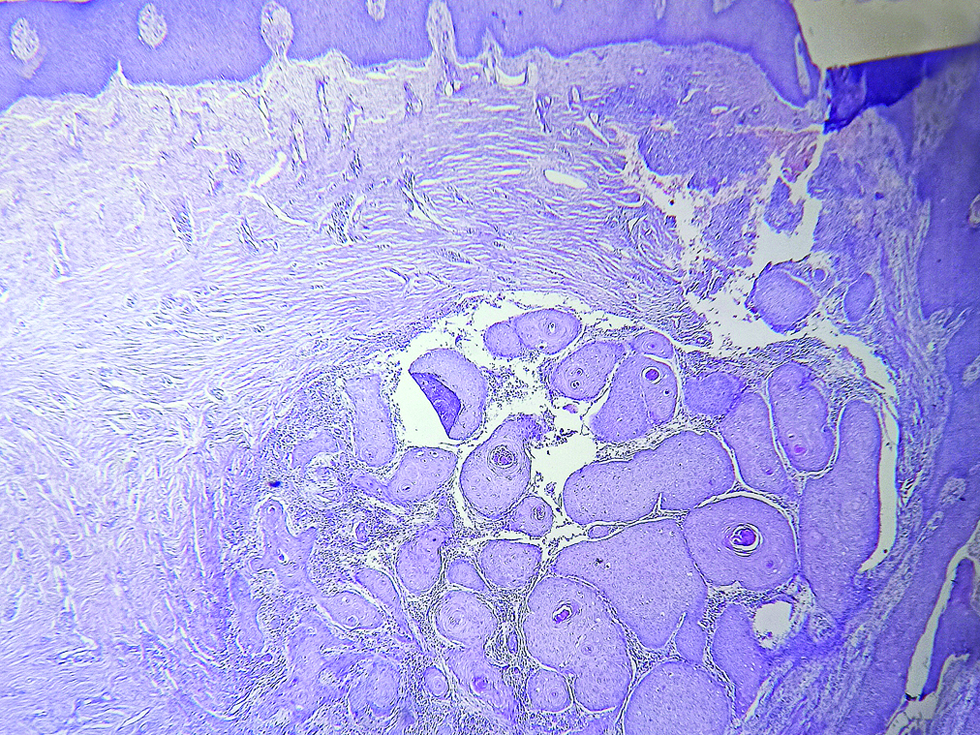
- Horn pearls composed of concentric layers of squamous cells with gradually increasing keratinization towards the centre (hematoxylin and eosin, × 100)
Occupational skin cancer often arises on the exposed areas among workers in chemical industry.1 The patient was working in the paint manufacturing industry, but the lesion was on the abdomen and not on any exposed parts. So the squamous cell carcinoma in his case may not have occurred because of exposure to paint. There was no history of any other predisposing factors like exposure to radiation, chronic friction or application of heating pads. He could not recall any history of trauma. The ulceration on the abdomen was left untreated for a long time and the persistence of infection or chronic inflammation could have been the cause of malignant transformation in this patient. Though there was no evidence suggestive of lupus vulgaris, Bowen disease, actinic keratosis or any other premalignant condition, malignant transformation of any premalignant skin lesion cannot be ruled out because the patient presented very late and biopsy was not done earlier. There are many case reports of squamous cell carcinoma, but the author was unable to find any previous reports of similar presentation of such giant cutaneous squamous cell carcinoma.
Cutaneous squamous cell carcinoma is a malignant tumour arising from keratinocytes of the epidermis. Squamous cell carcinoma may arise de novo or may arise on pre-existing skin lesions such as lupus vulgaris, lupus erythematosus, lichen planus, porokeratosis of Mibelli, psoriasis, epidermolysis bullosa, epithelial nevus, granuloma inguinale, chromoblastomycosis, acne conglobata, hidradenitis suppurativa, lichen sclerosus et atrophicus, nevus sebaceous, scar tissue, sinuses and fistulae.2 Squamous cell carcinoma is the most frequent histological type of neoplasm identified in scars and wounds.3 Dermatologists should be aware of this kind of atypical presentation of squamous cell carcinoma. Squamous cell carcinoma is often asymptomatic and hence patients often present very late. Unlike basal cell carcinoma, cutaneous squamous cell carcinoma is associated with a substantial risk of metastasis. Therefore, non-healing lesions should be viewed with great suspicion and a biopsy should be performed to rule out malignant transformation. A high index of suspicion and early histological diagnosis help in preventing complications.
Declaration of patient consent
Patient consent is not required as the patient’s identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- The epidemiology of non-melanoma skin cancer: Who, why and what can we do about it. J Dermatol. 1995;22:853-7.
- [CrossRef] [PubMed] [Google Scholar]
- Squamous cell carcinoma on a preexisting plaque of neurodermatitis. Indian J Dermatol Venereol Leprol. 1986;52:99-100.
- [PubMed] [Google Scholar]
- Burn scar neoplasms: A literature review and statistical analysis. Burns. 2005;31:403-13.
- [CrossRef] [PubMed] [Google Scholar]





