Translate this page into:
Granulomatous cheilitis evolving into Melkersson-Rosenthal syndrome with bilateral facial palsy
Correspondence Address:
K Muhammed
Kunnummal House, Koroth School Road, Vatakara - 673 101, Kerala
India
| How to cite this article: Muhammed K, Nandakumar G, Thomas S. Granulomatous cheilitis evolving into Melkersson-Rosenthal syndrome with bilateral facial palsy. Indian J Dermatol Venereol Leprol 2004;70:313-314 |
 |
 |
 |
 |
 |
 |
Sir,
Melkersson-Rosenthal syndrome (MRS) is a rare disease characterized by the classical triad of recurrent swelling of the lips and/or face, fissured tongue (lingua plicata) and relapsing peripheral facial nerve paralysis.[1] However, many patients do not manifest all signs of the triad. Melkersson in 1928 first described labial edema in association with recurrent facial palsy. Rosenthal in 1930 emphasized the role of genetic factors and added scrotal tongue to the syndrome. Monosymptomatic or oligosymptomatic forms in which only one or any two features of the triad are present are common.
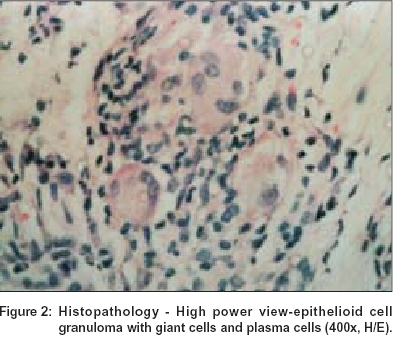
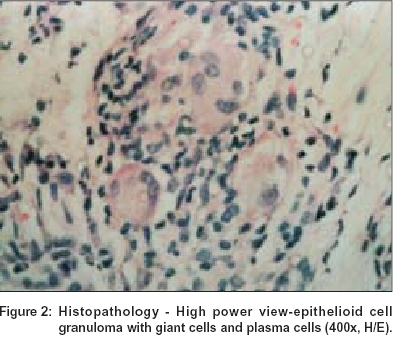
The most frequent monosymptomatic form is granulomatous cheilitis (GC),[2] described by Meischer in 1945, which is defined as painless chronic isolated enlargement of one or both lips due to granulomatous inflammation with a recurrent to gradually persistent course. Histopathologic examination reveals focal noncaseating epithelioid cell granulomas with lymphocytes and plasma cells. The lymph nodes may also show granulomatous inflammation. The origin of GC/MRS is obscure and the treatment is notoriously difficult. Among the numerous postulated theories are genetic factors, chronic infectious odontogenic foci, autoimmune mechanisms, allergic reactions and local disturbances of the autonomic nervous system.[1] Traditional therapies include systemic or intralesional steroids,[3] metronidazole,[4] clofazimine,[5] minocycline and surgical methods. Other treatment options include thalidomide, sulfasalazine, erythromycin, azathioprine and cyclosporine.
A 46-year-old female school teacher presented to the dermatology department of Medical College Hospital, Calicut with complaints of recurrent episodes of asymptomatic swelling of the upper lip of three years′ duration. The swelling used to subside with treatment, but there was no complete remission. She did not have any systemic complaints. On examination the patient had a diffuse swelling of her upper lip with a firm rubbery consistency [Figure - 1].
With a provisional diagnosis of granulomatous cheilitis, we investigated the patient. Her blood biochemistry, urinalysis and chest X-ray were normal. Biopsy from the lesion showed non-caseating epithelioid cell granulomas [Figure - 2]. The patient was started on oral metronidazole (400 mg) twice daily. Her lip swelling partially subsided with treatment.
