Translate this page into:
Hand, foot and mouth disease in Nagpur
Correspondence Address:
Vikrant A Saoji
22, Dandige Layout, Shankar Nagar, Nagpur - 440 010, Maharashtra
India
| How to cite this article: Saoji VA. Hand, foot and mouth disease in Nagpur. Indian J Dermatol Venereol Leprol 2008;74:133-135 |
Abstract
Hand, foot and mouth disease (HFMD) is a viral infection of children caused by Coxsackie virus-A16, a type of enterovirus closely related with the virus that causes herpangina. Although seen worldwide, it is not common in India. Hand, foot and mouth disease is sporadically reported from India as a mild illness. This report describes four cases of HFMD from Nagpur, Central India, seen between September 2005 and April 2006. All patients presented with a mild febrile prodrome followed by the appearance of aphthous-like oral ulcers and vesicular lesions on the hands and feet. All cases were clinically diagnosed. Coxsackie virus A16 was isolated from the serum of one of the patients. All the patients were in the age group of 3-5 years from different schools. It was a mild illness and all the four patients recovered without any complication. There were no secondary cases in the families.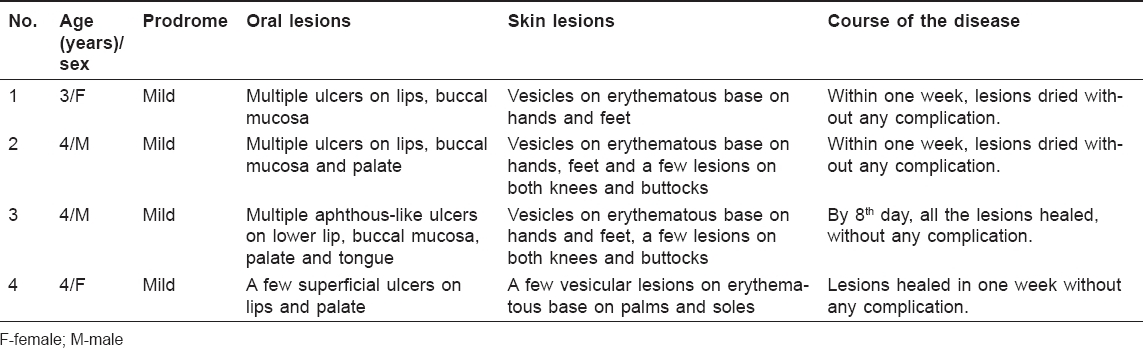
 |
| Figure 3: Skin lesions on buttocks in patient no. 3 |
 |
| Figure 3: Skin lesions on buttocks in patient no. 3 |
 |
| Figure 2: Cutaneous lesions on the feet in patient no. 3 |
 |
| Figure 2: Cutaneous lesions on the feet in patient no. 3 |
 |
| Figure 1: Oral ulcers in patient no. 2 |
 |
| Figure 1: Oral ulcers in patient no. 2 |
Introduction
Hand, Foot and Mouth Disease (HFMD) is a viral infection seen worldwide. Which mostly affects children below ten years of age. It is usually caused by Coxsackie A16, an enterovirus, closely related with the virus that causes herpangina. Enteroviruses include polio virus, coxsackie virus types A and B and ECHO viruses. HFMD may occur in an epidemic or sporadic form. HFMD epidemics are usually due to c oxsackie type A16 and sporadic cases are due to types A5 and A10. [1] Incubation period ranges from 5 to 7 days. Illness begins with a mild fever of short duration followed by oral and skin lesions. Oral lesions appear as vesicles, which rapidly ulcerate producing multiple small superficial ulcers with erythematous halos. The ulcers resemble aphthous ulcers and are usually seen on the tongue, palate, buccal mucosa, gums and lips. Oral ulcers cause discomfort, making oral feeding difficult. This enanthem is followed by skin lesions. Skin lesions are vesicles on erythematous bases similar to lesions of varicella but are more elongated and oval. The lesions are present prominently on the hands and feet. Sometimes, the exanthem is more widespread involving the buttocks, knees and elbows. [1] Lesions usually subside in 5-7 days. HFMD is usually a mild illness but sometimes meningitis, encephalitis and polio-like paralysis may occur. Diagnosis of HFMD is usually made based on clinical characteristics but can be confirmed by viral isolation from stool, vesicular fluid or blood. Serological tests are also available. Many deaths have been reported due to severe outbreaks of HFMD from many Asian countries. [2],[3],[4] It is not commonly seen in India; only a few reports are available. This report describes four cases of HFMD seen in Nagpur, Central India.
