Translate this page into:
Granular parakeratosis presenting with facial keratotic papules
2 Consultant Dermatologist, Apollo Gleneagles Hospital, Kolkatta, India
Correspondence Address:
R Joshi
14 Jay Mahal, A Road, Churchgate, Mumbai - 400 020
India
| How to cite this article: Joshi R, Taneja A. Granular parakeratosis presenting with facial keratotic papules. Indian J Dermatol Venereol Leprol 2008;74:53-55 |
Abstract
A 27-year-old female presented with pruritic keratotic papules over the left side of the face since one month. The lesions developed a few days after working in a hot humid environment and were preceded by severe uncontrollable pruritus for which she had repeatedly wiped the area with handkerchiefs and towels. A biopsy from one of the keratotic papules revealed granular parakeratosis with a markedly thick stratum corneum that had parakeratosis and also housed keratohyaline granules. Similar changes were seen in keratotic plugs of dilated follicular infundibula. |
| Figure 3: Post inflammatory hyperpigmentation with complete subsidence of papules after two weeks |
 |
| Figure 3: Post inflammatory hyperpigmentation with complete subsidence of papules after two weeks |
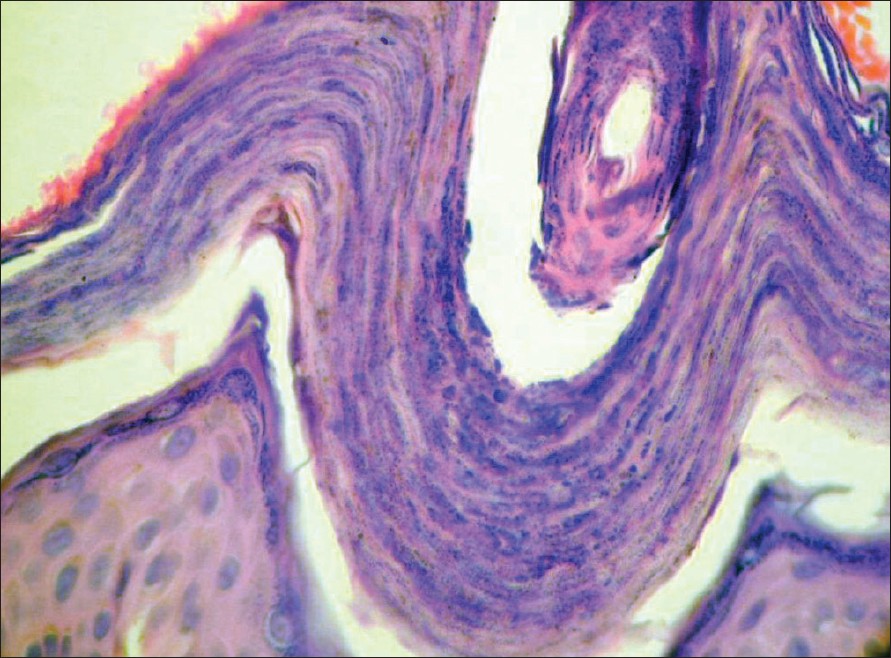 |
| Figure 2: Granular parakeratosis in follicular infundibulum (H and E stain, X400) |
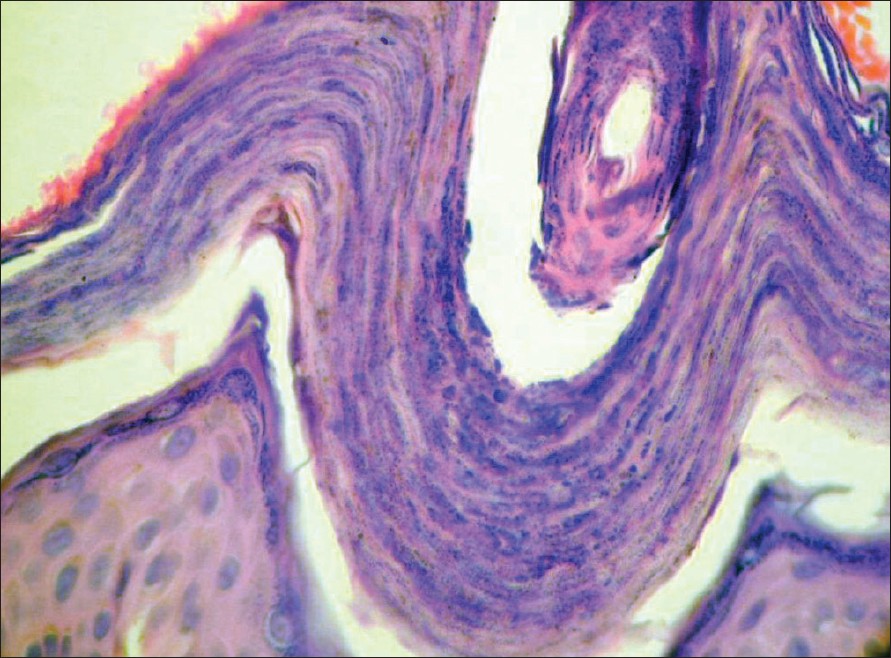 |
| Figure 2: Granular parakeratosis in follicular infundibulum (H and E stain, X400) |
 |
| Figure 1: Keratotic papules on the left side of the face at presentation |
 |
| Figure 1: Keratotic papules on the left side of the face at presentation |
Introduction
Axillary granular parakeratosis was first described by Northcutt et al ., in four patients who presented with pruritic red patches in the axillae, which on biopsy revealed severe compact parakeratosis, maintenance of the stratum granulosum and remarkable retention of keratohyaline granules throughout the stratum corneum. [1] A contact reaction to an antiperspirant/deodorant was suspected as the cause of the eruption. Since the first description of this condition several cases of axillary granular parakeratosis have been described by other authors [2],[3] and granular parakeratosis has also been described in other intertriginous sites. [4] Histological findings of granular parakeratosis have also been described in other lesions, namely keratotic papules, [5] acanthoma-like lesions [6] and even in association with dermatophyte infection, [7] dermatomyositis [8] and in molluscum contagiosum. [9]
