Translate this page into:
Hailey-Hailey disease complicated by eczema herpeticum
Corresponding author: Dr. Dipankar De, Department of Dermatology, Venereology and Leprology, Postgraduate Institute of Medical Education and Research, Chandigarh, India. dr_dipankar_de@yahoo.in
-
Received: ,
Accepted: ,
How to cite this article: Jain S, Dev A, Rao S, Chatterjee D, De D. Hailey-Hailey disease complicated by eczema herpeticum. Indian J Dermatol Venereol Leprol. doi: 10.25259/IJDVL_203_2024
Dear Editor,
Hailey-Hailey disease (HHD) is a chronic disease with a waxing and waning course. The course of the disease may be complicated by various exacerbating factors such as the summer season, exercise, increased friction, infections, and superimposed bacterial and viral infections. Herein, we present a case of HHD complicated by eczema herpeticum.
A 58-year-old man presented with a 4-year history of macerated lesions in the groin and perianal area associated with pain and bad odour. He had been intermittently using over-the-counter topicals. He reported a recent exacerbation of the lesions with increased pain and ulceration in the same areas for the past 7 days. There was no history of similar complaints among his family members. On examination, well to ill-defined moist, macerated erosions and vegetating plaques were present in both the inguinal folds [Figure 1]. These erosions had polycyclic margins in some areas. Overlying yellowish slough with seropurulent discharge was observed. Lesions of similar morphology were present in the perianal area which were non-oozy in nature and had a more vegetating appearance. Multiple discrete brown keratotic papules that coalesced at places were noted in the axillae and on the nape of the neck. Mucosal examination was normal and no nail changes were observed.

- Well to ill-defined macerated vegetating plaque with polycyclic margins and overlying yellowish slough. Background erythema can be noted.
Tzanck smear performed from the inguinal lesion demonstrated multinucleate giant cells. Potassium hydroxide smear from the lesions did not demonstrate any fungal hyphae or spores. Subsequently, a punch biopsy was performed from the axillary lesion, which on histopathological examination showed epidermal orthokeratosis, focal basal cell vacuolisation, and intraepidermal cleft formation with full thickness acantholysis giving a dilapidated brick wall appearance in the surrounding epidermis [Figure 2a]. A punch biopsy was obtained from the inguinal lesion as well, which on histopathology showed epidermal necrosis and keratinocytes with multinucleation, nuclear enlargement, and intranuclear inclusion bodies. Dermis showed dense perivascular inflammatory infiltrate [Figure 2b]. Immunohistochemistry for herpes simplex virus 1 (using rabbit polyclonal herpes simplex virus1 and herpes simplex virus2 by Cell Marque) was performed which showed nuclear positivity [Figure 3]. This case was managed with low-dose naltrexone (5 mg per day) along with valacyclovir 1 g twice a day for 7 days. Pain decreased significantly within 3 days of initiation of treatment and the lesions healed completely within 1 month of treatment [Figure 4].
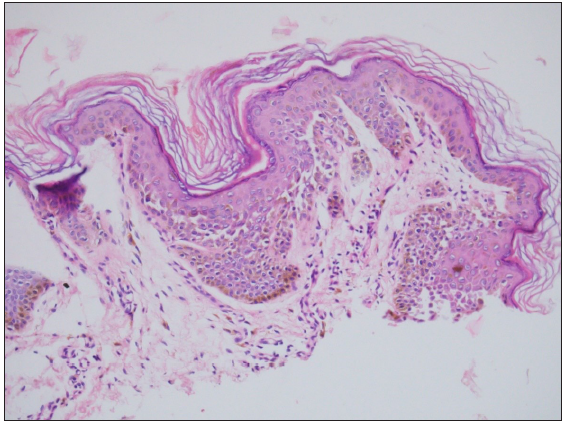
- Epidermal orthokeratosis, focal basal cell vacuolisation, and intraepidermal cleft formation with full thickness acantholysis giving a dilapidated brick wall appearance in the surrounding epidermis. (Haematoxylin and eosin, 40x)
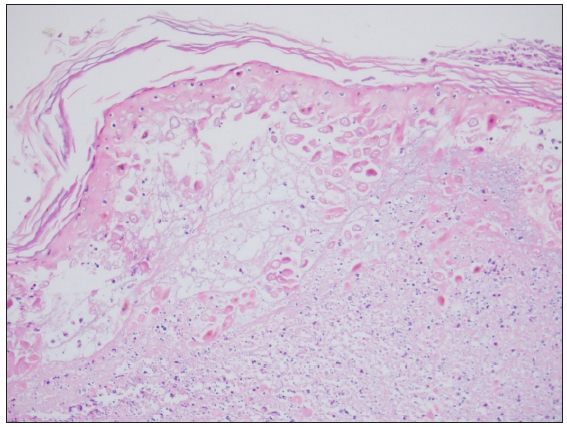
- Inguinal lesion showing necrosis and keratinocytes with nuclear enlargement and intranuclear inclusion bodies. A dense perivascular inflammatory infiltrate can be noted in the dermis. (Haematoxylin and eosin, 100x)
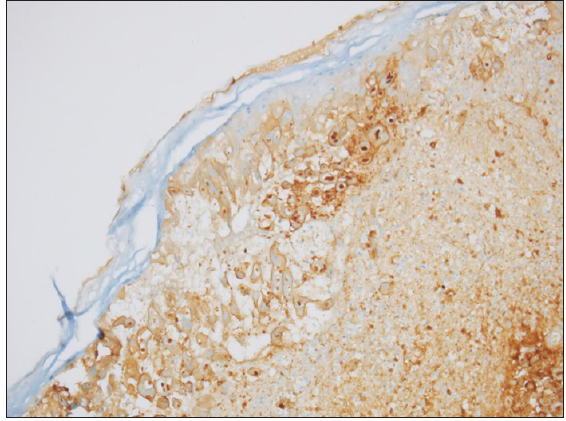
- Immunohistochemistry for herpes simplex virus 1 showing nuclear positivity. (IHC Stain: Rabbit polyclonal HSV1 and HSV2 by Cell Marque, 200×)

- Complete healing with post-inflammatory depigmentation after 3 months of therapy with low-dose naltrexone.
