Translate this page into:
Granulomatous slack skin syndrome: Report of a unique case
Correspondence Address:
A Ramesh
Department of Dermatology, Madras Medical College and Rajiv Gandhi Government General Hospital, Chennai - 600 003, Tamil Nadu
India
| How to cite this article: Maheswari S U, Sampath V, Ramesh A. Granulomatous slack skin syndrome: Report of a unique case. Indian J Dermatol Venereol Leprol 2018;84:169-173 |
Abstract
Granulomatous slack skin syndrome is a rare variant of cutaneous T-cell lymphoma (mycosis fungoides). It is characterized clinically by redundant skin folds, which show a predilection towards flexural areas such as the axilla and the groin. Histologically, it shows a granulomatous T-cell infiltrate and loss of elastic tissue. It has an indolent but progressive course; and is usually refractory to treatment. We report a unique case of slack skin syndrome, sparing the classical sites with rapid and unusual involvement of non-intertriginous areas.Introduction
Primary cutaneous lymphomas very rarely display granulomatous features (2%) and these include granulomatous slack skin syndrome and granulomatous mycosis fungoides. Granulomatous slack skin syndrome is a rare variant of cutaneous T-cell lymphoma, with approximately fifty cases reported in literature so far.[1],[2] It is characterized by the gradual development of erythematous plaques and redundant skin folds in intertriginous and flexural areas.[1] We report a unique case of granulomatous slack skin syndrome, sparing the classical sites with a rapid and unusual involvement of non-intertriginous areas.
Case Report
A 60-year-old woman presented with a 1-year history of multiple pigmented asymptomatic lesions involving the lower part of the trunk and bilateral lower limbs. Over a period of 5 months, the lesions progressively increased in size and some lesions showed laxity of the overlying skin. On examination, sharply demarcated pigmented plaques with fine scales were seen predominantly on the left lower abdomen, buttock, thigh, shin, ankle and a part of the right leg [Figure - 1].
