Translate this page into:
High-resolution ultrasound in the assessment of peripheral nerves in leprosy: A comparative cross-sectional study
Corresponding author: Dr. Sarita Sasidharanpillai, “Rohini,” Girish Nagar, Nallalom PO, Kozhikode - 673 027, Kerala, India. saritasclt@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Sreejith K, Sasidharanpillai S, Ajithkumar K, Mani RM, Chathoth AT, Menon PS, et al. High-resolution ultrasound in the assessment of peripheral nerves in leprosy: A comparative cross-sectional study. Indian J Dermatol Venereol Leprol 2021;87:199-206.
Abstract
Background:
Detection of peripheral nerve thickening and nerve function impairment is crucial in the diagnosis and the management of leprosy.
Aims and objectives:
(1) To document the cross-sectional area, echotexture and blood flow of peripheral nerves in healthy controls and leprosy cases using high-resolution ultrasound, (2) to compare the sensitivities of clinical examination and high-resolution ultrasound in detecting peripheral nerve thickening in leprosy.
Methods:
Peripheral nerves of 30 leprosy patients and 30 age- and sex-matched controls were evaluated clinically and by high-resolution ultrasound. When the cross-sectional area of a peripheral nerve on high-resolution ultrasound in a leprosy patient was more than the calculated upper bound of the 95% confidence interval for mean for that specific nerve in controls, that particular peripheral nerve was considered to be enlarged.
Results:
Cross-sectional areas more than 7.1 mm2 for the radial nerve, 8.17 mm2 for ulnar, 10.17 mm2 for median, 9.50 mm2 for lateral popliteal and 11.21mm2 for the posterior tibial nerve were considered as nerve thickening on high-resolution ultrasound. High-resolution ultrasound detected 141/300 (47%) nerves enlarged in contrast to the 60 (20%) diagnosed clinically by palpation (P < 0.001). Clinical examination identified thickening in 31/70 (44.3%) nerves in cases with impairment of nerve function and 29/230 (12.6%) in the absence of nerve function impairment. High-resolution ultrasound detected thickening in 50/70 (71.4%) nerves with impairment of function and in 91/230 (39.6%) nerves without any impairment of function.
Limitation:
A single-centre study design was the major study limitation.
Conclusion:
High-resolution ultrasound showed greater sensitivity than clinical examination in detecting peripheral nerve thickening in leprosy cases. High-resolution ultrasound, may therefore improve the sensitivity of the diagnostic criterion of peripheral nerve enlargement in the diagnosis and classification of leprosy.
Keywords
High-resolution ultrasound
leprosy
peripheral nerve
Plain Language Summary
Leprosy is a disease that affects the skin and nerves. Peripheral nerves (limb nerves) are often affected in leprosy, becoming thickened and losing their functions of sensation and movement control. Peripheral nerve thickening is usually detected clinically by touch, and this is important in diagnosing leprosy. This study (at the Government Medical College, Kozhikode) found that high resolution ultrasound (a type of scan) was better than clinical examination for detecting peripheral nerve thickening in 30 patients of leprosy. For comparison, the normal thicknesses of commonly checked peripheral nerves were also recorded in 30 healthy individuals in this study.
Introduction
Accurate detection of nerve thickening is very important in the classification and treatment of leprosy. Moreover, diagnosis of pure neuritic leprosy could be missed altogether if nerve thickening and nerve function impairment are overlooked.1 Assessment of peripheral nerve thickening by palpation is subjective and may differ between clinicians. Not many studies are available regarding the measurement of normal peripheral nerve thickness using a more objective method such as high-resolution ultrasound, though available literature points to the significance of high-resolution ultrasound in leprosy.2-4
High-resolution ultrasound reveals the nerves as distinct from the surrounding epineurium, giving a characteristic echo pattern in the transverse plane; the dark punctate areas produced by the nerve fascicle groups distributed throughout the hyperechoic background of the perineurium impart a “honeycomb” appearance.5
In this study, we assessed the usefulness of high-resolution ultrasound in measuring the mean cross-sectional areas of peripheral nerves in normal controls and leprosy cases, as well as its role in the diagnosis of leprosy.
