Translate this page into:
Granulomatous mycosis fungoides with hypohidrosis mimicking lepromatous leprosy
Correspondence Address:
Uday Khopkar
Department of Dermatology, Seth GS Medical College and KEM Hospital, Parel, Mumbai-12
India
| How to cite this article: Gutte R, Kharkar V, Mahajan S, Chikhalkar S, Khopkar U. Granulomatous mycosis fungoides with hypohidrosis mimicking lepromatous leprosy. Indian J Dermatol Venereol Leprol 2010;76:686-690 |
Abstract
Granulomatous mycosis fungoides (GMF) is a rare type of cutaneous T cell lymphoma. A 38-year-old married male presented with decreased sweating all over the body for last 8 years, progressive redness and scaling over body for 2 years and multiple noduloulcerative lesions over the body for 1 year. Cutaneous examination revealed generalized erythema and scaling with poikilodermatous changes over chest and upper back along with multiple noduloulcerative lesions. Skin biopsy from a nodular lesion revealed dense granulomatous infiltrate of atypical lymphocytes with epidermotropism and sparing of appendages. Diagnosis of GMF was made. Computed tomographic scan of thorax, abdomen and pelvis revealed axillary and inguinal lymphadenopathy. Immunohistochemistry revealed leukocyte common antigen and CD3 positivity suggestive of T cell origin. Patient was started on CHOP (Cyclophosphamide, Hydroxydaunorubicin, Oncovin and Prednisolone) regimen of chemotherapy with marked improvement after three cycles of chemotherapy. This case had some clinical resemblance to lepromatous leprosy.Introduction
Granulomatous mycosis fungoides (GMF) is a rare type of cutaneous T cell lymphoma (CTCL). The first case of this entity described in 1970 had multiple ulcerated nodules, many of which healed spontaneously with atrophic scars and poikiloderma. Heterogenous nature of clinical presentation delays diagnosis and consequently diagnosis is based mainly on histopathological features, immunohistochemistry and gene rearrangement studies. [1],[2] We report this case for its rarity, association with hypohidrosis, granulomatous lymphadenitis and to highlight its resemblance to lepromatous leprosy.
Case Report
A 38-year-old married male hailing from Uttar Pradesh presented with decreased sweating all over the body for last 8 years, generalized redness and scaling over the body for 2 years and multiple painful ulcerated lesions over the body for 1 year. He was apparently alright 25 years back (1984) when he developed asymptomatic hypopigmented patches over right thigh and face. Gradually he developed multiple patches all over the body over a period 10 years. The patient had taken multiple ayurvedic and homeopathic treatments in past without any improvement but no anti-leprosy treatment was received.
Later, the lesions started becoming dry and confluent with dyspigmentation since last 2 years and at the same time he developed multiple painless swellings over neck, axillae and groins for which he was treated with antituberculous therapy empirically without improvement. Since the last 1 year he started getting multiple painful noduloulcerative lesions over the body at multiple sites. He was investigated for leprosy and CTCL. Skin biopsy was suggestive of CTCL and he was referred to an oncologist for further management. Lymph node biopsy showed diffuse infiltrate of atypical lymphocytes with histiocyte microgranulomas. Bone marrow aspiration and biopsy showed normal uninvolved bone marrow. Hemogram revealed marginally raised erythrocyte sedimentation rate (36 mm at the end of 1 hour) and white blood cell count (10,800 cells/mm 3 ). Rest of the investigations including liver and kidney function tests were within normal limits. His serology was negative for HIV 1 and 2 as well as HBsAg and hepatitis C virus. Computed tomographic scan of the thorax, abdomen and pelvis revealed bilateral axillary and inguinal lymphadenopathy. Diagnosis of mycosis fungoides (MF) nodular stage with lymph node involvement was made. He was referred to us by the oncopathologist to rule out leprosy in view of history of hypopigmented patches, hypohidrosis and granulomatous infiltrate in histopathology.