 |
| Figure 1: Well-defined, hyperpigmented, indurated plaques |
The intertriginous areas such as axilla and groin were normal. The lax skin on the left thigh and right leg appeared like atrophic poikilodermatous plaques [Figure - 2]a and [Figure - 2]b. The basic investigations were within normal limits; except for a mild increase in serum calcium levels. Serum protein immunotyping showed absence of monoclonal gammopathy. Immunofluorescence was negative for autoantibodies. Computerized tomography of the chest, abdomen and pelvis showed shotty pulmonary, mesenteric and retroperitoneal lymph nodes; however fine needle aspiration cytology/biopsy could not done as the patient did not give her consent.
 |
| Figure 2a: Skin laxity in the right leg |
 |
| Figure 2b: Skin laxity in the left thigh region |
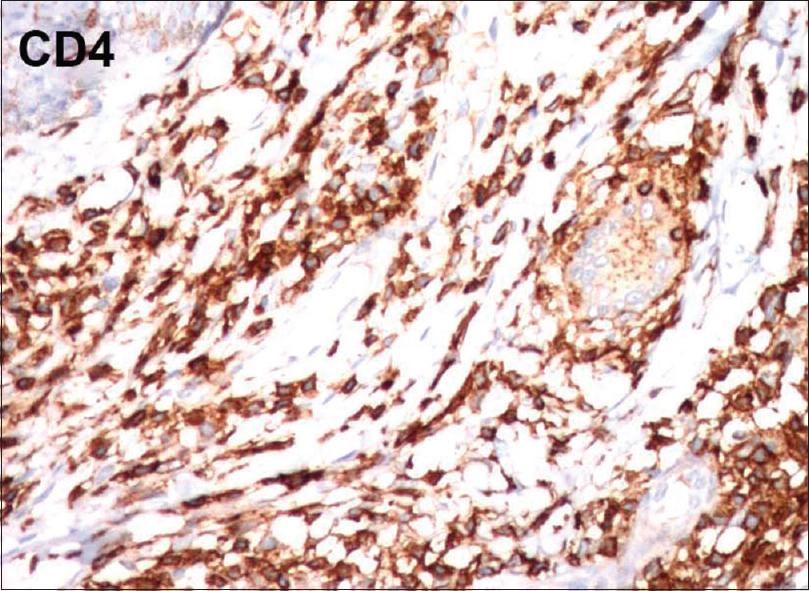
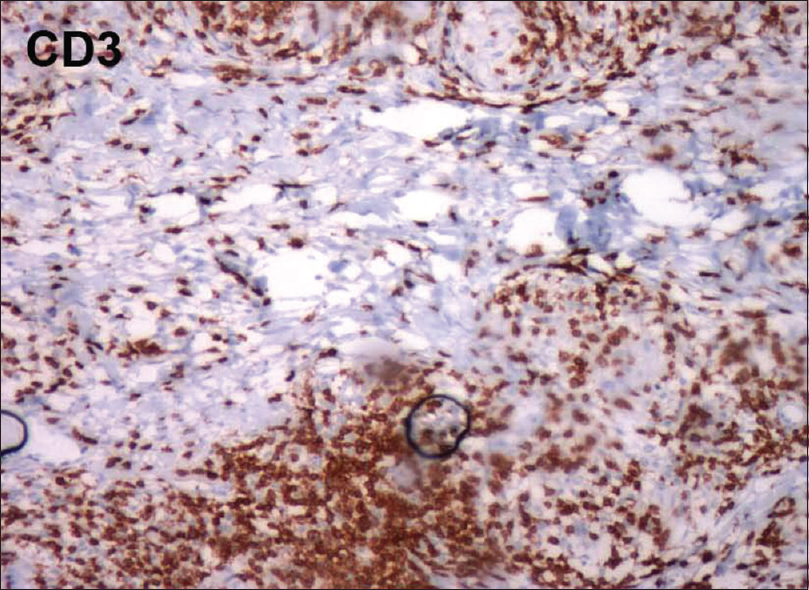
Skin biopsy from the affected sites revealed diffuse granulomatous infiltrates composed of lymphocytes and histiocytes and giant cells [Figure - 3]a. Lymphocytes showed atypical changes with single-cell epidermotropism [Figure - 3]b. The infiltrates were seen throughout the entire dermis and extending up to the subcutis [Figure - 4]a and [Figure - 4]b. Numerous multinucleated giant cells (more than 40 nuclei) scattered throughout the dermis, showed evidence of emperipolesis and elastophagocytosis [Figure - 5]a. Elastica van Gieson staining revealed reduced or absent elastic tissue in dermis [Figure - 5]b. Immunohistochemistry showed CD3 and CD4 positivity and reduced CD7 and CD8 expression [Figure - 6]a,[Figure - 6]b,[Figure - 6]c,[Figure - 6]d. Based on the above clinicopathological findings, we made a diagnosis of granulomatous slack skin syndrome, which is a variant of mycosis fungoides. The patient was started on psoralen and ultraviolet A therapy. Since the clinical response was not satisfactory, the patient was referred to oncology department for further management and follow-up.