Methods
The study was approved by the institutional ethics committee, and each study participant gave written informed consent for inclusion. Thirty consecutive individuals from September 2018, attending the outpatient clinic of the dermatology department of the Government Medical College, Kozhikode diagnosed to have leprosy by the World Health Organization criteria and who had not yet completed the fixed duration treatment were included in the study. Controls of same age and gender as that of cases were selected from amongst the persons with no clinical evidence of leprosy and who accompanied the patients attending the dermatology outpatient clinic. As per the study by Jain et al. the average standard deviation among cases and controls was 11.5mm2 for the ulnar nerve. Hence, to detect a difference of 6 mm2 between affected and normal nerves, the sample size calculated was 60 for each nerve.2 We excluded individuals with history of alcoholism, coexisting diabetes, hypothyroidism, hereditary neuropathies, HIV and trauma-related peripheral nerve disease from both groups. Evaluation for undetected diabetes mellitus (fasting and post prandial blood sugar estimation), hypothyroidism (free T3, T4 and thyroid stimulating hormone), hereditary neuropathies and HIV infection were carried out in study participants when there were symptoms and/or clinical features suggestive of the same.
Each patient was carefully examined for skin lesions (hypopigmented or erythematous patches, plaques, annular lesions, infiltrated plaques, nodules and vague shiny hypopigmented macules) and lesional impairment. of temperature, pain and touch sensation. Both groups underwent a clinical assessment by palpation to document enlarged peripheral nerves. This was done by the second author (dermatologist with more than 10 years of experience in diagnosing and treating leprosy) who was not blinded to the history and clinical details.
Total three hundred nerves (sixty each of ulnar, radial, median, lateral popliteal and posterior tibial nerves) were assessed in 30 cases and 30 healthy age- and sex-matched controls. The nerves were palpated at the same sites in all participants. The ulnar nerve at the elbow, median nerve in the wrist, lateral popliteal nerve behind the head of fibula as it winds round the neck of fibula and posterior tibial nerve behind the medial malleolus were palpated to detect thickening. Radial nerve was assessed in the radial groove in all the study participants. Nerves were clinically graded after palpation as followed.2
Grade 0: Nerve not thicker than the same nerve on the contralateral side.
Grade 1: Nerve thickened more than the same on the contralateral side.
Grade 2: Nerve thickened with a rope-like consistency.
Grade 3: Nerve thickened with a beaded or nodular feel.
We recorded sensory impairment along the course of nerve supply whenever present. Sensory impairment was defined as the inability or reduced ability to appreciate temperature, pain and touch. Temperature sensation was assessed using test tubes containing water at 420C and 250C. Pain sensation was tested using sterile needle prick and cotton wool was used to test fine touch. Sensory nerve function impairment of hands and feet were also assessed by Semmes-Weinstein nylon monofilaments as recommended.6 The power of muscles supplied by the respective nerves was tested and rated as per the Medical Research Council rating scale.7 Sensory and/ or motor function impairment along the course of the nerve supply in a diagnosed case of leprosy was taken as evidence of nerve function impairment.
A nerve conduction study was carried out in doubtful cases to confirm nerve function impairment.
All patients manifesting skin lesions of leprosy were advised to undergo skin smear studies (from ear lobe, representative skin lesion and normal skin) and biopsy (from representative skin lesion). In suspected neuritic leprosy, histopathology analysis was performed on a purely sensory cutaneous nerve, if one was enlarged. In pure neuritic leprosy where a nerve biopsy could not be performed or was inconclusive, other possible neurological causes were ruled out with the help of a neurologist. Based on the clinical findings, the skin smear and the histopathology findings, the cases were categorized along the leprosy spectrum. A preset proforma was used to document the clinical and investigation findings.
Ultrasonography and color Doppler
First author (A physiatrist having 10 years of experience in musculoskeletal ultrasound examination) assessed the aforementioned peripheral nerves, using a linear array transducer with a broadband frequency of 8–18 MHz and color Doppler. A pre-set proforma was used to document the findings. The clinician performing the high resolution ultrasound was blinded to the history and the clinical details of the study participants and was not aware whether the individual was a case or a control.