On presentation to us, he had diffuse erythema and induration. The face was shiny and infiltrated with loss of eyebrows, accentuated skin markings with infiltration of both ears [Figure - 1]. He also had poikilodermatous changes all over the body along with multiple painful indurated nodules of various sizes ranging from 2 to 6 cm. Many of these were ulcerated [Figure - 2]. But there were no hypopigmented patches. There was bilateral axillary and inguinal lymphadenopathy. The lymph nodes were firm, non-tender, mobile and non-matted measuring 2-3 cm in largest diameter. There was no sensory deficit, and peripheral nerve examination was also normal. Rest of the general and systemic examination was within normal limits.
 |
| Figure 1 :Diffuse infiltration of face with loss of eyebrows, accentuation of skin markings and multiple noduloulcerative lesions |
 |
| Figure 2 :Ulcerated nodule topped with hemorrhagic and purulent crust over chest |
We did a repeat skin biopsy from a nodular lesion on forearm. Histopathology revealed dense infiltrate of lymphocytes within the dermis extending deep up to subcutaneous fat [Figure - 3]. The lymphocytes were of large size with hyperchromatic indented nuclei. There was marked epidermotropism without spongiosis and some lymphocytes were aligned singly at the basal layer of the epidermis with characteristic basal tagging of lymphocytes. Multiple tuberculoid granulomas with Langhans and foreign body type of giant cells were also seen [Figure - 4]. Special stains for mycobacteria and fungi revealed no organisms. Infiltrate spared the nerves and appendages. The number of sweat units appeared normal but there was granulomatous infiltrate around them. Slit skin smear was negative for Mycobacterium leprae. Peripheral smear examination revealed no definite atypical lymphocytes. Immunohistochemistry of skin biopsy was positive for leukocyte common antigen and CD3 [Figure - 5] suggesting T cell origin of lymphoma. Tumor cells were negative for CD15, CD20, CD23, CD30 and anaplastic lymphoma kinase-1. Polymerase chain reaction (PCR) for monoclonality of the malignant cells is more confirmatory but we could not do it due to unaffordability of patient. PCR for M. leprae was also not done due to unavailability and as Fite-Faraco stain was also negative. Thus, we confirmed the diagnosis of GMF stage IV A2 of EORTC staging of MF. The patient was started on CHOP (Cyclophosphamide, Hydroxydaunorubicin, Oncovin and Prednisolone) regimen of chemotherapy by the oncologist with good improvement in skin lesions after three cycles [Figure - 6]. However, erythema and scaling were persistent and no noticeable improvement in hypohidrosis was seen. The patient is following up with the oncologist.
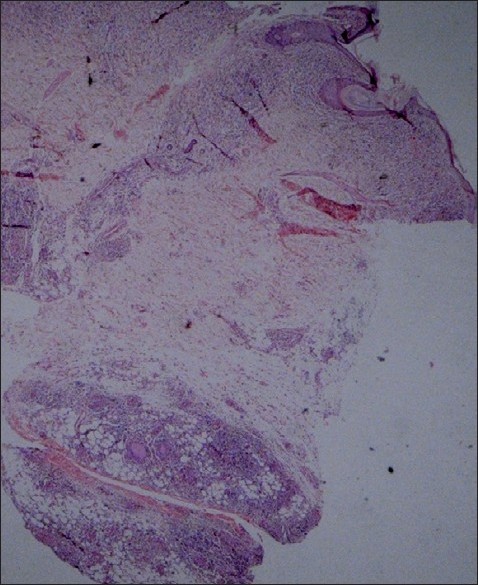 |
| Figure 3 :Low power view showing dense lymphocytic infiltrate in the dermis and subcutaneous tissue (H and E, ×40) |