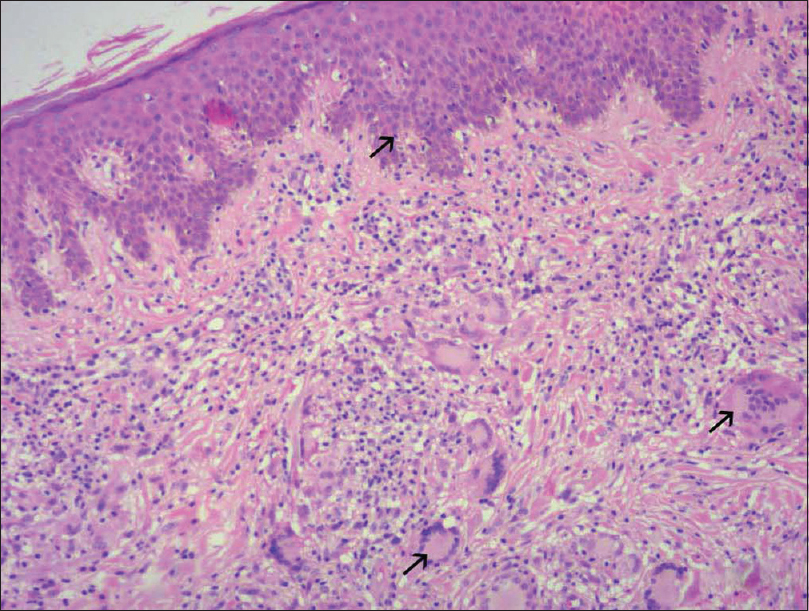 |
| Figure 3a: Diffuse granulomatous dermal infiltrates composed of atypical lymphocytes, histiocytes and giant cells (H and E, ×200) |
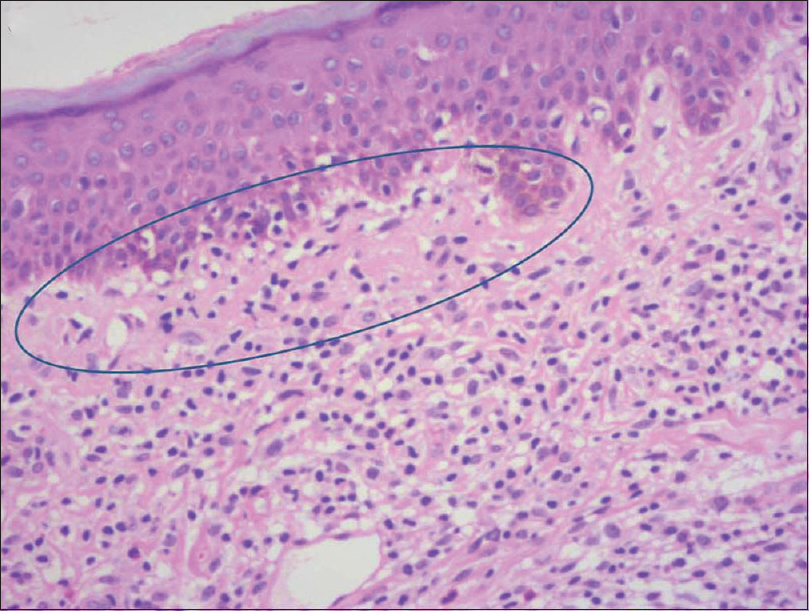 |
| Figure 3b: Focal epidermotropism of atypical lymphocytes (H and E, ×200) |
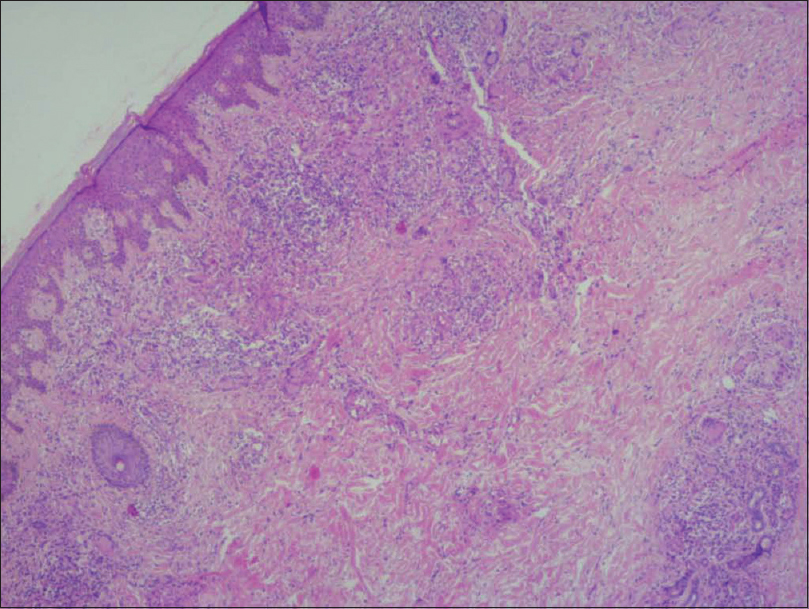 |
| Figure 4a: Deep dermal granulomas (H and E, ×100) |
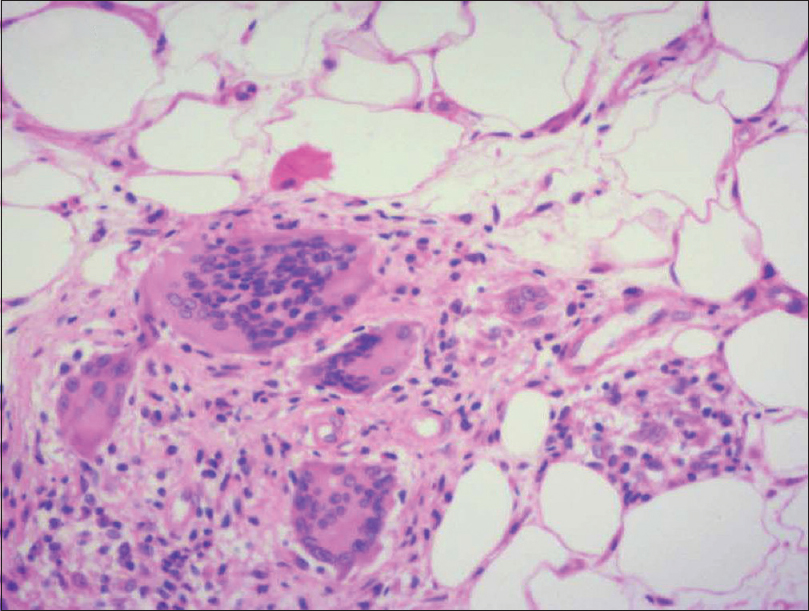 |
| Figure 4b: Infiltrates extending up to subcutis (H and E, ×400) |
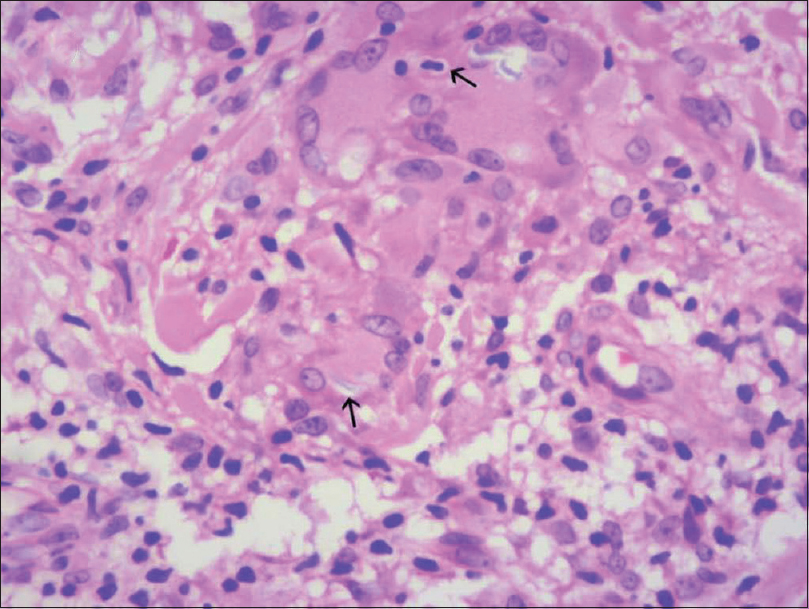 |
| Figure 5a: Multinucleated giant cells showing emperipolesis and elastophagocytosis (arrows) (H and E, ×400) |
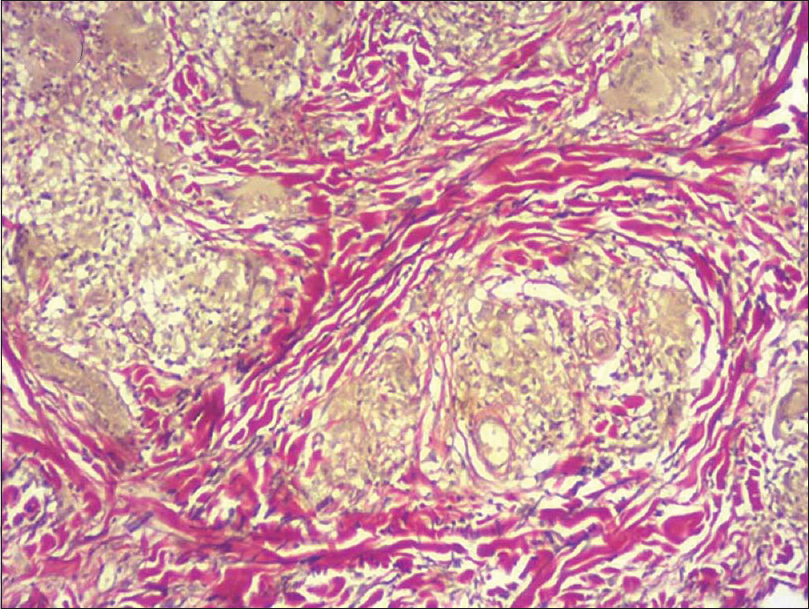 |
| Figure 5b: van Gieson staining showing reduction in elastic fibers (×100) |
 |
| Figure 6a: Immunohistochemistry showing CD3 positivity (×100) |
 |
| Figure 6b: Immunohistochemistry showing CD4 positivity (×100) |
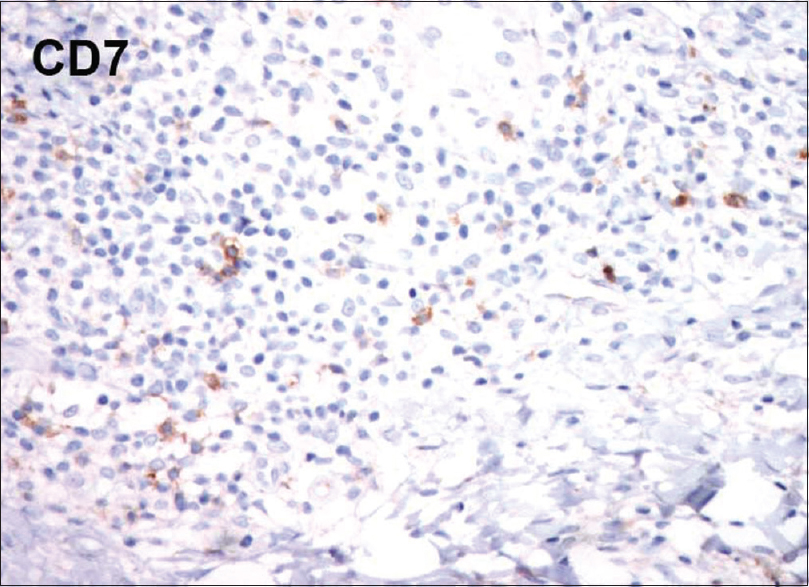 |
| Figure 6c: Immunohistochemistry showing reduced staining for CD7 (×100) |
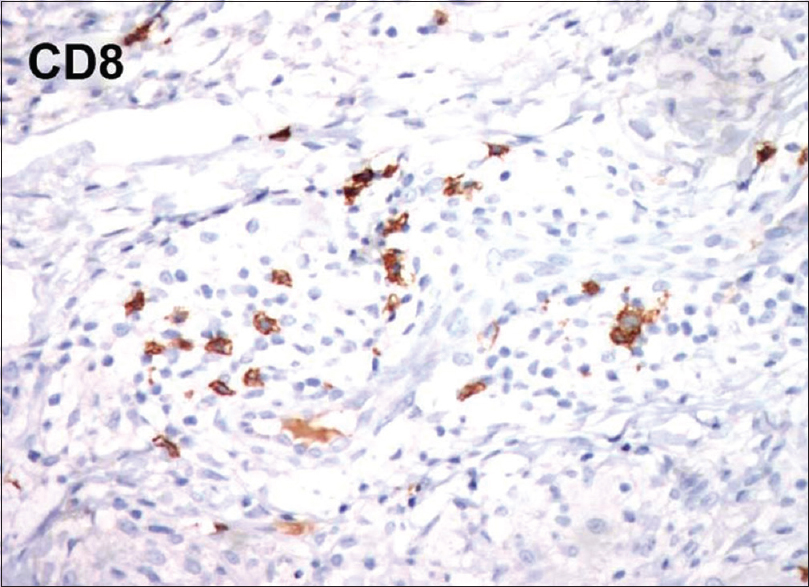 |
| Figure 6d: Immunohistochemistry showing reduced staining for CD8 (×100) |
Discussion
The term “granulomatous slack skin syndrome” was coined by Ackerman in 1978.[3] It is an extremely rare subtype of cutaneous T-cell lymphoma with a slight male preponderance.[4] The common clinical presentation includes the appearance of sharply demarcated painless, poikilodermatous, indurated plaques and patches, predominantly involving the axilla and the inguinal regions; but can be quite variable at initial presentation. The size increases slowly and progressively within a few years, leading to redundant folds of loose skin, whereas lesions in nonintertriginous regions tend not to undergo this transformation.