Case Reports
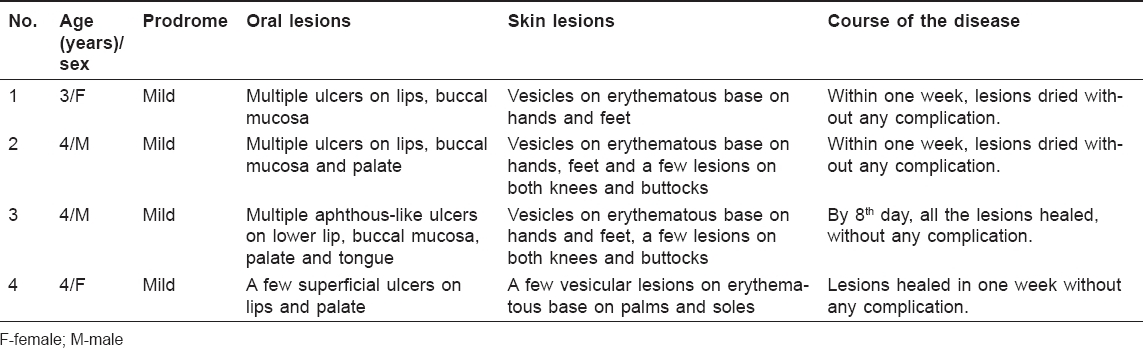
Four cases, two male and two female ranging in age from 3 to 5 years are presented in [Table - 1]. The first case was seen in September 2005 and the last case in April 2006 [Figure - 1],[Figure - 2],[Figure - 3]. All were nursery students, studying in different schools and staying in different localities of Nagpur. All the patients were from educated, middle-class families. A mild prodrome of 1-2 days was followed by the appearance of oral lesions. Aphthous-like oral ulcers were present on the lips, buccal mucosa and palate and led to feeding difficulty. Skin lesions appeared a further 1-2 days later and were seen as oval or circular vesicles on erythematous bases. In all these cases, the diagnosis of HFMD was made on clinical grounds because of the characteristic clinical presentation of oral ulcers and vesicular lesions on the hands and feet. In all the four patients, it was a mild illness with healing of the lesions in 7-8 days without any complication. The patients were treated symptomatically with antihistaminics and calamine lotion. There were no secondary cases in the families of these patients. Coxsackie A16 was detected using RT-PCR from the serum sample of one of the patients (Case 4).
Discussion
In all our four cases, diagnosis of HFMD was clinical and based on the typical presentation of oral ulcers and lesions on the hands and feet. However, we could demonstrate coxsackie A16 virus in the serum in one case. These cases could represent a small outbreak in our city. Due to the mild nature of the illness and the lack of awareness amongst doctors, it is possible that some of the cases could have been overlooked. Due to prominent skin manifestations of HFMD, patients may first consult a dermatologist. Oral lesions of HFMD can be easily misdiagnosed as aphthous ulcers or the exanthem can be misdiagnosed as varicella. However, varicella rarely presents with oral lesions and the skin lesions are more concentrated on the trunk, only rarely affecting the palms and soles. Herpangina is a viral infection of children caused by a type A coxsackie virus which presents with similar types of oral ulcers but are more extensive involving the tonsils, pharyngeal mucosa, soft palate and the posterior part of buccal mucosa. [1] Unlike HFMD, there are no skin lesions in herpangina.