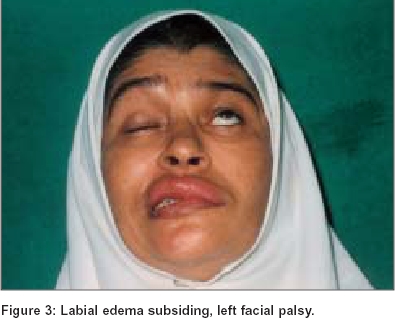
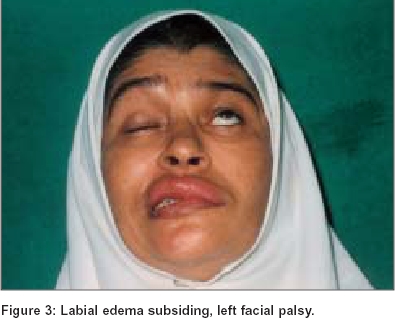
About six months later, she suddenly developed difficulty in closing her left eye and deviation of the angle of mouth to the right. On examination she was found to have left sided lower motor neuron (LMN) facial palsy [Figure - 3]. Her tongue appeared slightly larger than normal and showed superficial grooves on the anterior aspect. With these two new findings, the patient exhibited the complete triad of Melkersson-Rosenthal syndrome.
The facial palsy was managed with systemic steroids and physiotherapy. Oral clofazimine (100 mg) thrice daily along with intralesional triamcinolone acetonide (10 mg/ml) every three weeks were also started for the lip swelling. The facial palsy improved significantly and the lip swelling also subsided almost completely. Six months later, she again presented with relapse of right LMN facial palsy and was managed with systemic steroids and physiotherapy.
Clinically MRS may manifest as the classic triad, in an incomplete form, or with sequential appearance of the clinical findings. The onset of the disease is usually in middle age with no gender predominance. In a large series orofacial involvement was the predominant feature; it occurred in all 36 patients and was the presenting sign in 15 (42%).[2] The neurological features may precede the attacks of edema by months or years or may develop later and while initially intermittent, may occasionally become permanent.[1] Recurrent edema can be periorbital or vulval (vulvitis granulomatosa). In our patient, the labial edema responded partially to metronidazole and significantly to clofazimine and intralesional steroids,[3] but treatment did not prevent the occurrence of facial palsy. This case report highlights the interesting evolution of granulomatous cheilitis to full fledged MRS with bilateral facial palsy. The presence of the complete triad in a single patient is rare, being reported in only 10-20% of cases, and bilateral facial palsy in MRS is even rarer.[6]
| 1. |
Robert RM, Wolfgang W, Natalie Z, Kaddu S, Soyer HP, El Shahrawi CL, et al. Granulomatous cheilitis and Borrelia burgdorferi: Polymerase chain reaction and serologic studies in a retrospective case series of 12 patients. Arch Dermatol 2000;136:1502-6.
[Google Scholar]
|
| 2. |
Greene RM, Rogers RS 3rd. Melkersson-Rosenthal Syndrome: A review of 36 patients. J Am Acad Dermatol 1989;21:1263-70.
[Google Scholar]
|
| 3. |
Perez-Calderon R, Gonzalo-Garijo MA, Chaves A, de Argila D. Chelitis granulomatosa of Melkersson-Rosenthal syndrome: Treatment with intralesional corticosteroid injections. Allerg Immunopathol 2004;32:36-8.
[Google Scholar]
|
| 4. |
Kano Y, Shiohara T, Yagita A. Treatment of recalcitrant cheilitis granulomatosis with metronidazole. J Am Acad Dermatol 1992;27:629-30.
[Google Scholar]
|
| 5. |
Arbiser JL, Moschella SL. Clofazimine: A review of its medical uses and mechanisms of action. J Am Acad Dermatol 1995;32:241-7.
[Google Scholar]
|
| 6. |
Lopez Gonzalez R, Bragado Alonso A, Delgado Vicente S, Rodriguez Prieto MA. Melkersson-Rosenthal syndrome, about one case with bilateral facial paralysis. An Med Interna 2004;21:255-6.
[Google Scholar]
|
Fulltext Views
3,998
PDF downloads
959