[5] Our case, in contrast to the above findings, involved the nonintertriginous areas and lacked the typical feature of redundant skin folds. The development of skin lesions in our case was very rapid in contrast to the observations made by van Haselen et al.[6] and Kempf et al.[1] where the disease had an indolent slow and progressive course. The extracutaneous manifestations of the disease can rarely involve organs such as spleen, lymph node and lung.[7]
This condition is histologically characterized by the presence of diffuse granulomatous infiltrates composed of lymphocytes and histiocytes, throughout the entire dermis and sometimes the subcutaneous tissues as well. The granulomas are noncaseating in nature. The lymphocytes show pleomorphic, hyperchromatic and irregular nuclei. In the dermis, numerous multinucleated giant cells phagocytosing lymphoid cells (emperipolesis) and elastic fibers (elastophagocytosis) are seen. The giant cells have nuclei arranged either as Langhans type cell or of foreign body type. The reduced or absent elastic tissue is demonstrated in van Gieson staining. In immunohistochemistry, lymphocytes typically stain positive for CD3 and CD4 along with a negative or reduced staining for CD7 and CD8.[7] All the above findings were documented in our case.
The exact etiology of this condition is presently unknown. A chromosomal translocation involving t(3;9) (q12; p24) has been described. The rearrangement of T-beta cell receptor gene is seen in molecular analysis. In approximately 50% of the patients, an association with Hodgkin's disease, non-Hodgkin's lymphoma or mycosis fungoides is observed.[6]
