Translate this page into:
Hidradenocarcinoma of the chest
Correspondence Address:
Ana Brasileiro
Department of Dermatology, Hospital Santo Ant�nio dos Capuchos, Centro Hospitalar Lisboa Central, Lisbon
Portugal
| How to cite this article: Brasileiro A, Lencastre A, Joao A, Apetato M. Hidradenocarcinoma of the chest . Indian J Dermatol Venereol Leprol 2014;80:568-569 |
Sir,
Sweat gland tumors, especially those of a malignant nature remain an elusive area of knowledge for dermatologists, oncologists and pathologists. Due to the paucity of published literature, there is not only a lack of consensus over histopathological classification but also on their optimal management. We report a middle-aged patient with clear cell hidradenocarcinoma who was successfully treated with wide local excision and sentinel lymph node dissection.
A 49-year-old male reported a 13-month history of an asymptomatic, ulcerated, pink exophytic nodule measuring 3 cm in diameter and located on the right parasternal area [Figure - 1]. His past medical history was non-contributory though he stated that a similar lesion was present 8 months ago which was excised at another center and whose histology results he was not aware of. He described a rapid relapse and growth of the lesion soon after this procedure. Surgical excision with 2 cm margins revealed a poorly circumscribed ulcerated tumor in continuity with the epidermis [Figure - 2], with large cords and confluent areas of basaloid cells, occupying the entire dermis and part of the hypodermis [Figure - 3]. Several areas of necrosis and mitoses were observed within the tumor limits. Cells were AE1/AE3 positive; epithelial membrane antigen (EMA) and carcinoembryonic antigen (CEA) negative. Sentinel lymph node biopsy was negative. Thoraco-abdomino-pelvic computed tomography did not show any pathological findings. In view of the lack of local or distant metastasis, local widening of the tumor bed was performed such that no residual tumor was detected. The patient remains disease free for the past 24 months.
 |
| Figure 1: Pink ulcerated nodule on the chest. The preceding surgery scar can be seen in the background |
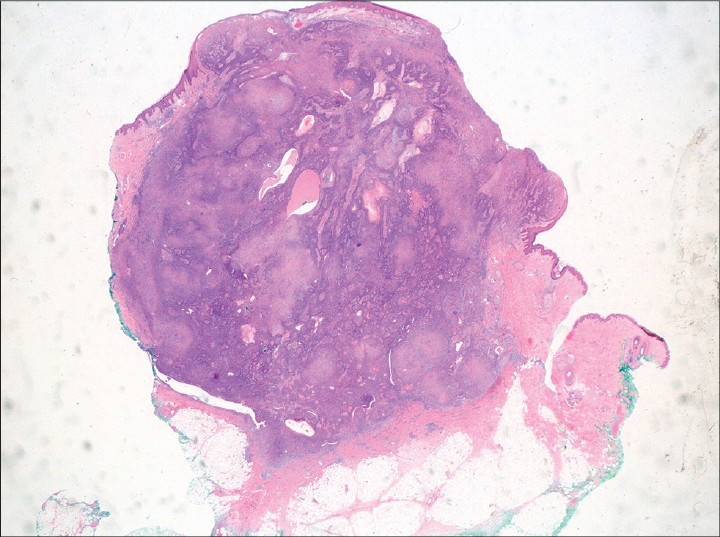 |
| Figure 2: Poorly circumscribed ulcerated tumor with several areas of necrosis (H and E, ×10) |
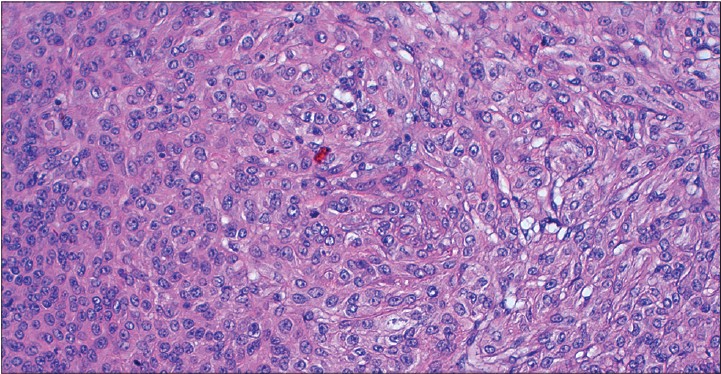 |
| Figure 3: Large cords and confluent areas of basaloid cells, some with cytoplasmatic vacuoles. In addition, there are areas with clear cells, atypical cells, and cystic spaces filled with eosinophilic material (H and E, ×200) |