We describe granular parakeratosis in a 27-year-old female who presented with pruritic keratotic papules on the left side of the face for one month and speculate that this papular rash is related to sweating and repeated frictional damage to the skin resulting in an unusual histological pattern, namely, granular parakeratosis.
Case Report
A 27-year-old female presented with pruritic keratotic papules over most of the left side of the face [Figure - 1] since one month. She felt that the lesions had appeared a few days after working in a warm environment. She had intense pruritus and admitted to repeatedly wiping this area with handkerchiefs and towels in an attempt to relieve this sensation. She had not used any cosmetics or deodorants but had used a strong topical corticosteroid (clobetasol propionate 0.05%) for three days with no change in the lesions. The lesions were small, discrete, firm, keratotic papules and geographic areas of erythematous macules involving a large area of the left cheek with intervening areas of normal skin. Most of the papules contained hyperpigmented keratotic plugs at their summits. A few papules were skin-colored while a few others showed superficial resolving scales.
The rest of the examination was unremarkable and on investigation, the hemogram showed slight leukocytosis (11,700/mm 3 ).
A skin biopsy was obtained from one of the papules and it revealed features typical of granular parakeratosis, namely compact hyperkeratosis with retention of kerato-hyaline granules within the horny layer accompanied by tiers of thin and flat parakeratotic nuclei. Apart from the epidermis similar changes were also seen to involve dilated follicular infundibula that contained plugs of granular parakeratosis [Figure - 2]. A sparse lymphocytic infiltrate was present in the upper dermis. No spongiosis or acrosyringeal or eccrine ductal involvement was seen. To relieve the severe pruritus, the patient was put on oral dexamethasone (2 mg/day) for three days, ebastine (10 mg/day) and instructed to apply calamine lotion on the lesions.
With oral steroids, pruritus was relieved within 48 h and at follow-up two weeks later the lesions had completely flattened leaving behind post-inflammatory hyperpigmentation [Figure - 3].