Radial, ulnar, median and posterior tibial nerves were evaluated with the participants in supine position. For radial nerve examination, the arm was placed with the shoulder adducted and internally rotated, and elbow flexed so that the arm lied on the chest. The probe was applied perpendicular to the long axis of the humerus, midway along its shaft, on the posterolateral surface. The nerve was assessed in the radial groove directly upon the surface of the bone. Ulnar nerve was studied at the medial epicondyle and 4 cm above the medial epicondyle with the arm in abduction and elbow flexed less than 900., Median nerve was assessed at the wrist and 4cm above the wrist. For median nerve examination, the study participant was positioned with the arms by the side and in supination. The tibial nerve was examined with the lower limb in minimal external rotation for easy assessment of the medial aspect of the ankle. The nerve was studied by placing the probe transversely perpendicular to the nerve at 1cm, 3cm and 5cm above and behind the medial malleolus. Lateral popliteal nerve was assessed with the patient in prone position and the knees in full extension. The probe was placed transversely over the fibular head and perpendicular to the nerve. Then the probe was moved proximally to obtain the second measurement above the head of fibula. Measurement at the point of maximum nerve thickness in the visualized segment of the nerve was recorded in each case. For measuring cross sectional area, the ultrasound beam was kept perpendicular to the nerve to minimise anisotropy. Then the trace was taken just inside the hyperechoic border of the epineurium. Positioning of study participants and positioning of limbs of study participants during high resolution ultrasound were kept uniform throughout the study. The mean cross-sectional area and the standard deviation were determined for each nerve in controls. Patients showing a cross-sectional area more than the calculated upper bound of 95% confidence interval for mean for a specific peripheral nerve in controls were considered to have enlargement of that nerve during subsequent analysis.
The echotexture of the nerves was graded as follows: mild abnormality = some hypo-echogenicity, moderate abnormality = obvious hypo-echogenicity and severe abnormality = absence of any fascicular pattern.
Doppler analysis was carried out in the colour box that defined the region of interest. Care was taken to include the area between the skin and the nerve in the Doppler box. The optimal Doppler frequency was determined and a low pulse repetition frequency was used. The correct gain was found by turning the gain up until random noise was heard and lowering till the noise disappeared. The wall filters were kept low. The presence of blood flow signals in the perineural plexus or intrafascicular vessels was considered as evidence of hypervascularity of the nerve.
Data were entered in Microsoft Excel and analyzed with SPSS Inc IBM company version 16 Chicago, SPSS Inc. (United States of America). Agreement between nerve thickening documented by clinical examination and by high-resolution ultrasound was assessed by kappa statistics. The sensitivities of clinical examination and high-resolution ultrasound to detect peripheral nerve thickening were compared by Pearson’s Chi-square test;P < 0.05 was considered significant.
Results
In each group, there were 24 males and six females. Age ranged from 16 to 78 years (mean, 44.4 ± 17.3 years in both cases and controls).
The mean cross-sectional area on high-resolution ultrasound in controls was 6.68 mm2 for the radial nerve, 7.78 mm2 for ulnar, 9.85 mm2 for median [Figure 1], 8.9 mm2 for lateral popliteal and 10.73 mm2 for the posterior tibial nerve.
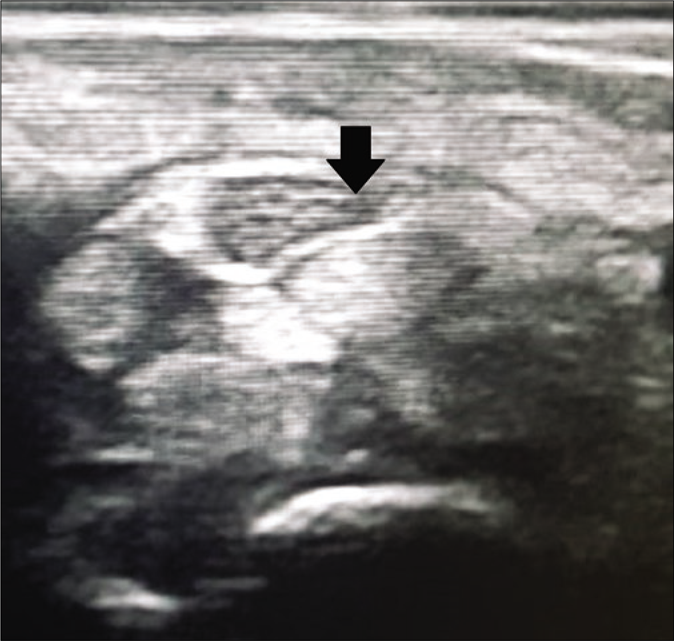
- High resolution ultrasound image (transverse view) of median nerve of a control showing normal thickness and honeycomb fascicular pattern at wrist (black arrow)
There were 21 borderline tuberculoid, 2 borderline lepromatous, 2 lepromatous and 5 pure neuritic leprosy cases. Six patients (20%) required paucibacillary and 24 (80%) needed multibacillary treatment.