Clear cell hidradenocarcinoma is one of the most common forms of the rare eccrine sweat gland carcinomas. It arises from the eccrine apparatus and is known for aggressive behavior with high rates of local recurrences and metastases. Clinically, it appears most commonly on the face, hands, or feet, starting as an asymptomatic solitary skin lesion with a pink, blue, or purple surface, which may ulcerate. It usually expands slowly, but sudden spontaneous spurts of growth may occur. [1] Lack of any characteristic clinical findings usually leads to a delay in the diagnosis by which time the loco-regional spread to lymph nodes or visceral metastasis to bone and lungs may have already occurred, making the course and prognosis of clear cell hidradenocarcinoma different from the commoner skin tumors. Only the "accelerated" growth mentioned by the patient raised our suspicion in this case, as the location was also not typical.
On histology, sheets of pale, glycogen-rich cells form the tumor. Rudimentary lumina formation within cells seen as intracellular vacuoles are an important feature, as is the cyto-architectural atypia. The number of mitoses and degree of atypia varies and some tumors may have a deceptively innocent appearance. [2] Usually, tumors express CK5, CK7, and AE1/AE3 antigens. CEA and EMA expression is variable. [3] The treatment needs to be individualized and decisions are taken on a case-to-case basis relying on the experience of the attending physician. Surgical technique and adjuvant radiotherapy or chemotherapy all remain areas of controversy. [1],[2] We opted to widen the primary tumor margins with sentinel lymph node dissection when marginal tumor remnants were observed on the first histological examination. The use of radiotherapy has been demonstrated to be useful in cases of moderately to poorly differentiated tumors. [1] Chemotherapy with capecitabine has been reportedly useful in a few cases of extensively metastatic disease. [4] Recently published research points towards a potential role for targeted therapy in metastasizing adnexal carcinomas. [2],[5] Further work needs to be done to assess their applicability in this setting.
| 1. |
Souvatzidis P, Sbano P, Madato F, Fimiani M, Castelli A. Malignant nodular hidradenoma of the skin: Report of seven cases. J Eur Acad Dermatol Venereol 2008;22:549-54.
[Google Scholar]
|
| 2. |
Gauerke S, Driscoll JJ. Hidradenocarcinomas - A brief review and future directions. Arch Pathol Lab Med 2010;134:781-5.
[Google Scholar]
|
| 3. |
Ko CJ, Cochran AJ, Eng W, Binder SW. Hidradenocarcinoma: A histological and immunohistochemical study. J Cutan Pathol 2006;33:726-30.
[Google Scholar]
|
| 4. |
Lerner A, Beckford A, Ugent S, Goldberg L, Jalisi S, Demierre MF. Complete response of metastatic malignant hidradenocarcinoma to capecitabine treatment. Arch Dermatol 2011;147:998-9.
[Google Scholar]
|
| 5. |
Dias-Santagata D1, Lam Q, Bergethon K, Baker GM, Iafrate AJ, Rakheja D, etal. A potential role for targeted therapy in a subset of metastasizing adnexal carcinomas. Modern Pathol 2011;24:974-82.
[Google Scholar]
|
Fulltext Views
3,251
PDF downloads
1,897





