Translate this page into:
Granulomatous inflammation with chronic folliculitis as a complication of bee sting acupuncture
Correspondence Address:
Won-Soo Lee
Department of Dermatology and Institute of Hair and Cosmetic Medicine, Yonsei University, Wonju College of Medicine, Wonju-220 701
Korea
| How to cite this article: Lee NR, Lee SY, Lee WS. Granulomatous inflammation with chronic folliculitis as a complication of bee sting acupuncture. Indian J Dermatol Venereol Leprol 2013;79:554 |
Sir,
Bee sting therapy is one of the traditional herbal medical procedures that has been widely used for the treatment of chronic recalcitrant neuralgia and arthralgia in Asian and Middle Eastern countries, and is also called apitherapy. [1],[2] There are two methods of this therapy, one is stinging directly to the treatment site [Figure - 1] and the other is injecting the artificially extracted venom from a bee. [3] The substrates that compose the venom of a bee have anti-inflammatory and analgesic effect. [4] The bee leaves poison sac and neural plexus when stinging, and the retained sting materials at the treatment site may induce inflammation and granulomatous reaction. [2]
 |
| Figure 1: Bee sting acupuncture therapy performing. The bee is used to sting directly to the lesions |
A 50-year-old man visited our clinic complaining of erythematous papules and nodules with tingling sensation on his back [Figure - 2] which showed wax and wane for the past 3 months, despite he had been treated with intralesional injection of steroid in a private clinic. He had no specific history but received bee sting acupuncture for several years in an oriental medical clinic due to his back pain. The skin lesions occurred after 2-3 years from the apitherapy procedures, directly at the sites that received the acupuncture. Histopathologic findings of biopsy specimen taken from the back showed perifollicular dense inflammatory infiltration composed of lymphocytes, plasma cells, and histiocytes [Figure - 3]a and b. Around the perifollicular infiltration, ruptured granulomatous reaction composed of epitheloid cells and lymphocytes was shown [Figure - 3]c. There was no giant cell or foreign body in the whole specimen. Special stains, Gomori methenamine silver (GMS) and diastase-periodic acid-Schiff (d-PAS) revealed negative findings. The patient was diagnosed as chronic folliculitis and granuloma caused by bee sting acupuncture treatment. For anti-inflammatory effect, he was treated with oral and topical antibiotics for a short period. The lesions showed slight improvement but the patient was not able to be followed-up.
 |
| Figure 2: Various sized, erythematous papules and nodules on the back, in the sites that received bee sting acupuncture |
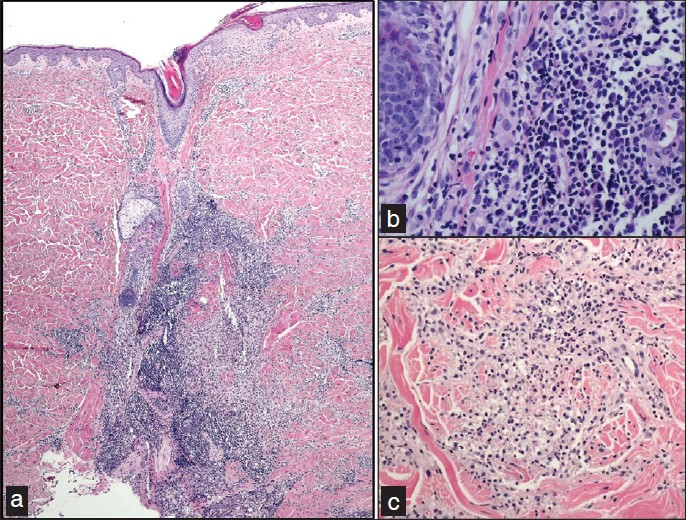 |
| Figure 3: Histologic features of biopsy taken from the back. (a) Dense inflammatory infiltration in the perifollicular area. (b) The perifollicular infiltration is composed of lymphocytes, plasma cells, and histiocytes. (c) Granulomatous reaction composed of lymphocytes and epitheloid cells. Hematoxylin and eosin; original magnification: (a) H and E, ×40; (b) H and E, ×400; (c) H and E, ×200 |
Reactions to insect bites including bee sting clinically show mild symptoms such as erythema, edema, urticaria and pain. There are also few serious events, that is, anaphylaxis and respiratory failure. Most insects retrieve their stingers after stinging, but bees leave poison sac and neural plexus at the site of injection and these retained materials in the skin continuously act as antigens, induce activation of macrophages and finally, derive granulomatous inflammatory reaction. Several dermatological complications of bee sting therapy have been reported; anaphylaxis, contact urticaria, [3] Mycobacterium chelonae infection, foreign body granuloma, [2] delayed type skin reaction, [4] skin atrophy, and pyoderma. Systemic complications that may be fatal such as disseminated intravascular coagulation (DIC), [5] hepatotoxicity, kidney injury, and thalamic hemorrhage have also been reported.
Folliculitis is an inflammation in the perifollicular area that presents as erythematous papules and pustules on the trunk, neck and groin area. The causes of folliculitis are mostly infection, bacterial organisms, fungi such as Pityrosporum, viruses, and demodex. Histopathologic findings of chronic folliculitis differs from acute folliculitis, that it shows perifollicular infiltration composed of lymphoid cells, histiocytes and plasma cells rather than neutrophils.
Granulomatous inflammation is a distinctive inflammatory pattern characterized by granulomas, containing epitheloid histiocytes. Of the five histological types of granuloma, foreign body granulomatous reaction is divided into two subtypes, allergic and non-allergic. Foreign body type giant cells and foreign body surrounded by numerous histiocytes and lymphocytes are characteristically visualized in the non-allergic type. Besides, granuloma composed of histiocytes is seen in the allergic type, and phagocytosis of foreign body is not seen. [2] The granuloma of this patient is suggested to be an allergic type foreign body granulomatous reaction due to remained poison sac or neural plexus in the skin, not due to the stinger which should have been discovered in the serial section of the specimen.
Although several reports had been published in Korean literatures, there are only five reports of complications of bee sting acupuncture in English literatures, since apitherapy is usually performed in Asian and Middle Eastern countries. Only one case of the five English literatures is a dermatologic complication. Therefore, we report the first case of chronic folliculitis associated with granuloma as a complication of bee sting acupuncture therapy, and no reports of chronic folliculitis combined with granulomatous reaction as in our case have been reported.
| 1. |
Lee MS, Pittler MH, Shin BC, Kong JC, Ernst E. Bee venom acupuncture for musculoskeletal pain: a review. J Pain 2008;9:289-97.
[Google Scholar]
|
| 2. |
Bae EJ, Son SB, Seo SH, Son SW, Kim IH. A case of foreign body granuloma with skin necrosis occurring after bee sting therapy. Korean J Dermatol 2009;47:350-3.
[Google Scholar]
|
| 3. |
Yoo MS AS, Lee SH, Lee WS. Contact urticaria due to bee sting therapy in a patient with chronic pain. Kor J Dermatol 1994;32:895-8.
[Google Scholar]
|
| 4. |
Kim DH, Kim MY, Park YM, Kim HO. A case of delayed type skin reaction induced by bee venom acupuncture. Kor J Dermatol 2005;43:1237-40.
[Google Scholar]
|
| 5. |
Jung JW, Jeon EJ, Kim JW, Choi JC, Shin JW, Kim JY, et al. A fatal case of intravascular coagulation after bee sting acupuncture. Allergy Asthma Immunol Res 2012;4:107-9.
[Google Scholar]
|
Fulltext Views
4,353
PDF downloads
1,843