Clinical examination identified thickening in 60 nerves (20%). Thirty one out of the sixty (51.7%) had nerve function impairment. None of the patients had an enlarged radial nerve. Among the 60 clinically thickened nerves, 21 (35%) showed grade-2 thickening and 39 (65%) grade 1. None of the patients manifested grade-3 enlargement of nerves.
Seventy (23.3%) of the 300 nerves studied in leprosy cases showed sensory and/or motor function impairment. Fifty nine (19.7%) manifested sensory function impairment, one (0.3%) had motor function impairment and 10 out of the 300 (3.3%) manifested both. Neuritis was diagnosed in eight nerves (2.7%) in three patients who manifested nerve tenderness with or without sudden-onset nerve palsy. Two of them had features of type 1 lepra reaction and the third had features of type 2 lepra reaction. All three patients were receiving 15–30 mg prednisolone daily (for 2-7 weeks) for the neuritis at the time of recruitment to the study.
All 25 patients with skin lesions underwent skin biopsy; clinicohistopathological concordance was noted in all of them. A sensory cutaneous nerve was clinically thickened in three (60%) of the five pure neuritic leprosy cases and two among them consented to a nerve biopsy, where both showed lymphocytic infiltration without definite granuloma formation. A detailed neurology workup favoured a diagnosis of leprosy in all the pure neuritic cases. Nerve conduction study was carried out in all the five pure neuritic cases and four patients with skin lesions. Five patients had reduction in both nerve conduction velocity and amplitude. Isolated reduction in conduction velocity and amplitude were recorded in two patients each. Distal latency was increased in three cases.
Cross-sectional areas of more than 7.1mm2 for the radial nerve, 8.17mm2 for ulnar [Figures 2 and 3], 10.17mm2 for median, 9.50mm2 for lateral popliteal and 11.21mm2 for the posterior tibial nerve [Figures 4 and 5] were considered as nerve thickening on high-resolution ultrasound.
