Translate this page into:
Granuloma annulare - Histology reconsidered
2 Department of Dermatology, St. John's Medical College & Hospital, Bangalore - 560 034, India
Correspondence Address:
Y K Inchara
Department of Pathology, St. John's Medical College, Bangalore - 560 034
India
| How to cite this article: Chaitra V, Inchara Y K, Rajalakshmi T, Antony M. Granuloma annulare - Histology reconsidered. Indian J Dermatol Venereol Leprol 2010;76:568-569 |
Sir,
Granuloma annulare (GA) is a common dermatologic condition of unknown etiology, affecting all ages. It shows considerable clinical and histologic overlap with other diseases. [1] Therefore, it is important to be aware of its varied histologic appearances.
We reviewed 21 skin biopsies signed out as GA between 2004 and 2008 at the pathology department of a tertiary care hospital. The lesions were categorized as follows: interstitial (7 cases; [Figure - 1]a, palisading (6), granulomatous (1) and mixed (7). [1],[2] The features particularly assessed included pattern of infiltrate, elastophagocytosis, type of infiltrate, vasculitis, karyorrhectic debris and dermal mucin, as ratified by alcian blue/periodic acid-Schiff (AB-PAS).
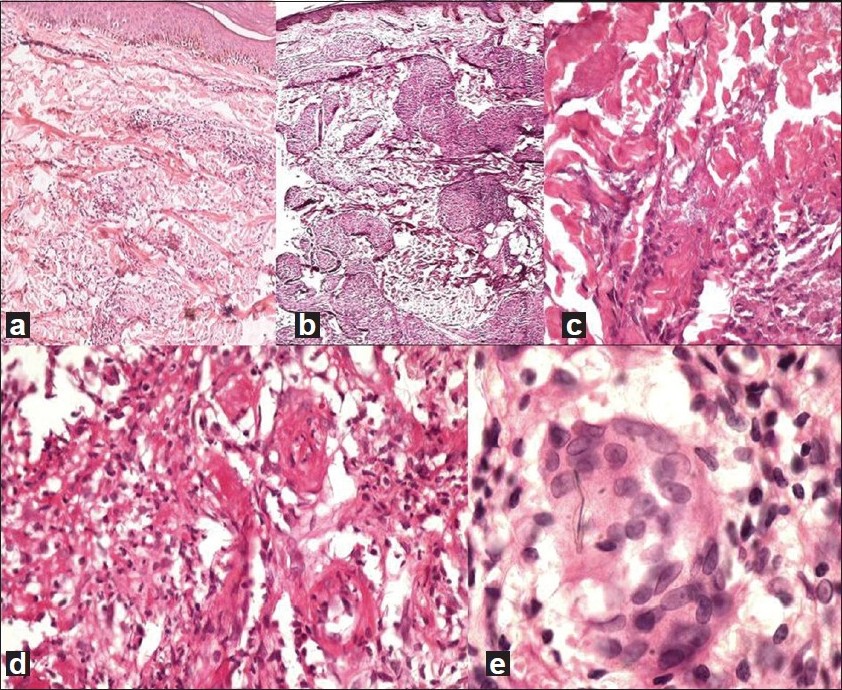 |
| Figure 1 : (a) Interstitial pattern in GA— histiocytes dissecting between collagen bundles and areas of normal dermis intervening (H and E, ×40). (b) Sarcoidal granulomas in GA (H and E, ×200). (c) Mucin identified without special stains: grey-blue, stringy material between collagen bundles (H and E, ×200). (d) Small-vessel vasculitis as evidenced by fibrinoid necrosis of vessel walls and surrounding neutrophils, nuclear debris (H and E, ×400). (e) Elastophagocytosis: multinucleate giant cells with engulfed elastic fibers (H and E, ×400) |
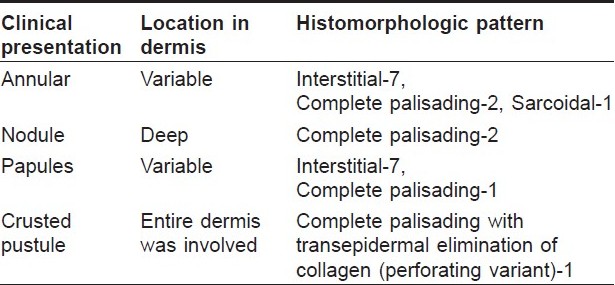
There were 11 men and 10 women, with a median age of 34 years. The lesions were localized in 10 cases and were generalized in 11 cases. Predilection for extremities was seen in 19 cases. Of these, one patient had painful lesions on the fingertips, and another showed involvement of palms and soles. Eleven cases presented as annular plaques. Papules were seen in 8 cases, nodules in 2 and crusted pustules in 1 case. One should recognize atypical presentations, such as pustules or painful acral lesions.