HHD is a relatively uncommon autosomal dominant disorder that is attributed to a mutation in the ATP2C1 gene that leads to dysfunction of the Ca2+ ATPase of the Golgi apparatus. The altered Ca2+ signalling results in flaccid blisters and erosions predominantly in the intertriginous areas. The lesions are moist and malodorous and significantly affect the quality of life of the patients.
The disease was named after the Hailey brothers who first described the entity.1 The name ‘recurrent herpetiform dermatitis repens’ was proposed by Ayers and Anderson for the disease owing to the striking morphological similarity of the early vesicles to Herpes simplex infection but they did not find or look for any evidence of the infection in the lesions.2 Leppard et al. first reported the occurrence of a severe relapse of HHD secondary to herpes simplex infection.3
The occurrence of herpes simplex infection in a case of HHD has several implications.4 The pan-epidermal acantholysis in HHD may predispose the patient to a super-infection by various organisms including herpes simplex virus that is known to cause eczema herpeticum in predisposed patients with skin barrier defects. Secondly, the infection causes a painful relapse of the disease which may be difficult to diagnose without a high index of suspicion since clinically both the diseases can have vesicles and painful erosions. Histopathologically, primary acantholytic disorders can reveal pseudo-herpetic changes but multinucleated cells and nuclear moulding are relatively specific features of herpes infections.5 A confirmatory immunohistochemistry for herpes simplex virus1 antigen may be indispensable in doubtful cases as in ours. Since eczema herpeticum is a potentially life-threatening condition, it requires treatment with systemic antivirals such as high-dose acyclovir or valacyclovir, sometimes without waiting for confirmation of the diagnosis.
Low-dose naltrexone is a novel treatment modality for HHD that inhibits opioid receptors and has shown promising results in the treatment of HHD.6 Other treatment options include topicals like corticosteroids, vitamin D analogues, zinc oxide paste, calcineurin inhibitors, and systemics like oral corticosteroids, oral retinoids, and dapsone. Surgery and ablative therapies like CO2 laser and photodynamic therapy can be utilised in case of recalcitrant lesions. An important cornerstone of management is to avoid exacerbating and precipitating factors by wearing lightweight clothes to avoid friction and sweating.
To conclude, the course of HHD may be complicated by secondary herpes simplex infection. A sudden relapse of the disease presenting with pain and a burning sensation that may be accompanied by new onset vesicles and ulcers with polycyclic margins should raise the suspicion of eczema herpeticum. A simple bedside Tzanck smear demonstrating multinucleate giant cells supports the diagnosis, which can be further confirmed by histopathological examination and immunohistochemistry.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
References
- Familial benign chronic pemphigus. Arch Dermatol. 1939;39:679-85.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic benign familial pemphigus. Induction of lesions by herpesvirus hominis. Br J Dermatol. 1973;88:609-13.
- [CrossRef] [PubMed] [Google Scholar]
- A case of eczema herpeticum with hailey-hailey disease. Ann Dermatol. 2009;21:311-4.
- [CrossRef] [PubMed] [Google Scholar]
- Hailey-hailey disease with coexistent herpes virus infection: Insights into the diagnostic conundrum of herpetic/pseudoherpetic features in cutaneous acantholytic disorders. Am J Dermatopathol. 2018;40:749-53.
- [CrossRef] [PubMed] [Google Scholar]
- Hailey-Hailey disease treated successfully with naltrexone and magnesium. JAAD Case Rep. 2019;5:760-2.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]