Discussion
Granular parakeratosis is a unique epidermal reaction pattern reflecting an acquired disorder of keratinization, which may occur as a contact reaction to an antiperspirant/deodorant and is often restricted to intertriginous areas. It is speculated that the offending agent alters the maturation sequence of the stratum granulosum and stratum corneum, possibly by interfering the process of degradation of filaggrin precursor to filaggrin units. [1] Studies on granular parakeratosis suggest a basic defect in the processing of profilaggrin to filaggrin which results in failure to degrade keratohyalin granules and to aggregate keratin filaments during cornification. Associated abnormalities of the cell surface structures and dysregulation of cornified envelope components may account for the retention hyperkeratosis. [10]
The occurrence of granular parakeratosis as a pathological finding is rare in biopsy specimens and it is possible that clinicians are not too familiar with this entity. [11] Our case is to the best of our knowledge the first case of granular parakeratosis reported from India and to occur on the face.
This patient did not present with the typical axillary lesions but had pruritic, keratotic papules on the face. The clinical history in our patient makes us suspect sweating and repeated friction as possible precipitating factors but this would need to be confirmed in a larger number of patients. Maceration of skin with repeated friction may be important causal factors in hot and humid climates and may lead to hyperkeratosis and keratinization with retention of keratohyaline granules within the corneocytes of the stratum corneum.
Granular parakeratosis is not a disease per se, but is an epidermal reaction pattern to various stimuli. Two forms of granular parakeratosis need to be distinguished: a) the dermatosis, granular parakeratosis that occurs generally in intertriginous regions or as in our case on the face and is a clinico-pathological entity and b) incidental finding of granular parakeratosis as a histological finding in other diseases like dermatophyte infection, molluscum contagiosum, solitary acanthomas etc. Therefore a distinction needs to be made between the incidental finding of histological changes of granular parakeratosis associated with other conditions like dermatophyte infection, molluscum contagiosum etc. and the dermatosis referred to as axillary or intertriginous granular parakeratosis.
It is important for clinicians and pathologists to be aware of this entity that appears to be a reaction pattern of the epidermis to as yet undefined stimuli and may be associated with varied clinical presentations.
| 1. |
Northcutt AD, Nelson DM, Tschen JA. Axillary granular parakeratosis. J Am Acad Dermatol 1991;24:541-4.
[Google Scholar]
|
| 2. |
Mehregan DA, Vandersteen P, Sikorsky L, Mehregan DR. Axillary granular parakeratosis. J Am Acad Dermatol 1995;33:373-5.
[Google Scholar]
|
| 3. |
Webster CG, Resnik KS, Webster GF. Axillary granular parakeratosis: Response to isotretinoin. J Am Acad Dermatol 1997;37:789-90.
[Google Scholar]
|
| 4. |
Chang MW, Kaufmann JM, Orlow SJ, Cohen DE, Mobini N, Kamino H. Infantile granular parakeratosis: Recognition of two clinical patterns. J Am Acad Dermatol 2004:50:S93-6.
[Google Scholar]
|
| 5. |
Resnik RS, DiLeonardo M. Follicular granular parakeratosis. Am J Dermatopathol 2003;25:428-9.
[Google Scholar]
|
| 6. |
Resnik KS, Kantor GR, DiLeonardo M. Granular parakeratotic acanthoma. Am J Dermatopathol 2005;27:393-6.
[Google Scholar]
|
| 7. |
Resnik KS, Kantor GR, DiLeonardo M. Dermatophyte related granular parakeratosis. Am J Dermatopathol 2004;26:70-1.
[Google Scholar]
|
| 8. |
Pock L, Hercogovα J. Incidental granular parakeratosis associated with dermatomyositis. Am J Dermatopathol 2006;28:147-9.
[Google Scholar]
|
| 9. |
Pock L, ?ermαkovα A, Zipfelovα J, Hercogovα J. Incidental granular parakeratosis associated with molluscum contagiosum. Am J Dermatopathol 2005;27:255-7.
[Google Scholar]
|
| 10. |
Metze D, Rutten A. Granular parakeratosis a unique acquired disorder of keratinization. J Cutan Pathol 1999;26:339-52.
[Google Scholar]
|
| 11. |
Scheinfeld NS, Mones J. Granular parakeratosis: Pathological and clinical correlation of 18 cases of granular parakeratosis. J Am Acad Dermatol 2005;52:863-7.
[Google Scholar]
|
Fulltext Views
2,853
PDF downloads
910





