Translate this page into:
Helicobacter-induced pyoderma gangrenosum–like skin ulcers in a case of Bruton’s agammaglobulinemia
Corresponding author: Dr. Sujay Khandpur, Department of Dermatology and Venereology, All India Institute of Medical Sciences, New Delhi, India. sujay_khandpur@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Swarnkar B, Anand GRP, Khandpur S, Panda AK, Sharma M. Helicobacter-induced pyoderma gangrenosum-like skin ulcers in a case of Bruton’s agammaglobulinemia. Indian J Dermatol Venereol Leprol. 2024;90:230–2. doi: 10.25259/IJDVL_794_2022
Dear Editor,
A 20-year-old underweight and stunted boy, a known case of Bruton’s agammaglobulinemia, presented with painful ulcers over both lower legs and left foot for 2 years. The lesions started as painful reddish swellings which ulcerated within a few weeks to leave behind small ulcers. The ulcers gradually increased to the present size of around 6 × 5 cm and 4 × 3 cm over the medial malleolus and lower third of the right leg, respectively, and 20 × 10 cm over the left leg and foot [Figure 1]. The ulcers showed necrotic slough over the granulation tissue, hyperpigmented thick margin and were tender to touch.

- Ulcer involving the lower third of the left leg and dorsum of the left foot.
There was no history suggestive of the pathergy phenomenon. The patient gave a history of recurrent fever, lower respiratory tract and gastrointestinal tract infections since early childhood, the frequency of which had decreased over time.
He has been on replacement monthly intravenous immunoglobulin therapy for Bruton’s agammaglobulinemia since 10 years of age. In the past, a dermatologist at his native place had administered multiple short courses of antibiotics and apremilast with no improvement in ulcers. There was no history of agammaglobulinemia in the family. There was no evidence of varicose veins over the lower limbs or significant lymphadenopathy. Based on the history and examination, we kept the clinical differentials of pyoderma gangrenosum, cutaneous tuberculosis, atypical mycobacterial infection and deep fungal infection.
A biopsy from the ulcer edge showed irregular epidermal acanthosis [Figure 2a]. The dermis showed proliferating capillaries and a diffuse infiltrate of neutrophils, lymphocytes and histiocytes with focal extravasation of red blood cells [Figure 2b]. X-rays of bilateral legs showed diffuse osteopenia. Pus culture was sterile.