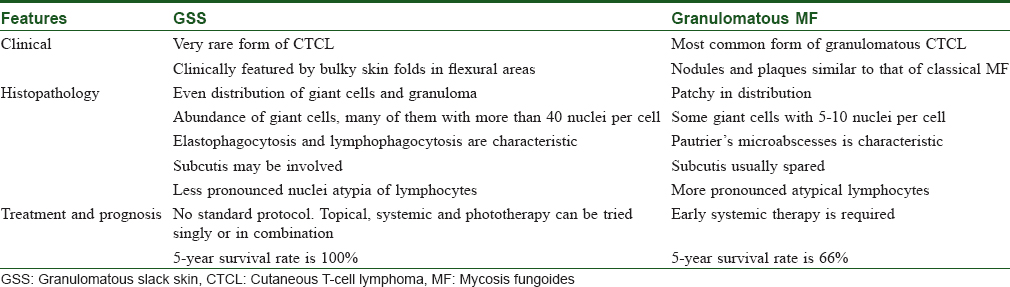
Hermes et al. hypothesized that the granuloma formation in this condition may be the result of antigenic status of the atypical lymphocytes and/or elastic fibers.[8] Some researchers consider these granulomatous reactions associated with malignancies as peculiar hypersensitivity response to malignant cells, or to some persistent infection, while others consider it as protective phenomenon with a good prognosis.[9] Granulomatous mycosis fungoides is a close differential diagnosis of granulomatous slack skin syndrome. Even though they share overlapping histologic features, LeBoit et al. had identified certain pathological features to distinguish between the two [Table - 1].[10] Generalized cutis laxa is differentiated from granulomatous slack skin syndrome by its frequent facial skin involvement and flexural sparing. In anetoderma, lesions are usually smaller with random distribution and there is no association with systemic elastolysis. Mid-dermal elastolysis also mimics slack skin syndrome, but the wrinkling is of crinkle type and there is no tendency to develop into pendulous folds. Furthermore, early lesions of granulomatous slack skin may mimic patches and plaques of classical mycosis fungoides.[6] A case of granulomatous slack skin, mistaken for leprosy and treated with dapsone and rifampicin has also been described.[9]