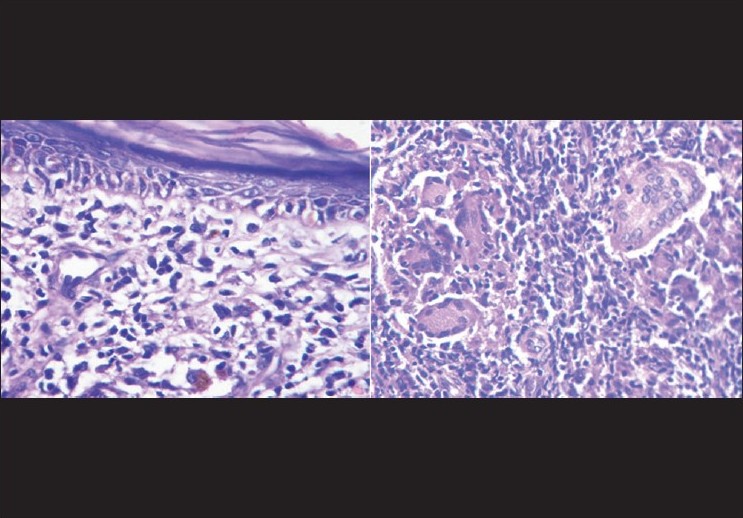 |
| Figure 4 :Dense dermal infiltrate of atypical lymphocytes with epidermotropism without spongiosis and characteristic basal epidermal tagging of lymphocytes and tuberculoid granuloma in the deep dermis with foreign body type of giant cells (H and E, ×200) |
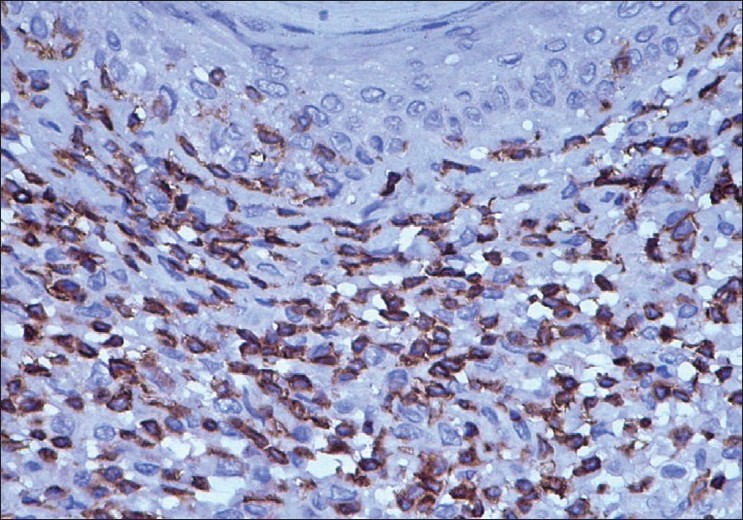 |
| Figure 5 :Immunohistochemistry showing CD3 positive lymphocytic infiltrate in dermis (×200) |
 |
| Figure 6 :Lesion on chest healing with puckered scar after three cycles of chemotherapy (compare with Figure 2) |
Discussion
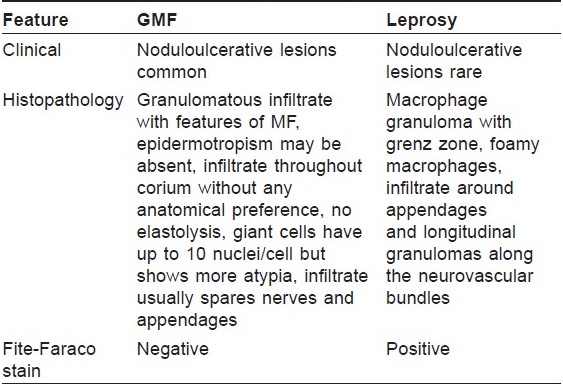
Granuloma formation in MF is now a well-characterized feature. GMF was first reported in 1970. [2] Because of variable presentation, GMF lacks particular clinical criteria for diagnosis, making it primarily a histopathological diagnosis and it should be suspected in cases of granulomatous dermatitis with other features of MF. [3] It can be confused especially with granulomatous slack skin or leprosy and should be differentiated on histopathology.
Granuloma formation is known to occur in various lymphomas and other malignancies including solid organ malignancies and even malignant melanoma with variable frequency. [1] Hodgkin′s disease has the highest frequency of granuloma formation among the various lymphomas. It is rarely seen in non-Hodgkin′s lymphomas including cutaneous lymphomas. [4] In cutaneous lymphomas, two variants, granulomatous slack skin and GMF are especially associated with granuloma formation. Though the granuloma is usually sarcoidal, tuberculoid and granuloma annulare like granulomas are also described in GMF. [2] Both GMF and granulomatous slack skin can be mistaken for some non-neoplastic granulomatous dermatitis on histology but epidermotropism with atypical lymphocytes helps to differentiate between the two. [5] Concomitant occurrence of non-neoplastic granulomas with MF like sarcoidosis and granuloma annulare or infectious granulomas may also be considered. [1],[6],[7] GMF may also be mistaken for leprosy specially in countries like India where leprosy is endemic. This leads to delay in diagnosis and treatment. A case of granulomatous slack skin mistaken for leprosy and treated with dapsone and rifampicin has been described. [8] Diagnostic dilemma with leprosy is more likely if a patient has peripheral neuropathy due to GMF itself. [9] Presence of epidermotropism and atypical lymphoid infiltrate throughout the dermis without any anatomical preference with sparing of appendages and dermal nerves allows differentiation between the two on histopathology. These findings were present in our case. The clinical similarities between GMF and leprosy and difficulty in differentiation of the two on histopathology led us to compare them [Table - 1].