Enteroviruses multiply in the gastrointestinal tract and are transmitted by the feco-oral route. Good hygienic practices are the most important preventive strategies. As virological studies are not easily available in developing countries like India, the diagnosis of HFMD is often made on clinical grounds alone. HFMD is commonly caused by coxsackie virus A16 and Enterovirus 71 but is also reported with coxsackie virus A5, A7, A9, A10, B2, B3 and B5. [5] HFMD caused by Coxsackie virus A16 (CV-A16) is usually a mild disease and the patient recovers in 5-7 days without any complication. [2] Rarely is HFMD severe, leading to meningitis, encephalitis, poliomyelitis-like paralysis and even death. [2] Many deaths occurred due to a severe outbreak of HFMD due to Enterovirus 71 (EV71) in Malaysia, [2] Taiwan [3] and Singapore. [4] Although major outbreaks have been reported from Asian countries, not many cases are reported from India. Sasidharan et al. reported 81 cases of HFMD from Calicut, seen between October 2003 and February 2004. [6] Although this outbreak was caused by EV71, it was a mild illness without any complication or mortality. Coxackie virus A16 was isolated from one of our patients which indicates that the present outbreak in Nagpur is not related with the outbreak reported from Kerala (due to EV71) and there may be different serotypes prevalent in the country. There are various subtypes of EV71 and only some of the subtypes such as B4 and C2 are associated with severe disease, whereas subtype B3 is associated with mild disease. [2] Genetic recombination is known to occur between various subtypes producing new subtypes with differing pathogenic potentials. [2]
There is no normal enteric virus flora. Usually only one type of enterovirus multiplies within the intestine of an individual at any given time. Polio vaccination has eliminated polio viruses from the gut, thereby increasing the chances of coxsackie viral and echoviral infections. [7] It is possible that the emergence of HFMD in India may be related to the mass polio vaccination. However, a firm conclusion can be made in this regard only after studying a large number of cases of HFMD over a period of time. Moreover, in today′s aviation era, it is very easy for organisms to be transferred from one part to another part of our country, spreading the disease. A small outbreak of HFMD can become a major epidemic and because of genetic recombination of viruses, a benign illness can become a deadly disease as has happened in many Asian countries. It is important for dermatologists to be aware of this disease as they may be the first health care professional to be consulted in such cases.
Acknowledgment
The author wishes to thank Dr. Satish Deopujari and Dr. Vikram Rajan for referring the cases and also to Rota-Enterovirus group, National Institute of Virology, Pune for carrying out virological studies in our patients.
| 1. |
Sterling JC. Virus infections. In : Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook's textbook of dermatology. 7 th ed. Oxford: Blackwell Science; 2004. p. 25.1-83.
th ed. Oxford: Blackwell Science; 2004. p. 25.1-83.'>[Google Scholar]
|
| 2. |
Chan YF, AbuBakar S. Recombinant human enterovirus 71 in hand foot and mouth disease patients. Emerg Infect Dis 2004;10:1468-70.
[Google Scholar]
|
| 3. |
Chang LY, King CC, Hsu KH, Ning HC, Tsao KC, Li CC, et al . Risk factors of enterovirus 71 infection and associated hand foot and mouth disease/herpangina in children during epidemic in Taiwan. Pediatrics 2002;109:e88.
[Google Scholar]
|
| 4. |
Shah VA, Chong CY, Chan KP, Ng W, Ling AF. Clinical characterstic of an outbreak of hand foot and mouth disease in Singapore. Ann Acad Med Singapore 2003;32:381-7.
[Google Scholar]
|
| 5. |
Frieden IJ. Viral exanthems. In : Aly R, Maibach HI, editors. Atlas of infections of the skin. Churchil Livingstone: 1999. p. 231-43.
[Google Scholar]
|
| 6. |
Sasidharan CK, Sugathan P, Agrawal R, Khare S, Lal S, Paniker J. Hand-foot-and-mouth disease in Calicut. Indian J Pediatr 2005;72:17-21.
[Google Scholar]
|
| 7. |
Martin LA. Enteric viruses. In : Petersdorf RG, Adams RD, Braunwald E, Isselbacher KJ, Martin JB, Wilson JD, editors. Harrison's principles of internal medicines. 10 th ed. McGraw-Hill International Book Company; 1983. p. 1125-32.
th ed. McGraw-Hill International Book Company; 1983. p. 1125-32.'>[Google Scholar]
|
Fulltext Views
5,987
PDF downloads
1,910





