Translate this page into:
Glimpses of gold: Unveiling the enigma of multiple lichen aureus
Corresponding author: Dr. Dipankar De, Department of Dermatology, Venereology and Leprology, Postgraduate Institute of Medical Education and Research (PGIMER), Chandigarh, India. dr_dipankar_de@yahoo.in
-
Received: ,
Accepted: ,
How to cite this article: Sharma A, De D, Chatterjee D. Glimpses of gold: Unveiling the enigma of multiple lichen aureus. Indian J Dermatol Venereol Leprol. 2025;91:S77-S78. doi: 10.25259/IJDVL_868_2023
Dear Editor,
A 53-year-old woman presented with a six-month history of multiple, mildly itchy, reddish-brown lesions on both legs. The lesions started appearing after four months of surgery for varicose veins and gradually increased in number over the next 4 months. On examination, there were multiple, well-defined, variably sized and shaped, reddish-brown papules and plaques on both legs ranging between 1 × 1 cm to the largest being 5 × 3 cm. The two most prominent plaques on her left leg showed a classic reddish-brown appearance surrounded by a yellowish-golden rim with the surface showing mild scaling forming a collarette at some places and punctate red to brown vascular structures [Figures 1a and 1b]. The surrounding skin showed signs of venous flares, such as dilated tortuous capillaries and veins on a generalised yellowish-to-brownish background. Dermoscopic examination revealed the presence of multiple discrete red dots and globules in a coppery brown background, serpentine vessels, reticular brown lines and subtle brown dots [Figure 2].
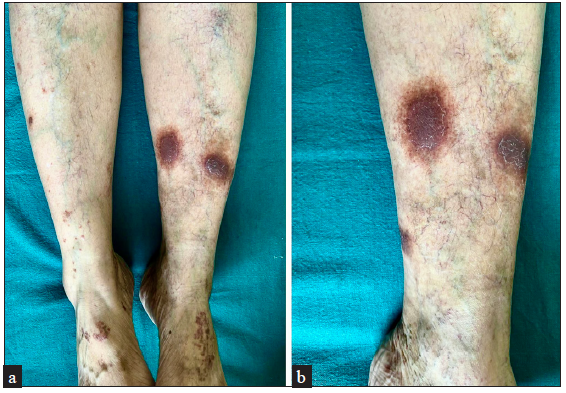
- Two prominent plaques showing a classic reddish-brown appearance surrounded by a yellowish-golden rim. Note the signs of venous flares surrounding these plaques.
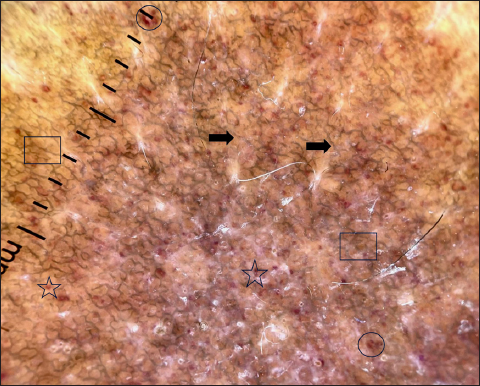
- Dermatoscopic examination revealed multiple discrete red dots (black star) and globules (black circle) on a coppery brown background, serpentine vessels (black arrows) and subtle brown dots (black square) (DermLite™ DL4;10x polarised mode).
A skin biopsy performed on one of the lesions for histopathological examination revealed epidermal hyperkeratosis, focal patchy parakeratosis with focal basal cell vacuolisation and lymphocytic exocytosis [Figure 3]. The upper dermis showed moderate lymphocytic inflammatory infiltrate, predominantly in the perivascular region. The dermal vessels had endothelial swelling, and extravasated red blood cells (RBCs) were noted in the upper dermis. No evidence of vasculitis was identified.
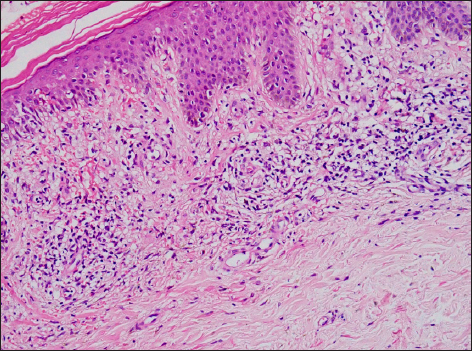
- Epidermal hyperkeratosis, focal basal cell vacuolisation and lymphocytic exocytosis. The upper dermis showed moderate lymphocytic inflammatory infiltrate, which was also seen in the perivascular location. Vessels showed endothelial swelling and extravasated RBCs (Haematoxylin and eosin, 100x).
Based on the clinical, dermatoscopic and histopathological findings, a diagnosis of multiple lichen aureus was made. Mid-potency topical steroid, once daily application, in combination with oral vitamin C supplementation and avoidance of prolonged standing, were suggested for treatment. The acute appearance of characteristic, rust-yellow or gold-coloured papules or circumscribed patches and plaques characterises lichen aureus. The name “lichen aureus” draws attention to the eruption’s traditional gold-brown hue. Notably, lesions that are copper-orange or violaceous may also be seen in lichen aureus. Unilateral lower extremity involvement is more common than bilateral involvement. 1 The lesions can appear in the upper extremities and trunk and can occur in segmental, dermatomal, and blaschkoid patterns. 2,3 The lesions can follow the course of superficial or deep veins. Aberrant distributions and patterns have been observed more frequently in children. 1
Multiple lichen aureus has been rarely reported. Torraca et al. 4 described a case of multiple segmental lesions of lichen aureus that evolved over six years. One of the possible factors for the multiplicity of lesions in our patient can be the presence of venous insufficiency. In a previous study by Kim et al. 5 venous insufficiency was detected in 35 of the 56 (62.5%) patients with pigmented purpuric dermatosis. Significant correlations were found between pigmented purpuric dermatosis and venous insufficiency. Longer duration of pigmented purpuric dermatosis, darker, and widespread lesions were seen in patients with established venous insufficiency.
Managing a case of widespread pigmented purpuric dermatosis in the presence of established venous insufficiency, when surgical management for venous insufficiency has already been tried without much improvement in lichen aureus, remains a challenge. Patients need counselling and an understanding of the interplay of various factors involved in the genesis of these skin lesions. Topical steroids, in combination with oral vitamin C supplementation, can be tried. Behavioural modifications, like intermittent sitting during hours of prolonged standing, elevation of limbs while sitting and interrupting the itch-scratch cycle, must be emphasised to the patients.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript, and no images were manipulated using AI.
References
- Segmental lichen aureus: Combination therapy with pentoxifylline and prostacyclin. J Eur Acad Dermatol Venereol. 2006;20:1378-80.
- [CrossRef] [PubMed] [Google Scholar]
- Segmental lichen aureus in a child. Int J Dermatol. 1991;30:654-5.
- [CrossRef] [PubMed] [Google Scholar]
- Segmental lichen aureus: An uncommon presentation. An Bras Dermatol. 2017;92:704-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Venous insufficiency is a clear provoker of pigmented purpuric dermatosis. Ann Dermatol. 2022;34:34-9.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]