Granulomatous lymphadenitis is rare in GMF. A case of GMF with granulomas in lymph node initially diagnosed as sarcoidosis is reported. [7] In our case, clinical and histological involvement of lymph nodes with formation of multiple histiocytic microgranulomas was observed. There was no CNS, pulmonary, thyroid or intestinal involvement. In view of history of disease starting as hypopigmented patches initially, GMF in our case presumably evolved from preexisting hypopigmented MF.
To the best of our knowledge, presence of hypohidrosis with GMF is not reported. The hypohidrosis in our case could be due to inflammatory and compressive effect of the dense granulomatous infiltrate onto sweat units.
The exact etiology of granulomatous reactions associated with malignancies in not known. Some consider it as peculiar hypersensitivity response to malignant cells or some persistent infection while some consider it as protective phenomenon with good prognosis. [10],[11],[12] Prognostic significance of granulomas in the setting of malignant disease is not clear though some may consider it as protective response of host. Granuloma does not necessarily mean better prognosis as four patients of GMF who died of disseminated disease have been reported. [4],[11] A case with spontaneous regression of GMF in HIV positive patient has also been described. Regression was thought to be probably due to cytotoxic effect of HIV on neoplastic cells. [13]
In conclusion, our case had many unusual features, viz., presence of hypohidrosis, granulomatous lymph node involvement. GMF presumably evolved from hypopigmented MF. It had clinical resemblance to leprosy due to diffuse infiltration of face, loss of eyebrows and history of hypopigmented patches.
| 1. |
Fischer M, Wolharb J, Audring H, Sterry W, Marsch WC. Granulomatous mycosis fungoides. Report of two cases and review of the literature. J Eur Acad Dermatol Venereol 2000;14:196-202.
[Google Scholar]
|
| 2. |
von Nida J, Randell P, Heenan P. Granulomatous mycosis fungoides with extensive chest wall involvement. Australas J Dematol 2004;45:42-6.
[Google Scholar]
|
| 3. |
Panda S. Mycosis fungoides: Current trends in diagnosis and management. Indian J Dermatol 2007;52:5-20.
[Google Scholar]
|
| 4. |
Dabski K, Stoll HL. Granulomatous reactions in mycosis fungoides. J Surg Oncol 1987;34:217-29 .
[Google Scholar]
|
| 5. |
LeBoit PE, Zackheim HS, White CR. Granulomatous variant of cutaneous T-cell lymphoma. Am J Surg Pathol 1988;12:83-5.
[Google Scholar]
|
| 6. |
Wong WR, Yang LJ, Kuo TT, Chan HL. Generalized granuloma annulare associated with granulomatous mycosis fungoides. Dermatology 2000;200:54-66.
[Google Scholar]
|
| 7. |
Mainguence C, Picard O, Audoudin J, Le Tourneau A, Jagueux M, Diebold J. An unusual case of mycosis fungoides presenting as sarcoidosis or granulomatous mycosis fungoides. Am J Clin Pathol 1993;92:82-6.
[Google Scholar]
|
| 8. |
Helm KF, Cerio R, Winkelmann RK. Granulomatous slack skin: a clinicopathological and immunohistochemical study of three cases. Br J Dermatol 1992;126:142-7.
[Google Scholar]
|
| 9. |
Lili-Naz H, Vera B, Sukriti N. Muscle and nerve involvement in granulomatous mycosis fungoides. Muscle and Nerve 2007;36:860-5.
[Google Scholar]
|
| 10. |
Cerroni L. Cutaneous granulomas and malignant lymphomas. Dermatology 2003;206:78-80.
[Google Scholar]
|
| 11. |
Rangioletti F, Cerroni L, Massone C, Basso M, Ciambellotti A, Rebora A. Different Histologic patterns of granulomas in systemic lymphomas. J Am Acad Dermatol 2004;51:600-06.
[Google Scholar]
|
| 12. |
Flaxman BA, Koumans JAD, Ackerman AB. Granulomatous mycosis fungoides: a 14-year follow up of a case. Am J Dermatopathol 1983;5:145-51.
[Google Scholar]
|
| 13. |
Sorrells T, Pratt L, Newton J, Graham S, Ryan M. Spontaneous regression of granulomatous mycosis fungoides in an HIV positive patient. J Am Acad Dermatol 1997;37:876-80.
[Google Scholar]
|
Fulltext Views
3,605
PDF downloads
2,132





