Translate this page into:
Henoch-Schonlein purpura : Yet another disease manifesting the Koebner phenomenon
Correspondence Address:
Sudhir U.K Nayak
Department of Dermatology, Kasturba Medical College, Manipal University, Manipal-576104
India
| How to cite this article: Nayak SU, Shenoi SD, Pai B S, Prabhu S. Henoch-Schonlein purpura : Yet another disease manifesting the Koebner phenomenon. Indian J Dermatol Venereol Leprol 2013;79:135 |
Sir,
A 60-year-old housewife presented with asymptomatic reddish lesions on extremities of 3 weeks duration. There was a history of abdominal pain with blood-stained diarrhea and joint pain. There was no history of passing high colored urine, history of any prior drug intake, pruritus, or any other systemic complaints. There was no previous history of similar complaints. Examination revealed palpable and non-palpable purpurae over the extremities, gluteal region, and lower abdomen [Figure - 1]. Some of the purpurae were arranged in a linear pattern especially over the lower extremities [Figure - 2]. A clinical diagnosis of Henoch-Schonlein purpura (HSP) with Koebner′s phenomenon was made.
 |
| Figure 1: Henoch-Schonleinpurpura (HSP) on legs with Koebner's phenomenon |
 |
| Figure 2: Koebner's phenomenon at multiple sites |
The laboratory investigations, such as complete blood picture and stool examination for occult blood were within normal limits. Urine microscopy showed the presence of protein but analysis of 24-h urine for protein was within the permissible range. The anti-Streptolysin O (ASO) titer, C-reactive protein, and complement levels were in the normal range. Biopsy on histopathology showed features of leukocytoclastic vasculitis and, on direct immunofluorescence showed immunoglobulin A (IgA) deposits in the blood vessels, confirming the diagnosis of HSP [Figure - 3].
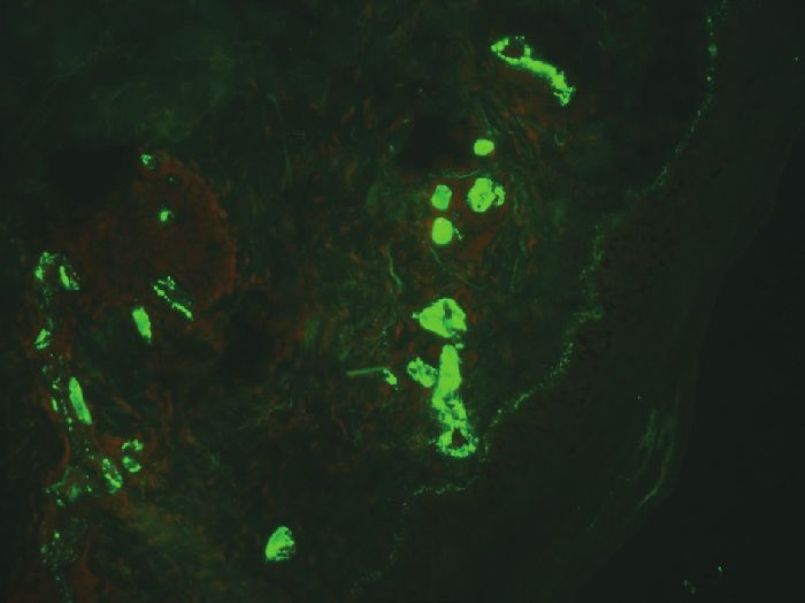 |
| Figure 3: Direct immunofluorescence showing IgA blood vessel deposits (×20) |
Patient was started on oral methylprednisolone 32 mg/day. In spite of such a high dose, the patient was getting new lesions with many lesions being arranged in a linear pattern that necessitated an increase in dose with which the lesions were subsided. The HSP is a small vessel vasculitis characterized by involvement of the skin (in the form of purpura), gastrointestinal, and renal systems (hematuria and proteinuria) with or without arthralgia or arthritis. The purpura commonly involves the extensors of the limbs and buttocks, occasionally involving the trunk and face. The HSP on histopathology shows the presence of leukocytoclastic vasculitis. The diagnosis of HSP is made by direct immunofluorescence where there is presence of perivascular IgA deposits, a feature that differentiates HSP from other vasculitides.
Koebner phenomenon, described first by Heinrich Koebner, is the development of isomorphic pathologic lesions in traumatized uninvolved skin of patients who have cutaneous diseases. [1] The trauma can either be external or internal. In certain diseases, such as psoriasis, trauma is followed by new lesions in the traumatized but otherwise normal skin, and these are clinically and histopathologically identical to those in the diseased skin. The three disease processes that display the true isomorphic response of Koebner are psoriasis, lichen planus, and vitiligo. Questionable isomorphic phenomenon has been described with anaphylactoid purpura and vasculitis. [1] The exact pathogenesis of Koebner phenomenon is unknown. The pathogenic factors that are speculated include immunologic, vascular, dermal, enzymatic, inhibitory, neural, growth, genetic, and hormonal factors. Capillary changes in the dermis are purported to precede all other morphologic changes. [1] Our patient in spite of being started on high doses of corticosteroids was developing fresh purpura with Koebner phenomenon, thus indicating disease activity. Itching owing to xerosis may be the reason for Koebner phenomenon in our patient. Immune complex deposition caused by scratching-induced vasodilatation and stasis is postulated to be a reason for Koebner′s phenomenon. [2],[3] Extensive search for Koebner phenomenon in HSP revealed the presence of only two case reports. [4],[5] Reverse Koebner phenomenon, that is, the non-appearance or disappearance of lesions has also been described in vasculitis. [6] This case is being reported for the rarity of occurrence of Koebner phenomenon in HSP and also being an indicator of disease activity.
| 1. |
Thappa DM. The isomorphic phenomenon of Koebner. Indian J Dermatol Venereol Leprol 2004;70:187-9.
[Google Scholar]
|
| 2. |
De D, Dogra S, Kanwar AJ. Isomorphic response of Koebner in a patient with cutaneous small vessel vasculitis. J Eur Acad Dermatol Venereol 2008;22:1125-6.
[Google Scholar]
|
| 3. |
Chan LS, Cooper KD, Rasmussen JE. Koebnerization as a cutaneous manifestation of immune complex-mediated vasculitis. J Am Acad Dermatol 1990;22:775-81.
[Google Scholar]
|
| 4. |
Green ST, Natarajan S. The Koebner phenomenon in anaphylactoid purpura. Cutis 1986;38:56-7.
[Google Scholar]
|
| 5. |
Nischal KC, Uday K, Urmila B. Koebner's phenomenon in Henoch Schoenlein purpura and role of pressure in its causation. Dermatol Online J 2007;13:26.
[Google Scholar]
|
| 6. |
Yadav S, De D, Kanwar AJ. Reverse koebner phenomenon in leukocytoclastic vasculitis. Indian J Dermatol 2011;56:598-9.
[Google Scholar]
|
Fulltext Views
4,025
PDF downloads
3,297