There is no standard treatment protocol for this condition and the choice of a particular regimen will entirely depend on the stage of the disease. The treatment options include topical nitrogen mustard, psoralen and ultraviolet A, corticosteroids, retinoids, radiotherapy, interferon alpha, poly-chemotherapy (Cyclophosphamide, doxorubicin, vincristine and prednisolone- CHOP) and total skin electron beam irradiation, which can be employed either in isolation or in a multimodal setting.[4] However, none of these appears to provide sustained satisfactory clinical outcomes. The surgical treatment of excising the redundant skin for esthetic and functional improvement has a high relapse rate.[1] Even though the 5-year disease-specific survival of this condition is close to 100%, its association with lymphoproliferative disorders warrants a lifelong close follow-up.[2]
Conclusion
Our case contributes to the further understanding of this rare condition. In addition, we were unable to find any previous reports of granulomatous slack skin syndrome rapidly involving the nonintertriginous areas, sparing the classical sites.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Kempf W, Ostheeren-Michaelis S, Paulli M, Lucioni M, Wechsler J, Audring H, et al. Granulomatous mycosis fungoides and granulomatous slack skin: A multicenter study of the cutaneous lymphoma histopathology Task Force Group of the European Organization for Research and Treatment of Cancer (EORTC). Arch Dermatol 2008;144:1609-17.
[Google Scholar]
|
| 2. |
Willemze R, Jaffe ES, Burg G, Cerroni L, Berti E, Swerdlow SH, et al. WHO-EORTC classification for cutaneous lymphomas. Blood 2005;105:3768-85.
[Google Scholar]
|
| 3. |