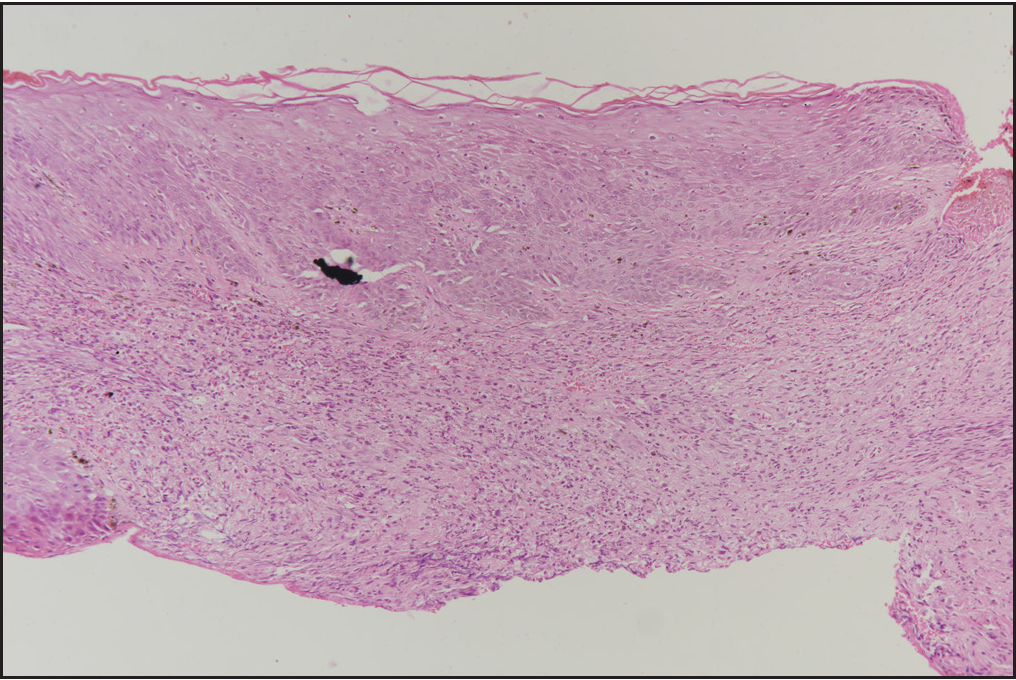
- Ulcer edge biopsy shows irregular epidermal acanthosis and diffuse dermal infiltrate of neutrophils, lymphocytes and histiocytes. (H&E-100×)
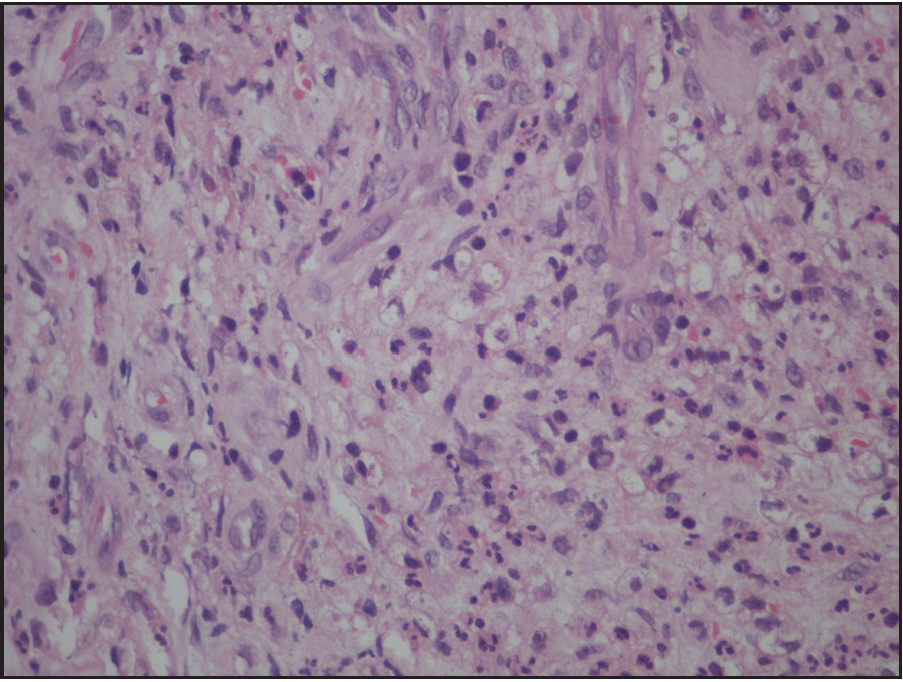
- The dermis shows proliferating capillaries and a diffuse infiltrate of neutrophils, lymphocytes and histiocytes with focal extravasation of red blood cells. (H&E-400×)
With the clinical possibility of pyoderma gangrenosum, we started the patient on oral dapsone, thalidomide and topical potent corticosteroid (clobetasol propionate 0.05%). Given the background of primary immunodeficiency disease, we avoided oral corticosteroids and cyclosporine. Physiotherapy, regular dressing of ulcers, non-steroidal anti-inflammatory drugs (ibuprofen and paracetamol combination) and amoxicillin-clavulanic acid combination were also given. After 2 months, the ulcer size worsened.
Given no response to therapy and the possibility of chronic infection in an immunocompromised individual, we did a literature search and found reports of Helicobacter-induced ulcers in Bruton’s agammaglobulinemia cases. Based on the suspicion of Helicobacter in our patient, we ordered a Warthin starry stain on the biopsy section which revealed elongated, brownish-black, curvilinear rods [Figure 3]. The tissue and blood culture did not reveal Helicobacter while polymerase chain reaction–based tests were not available in our institute.
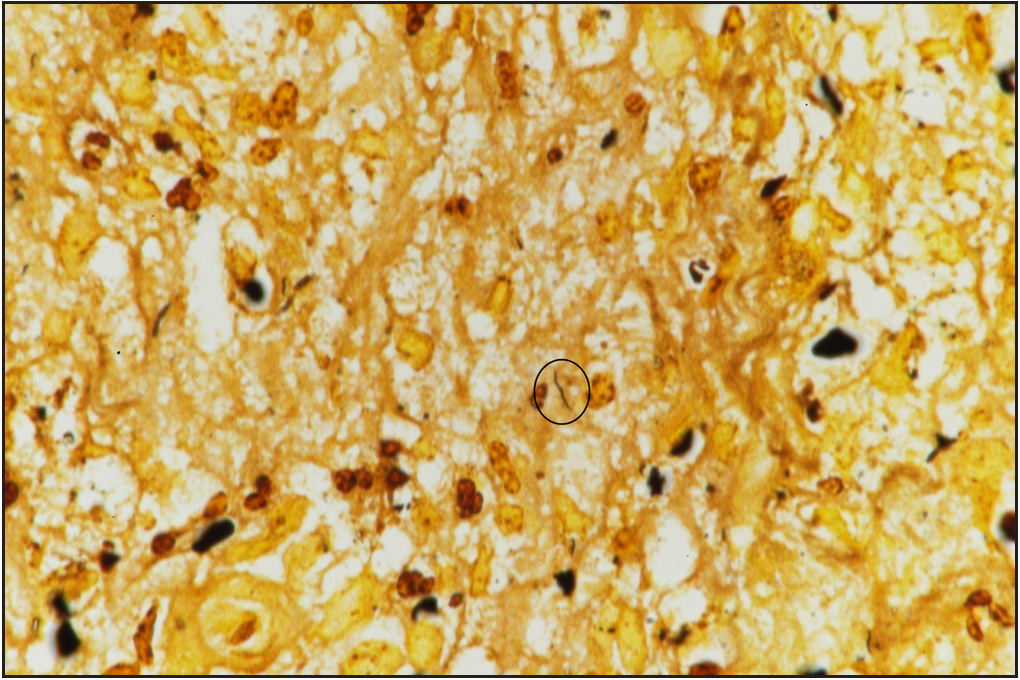
- Elongated, brownish-black, curvilinear rods (encircled with a black circle). (Warthin starry stain-1000×)
We made the final diagnosis of Helicobacter-induced pyoderma gangrenosum–like skin ulcers in a case of Bruton’s agammaglobulinemia and started ertapenem injection (1 g/day) and doxycycline tablet (100 mg/day). Ertapenem was changed to clarithromycin tablet (500 mg/day) after 4 weeks. After 4.5 months of therapy, there was complete resolution of right leg ulcers while the left leg ulcer showed significant re-epithelisation [Figure 4]. The patient is being continued on the same regime (doxycycline plus clarithromycin) with further healing of ulcers without any side-effects till now. There was no history of gastrointestinal symptoms, urticaria or prurigo in the patient.