One case showed numerous discrete, tight epithelioid granulomas with absence of lymphocytes, mimicking sarcoidosis, but was distinguished by the presence of abundant mucin [Figure - 1]b. Stains for mycobacteria and fungi and workup for sarcoidosis were negative.
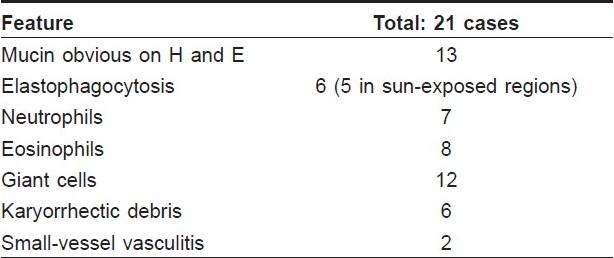
In most cases, the lesions were located in the upper and mid dermis (53%). The case presenting as pustules showed transepidermal elimination of collagen, conclusive of perforating GA. The other features assessed are summarized in [Table - 1]. The clinicopathologic correlation of the lesions is depicted in [Table - 2]. A single case was associated with polycythemia vera, supporting the claim of some authors that GA can be a paraneoplastic syndrome. [3] The histologic findings here were subtle, with altered collagen being present focally.
On follow-up, the lesions resolved in all except 1 case. This patient had perforating GA, with repeated recurrences.
Although GA is regarded as the prototype of a palisading granulomatous dermatosis, we found that the interstitial and mixed patterns predominate. Abundant dermal mucin is a hallmark of GA. Our study showed that a diligent search for mucin on H and E sections is rewarding, and mucin can be identified in 61% of cases without the aid of special stains [Figure - 1]c. Histiocytes are consistently present in GA. In some cases, they may not abound and there may be a preponderance of neutrophils and eosinophils, which should not preclude the diagnosis. A granulomatous pattern is infrequent, mimicking tuberculosis or sarcoidosis. In such situations, good clinicopathologic correlation with additional investigations is mandatory.
The etiology of GA is uncertain. It is possible that our observations reflect the etiopathogenesis in a few cases. The abundance of eosinophils seen in some (38%) of our biopsies may reflect an insect bite or a drug-related causation. Small-vessel vasculitis, as seen in 10% of our cases [Figure - 1]d, may have led to the formation of micro infarcts in the dermis, as a consequence of which the collagen was altered, evoking a histocytic response. This has been suggested previously in a study of 38 cases, where 33 (86%) biopsies showed vasculitis on histology/ immunofluorescence. [4] In this series, elastophagocytosis [Figure - 1]e was frequently observed in lesions over sun-exposed areas, adding credence to the idea that actinic granuloma is merely GA occurring in sun-exposed areas. [5]
The pathologist should be well versed with all the morphologic variations of GA in order to make a confident and reliable diagnosis.
| 1. |
Ackerman AB, Boer A, Bennin B, Gottlieb GJ. An algorithmic method for diagnosis that employs pattern analysis. In: Ackerman AB, editor. Histologic Diagnosis of Inflammatory Skin Diseases. 3 rd ed. New York: Ardor Scribendi; 2005. p. 375-408.
[Google Scholar]
|
| 2. |
Strutton G. The Granulomatous reaction pattern. In: Weedon D, editor. Skin Pathology. 2 nd ed. Edinburgh: Churchill Livingstone; 1999. p. 161-81.
[Google Scholar]
|
| 3. |
Cohen PR. Granuloma annulare associated with malignancy. South Med J 1997;90:1056-9.
[Google Scholar]
|
| 4. |
Dahl MV, Ullman S, Goltz RW. Vasculitis in granuloma annulare: Histopathology and direct immunofluorescence. Arch Dermatol 1977;113:463-7.
[Google Scholar]
|
| 5. |
Glusac EJ, Shapiro PE. Non-infectious Granulomas In: Elder DE, Elenitsas R, Johnson BL, Murphy GF, editors. Lever's Histopathology of skin. 9 th ed. Philadelphia: Lippincott Williams and Wilkins; 2005:373-4.
th ed. Philadelphia: Lippincott Williams and Wilkins; 2005:373-4.'>[Google Scholar]
|
Fulltext Views
5,638
PDF downloads
1,973