Ackerman AB: Granulomatous slack skin; in Ackerman AB (ed): Histologic diagnosis of inflammatory skin diseases. Philadelphia, Lea and Febiger, 1978, pp 483-85.
[Google Scholar]
|
| 4. |
Shah A, Safaya A. Granulomatous slack skin disease: A review, in comparison with mycosis fungoides. J Eur Acad Dermatol Venereol 2012;26:1472-8.
[Google Scholar]
|
| 5. |
Wang C, Duvic M, Vangipuram R. Slack skin syndrome with granulomatous involvement of the lungs: A case report and literature review. J Clin Exp Dermatol Res 2015;6:304.
[Google Scholar]
|
| 6. |
Van Haselen CW, Toonstra J, van der Putte SJ, van Dongen JJ, van Hees CL, van Vloten WA. Granulomatous slack skin. Report of three patients with an updated review of the literature. Dermatology 1998;196:382-91.
[Google Scholar]
|
| 7. |
Goldsztajn KO, Moritz Trope B, Ribeiro Lenzi ME, Cuzzi T, Ramos-E-Silva M. Granulomatous slack skin. Histopathology diagnosis preceding clinical manifestations by 12 years. J Dermatol Case Rep 2012;6:108-12.
[Google Scholar]
|
| 8. |
Hermes B. Haas N, Czarnetzki BM. Annular elastolytic giant cell granuloma with a spontaneous healing tendency. Hautarzt. 1995 Jul; 46(7):490-3
[Google Scholar]
|
| 9. |
Gutte R, Kharkar V, Mahajan S, Chikhalkar S, Khopkar U. Granulomatous mycosis fungoides with hypohidrosis mimicking lepromatous leprosy. Indian J Dermatol Venereol Leprol 2010;76:686-90.
[Google Scholar]
|
| 10. |
LeBoit PE, Zackheim HS, White CR Jr. Granulomatous variants of cutaneous T-cell lymphoma. The histopathology of granulomatous mycosis fungoides and granulomatous slack skin. Am J Surg Pathol 1988;12:83-95.
[Google Scholar]
|
Fulltext Views
5,864
PDF downloads
2,157