- Left leg ulcer showed significant re-epithelisation.
The genus Helicobacter includes two species, namely, gastric and enterohepatic. Enterohepatic Non-Helicobacter Pylori Helicobacter can cause disease, especially in immunocompromised individuals like those with Bruton’s agammaglobulinemia, acquired immunodeficiency syndrome, asplenia and liver cirrhosis. The infection source is unknown, but the migration of these organisms from the gastrointestinal tract and zoonosis are the accepted hypotheses. Clinically, most relevant species like Helicobacter cinaedi and Helicobacter bilis colonise the biliary tract, intestine and liver of animals and humans. The natural hosts of Helicobacter cinaedi are dogs, hamsters and rhesus macaques and of Helicobacter bilis are cats and mice. These species have been found to be associated with bacteremia and systemic illness in humans supporting the hypothesis of zoonosis. The clinical manifestations include cellulitis, abscess formation, cutaneous ulcers, pleurisy, synovitis, suppurative cholangitis and sepsis.1 The lower extremity followed by the upper extremity is the commonest site of cutaneous involvement. There are no specific management guidelines for such cases but combination antibiotics have been used in the past with variable responses.
There are a few reports in the literature of cutaneous ulcers induced by Helicobacter in Bruton’s agammaglobulinemia [Table 1].
| Author | Age (years)/Gender | Helicobacter species (sample analysed) | Clinical manifestation | Treatment | Response |
|---|---|---|---|---|---|
| Cuccherini et al., 20002 | 21/Male | Helicobacter-like organisms (blood) | Leg ulcer, synovitis, fever, osteomyelitis | Imipenem and gentamicin followed by imipenem and meropenem (9 months) | Substantial improvement |
| Murray et al., 20103 | 17/Male | Helicobacter bilis (skin) | Leg ulcer | Tobramycin and meropenem (2.5 months) | Almost complete healing |
| Dua et al., 20114 | 26/Male | Helicobacter cinaedi (skin) | Leg ulcer, synovitis | Amikacin and meropenem (1 month) followed by doxycycline and ertapenem (2 months) | Ulcer reduced in size; joint pain resolved |
| Sharp, 20115 | 25/Male | Helicobacter fennelliae (skin) | Lower limb ulcers | - | - |
| Gonzalez et al., 20221 | 18/Male | Helicobacter bilis (skin) | Leg ulcer, osteomyelitis | Multiple (2 years) | No response |
Ours is a rare case of Helicobacter-induced leg ulcers responding to long-term antibiotics. This diagnosis must be considered in an immunocompromised individual presenting with pyoderma gangrenosum–like ulcers.
Declaration of patient consent
Patient’s consent not required as patients identity is not disclosed or compromised.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Infections with enterohepatic non-H. pylori helicobacter species in X-linked agammaglobulinemia: Clinical cases and review of the literature. Front Cell Infect Microbiol. 2022;11:807136.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Bacteremia and skin/bone infections in two patients with X-linked agammaglobulinemia caused by an unusual organism related to Flexispira/Helicobacter species. Clin Immunol. 2000;97:121-9.
- [CrossRef] [PubMed] [Google Scholar]
- Pyoderma gangrenosum-like ulcer in a patient with X-linked agammaglobulinemia: identification of Helicobacter bilis by mass spectrometry analysis. Arch Dermatol. 2010;146:523-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Pyoderma gangrenosum-like ulcer caused by Helicobacter cinaedi in a patient with X-linked agammaglobulinaemia. Clin Exp Dermatol. 2012;37:642-5.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic skin lesions from a patient with Bruton’s X-linked agammaglobulinemia. J Clin Microbiol. 2011;49:483,770.
- [CrossRef] [PubMed] [Google Scholar]