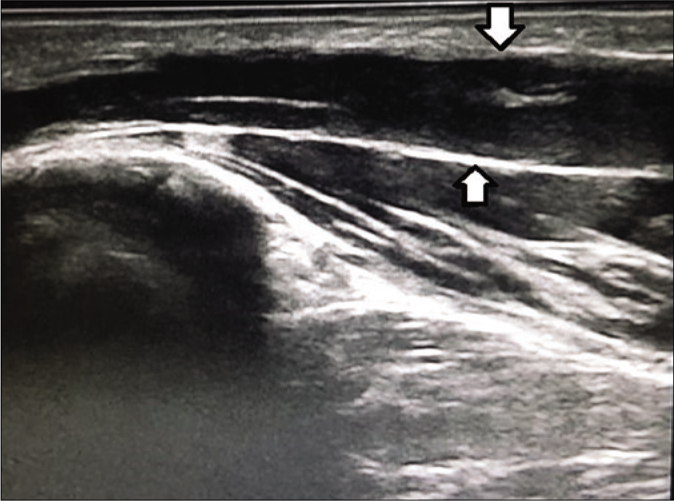
- High resolution ultrasound image (longitudinal view) of ulnar nerve of a leprosy patient showing enlarged nerve (white arrow) at elbow
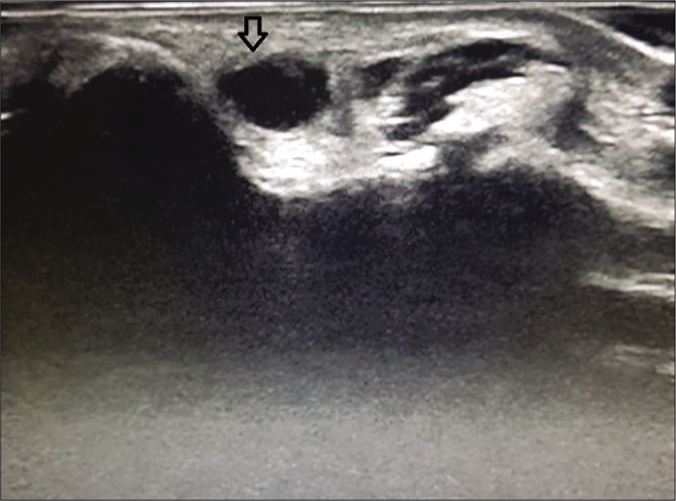
- High resolution ultrasound image (transverse view) of ulnar nerve of a leprosy patient showing thickened and hypoechoeic nerve with loss of fascicular pattern (black arrow) at elbow
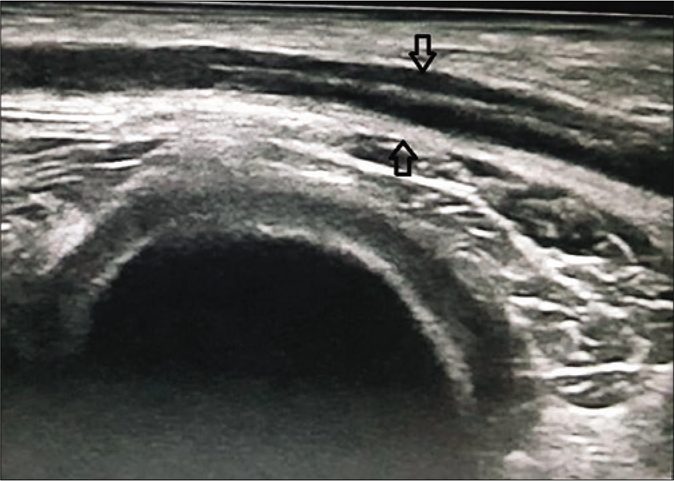
- High resolution ultrasound image (longitudinal view) of posterior tibial nerve of a leprosy patient showing enlarged nerve (black arrow) at medial malleolus
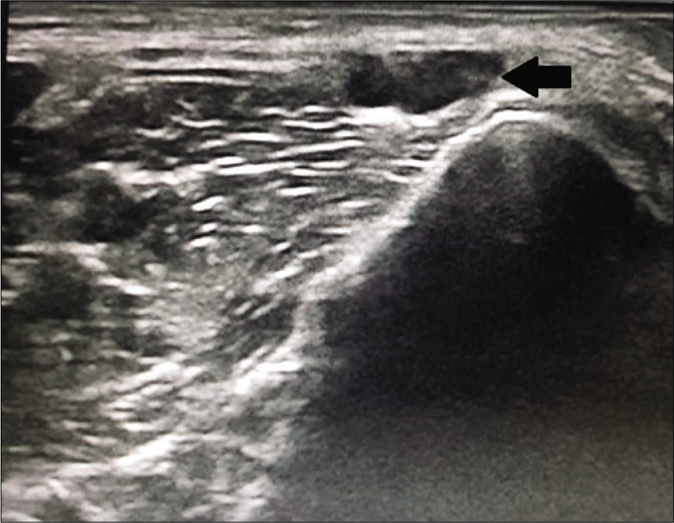
- Hiigh resolution ultrasound image of posterior tibial nerve (transverse view) of a leprosy patient showing enlarged, hypoechoeic nerve with loss of normal honeycomb pattern (black arrow) at medial malleolus
Except for the radial nerve, the other four peripheral nerves evaluated in the leprosy cases showed a statistically significant increase in the mean cross-sectional area in comparison to the healthy controls [Table 1]. Two of the three median nerves found enlarged in cases by clinical examination were detected to be bifid median nerves (physiological variation) on high-resolution ultrasound. None of the bifid median nerves showed impairment of function.
| Mean cross-sectional area on high-resolution ultrasound examination | Study participants | Range (mm2) | Mean±SD (mm2) | P | 95% of CI for mean (mm2) |
|---|---|---|---|---|---|
| Radial nerve | Cases | 3-12 | 6.38±2.195 | 0.395 | 5.82–6.95 |
| Controls | 3-9 | 6.68±1.610 | 6.27–7.10 | ||
| Ulnar nerve | Cases | 4-26 | 10.15±5.118 | 0.001 | 8.83–11.47 |
| Controls | 5-12 | 7.78±1.508 | 7.39–8.17 | ||
| Median nerve | Cases | 4-27 | 11.455±4.2575 | 0.006 | 10.355–12.555 |
| Controls | 7-13 | 9.850±1.2327 | 9.532–10.168 | ||
| Lateral popliteal nerve | Cases | 6-44 | 13.45±7.670 | 0.000 | 11.47–15.43 |
| Controls | 6-20 | 8.90±2.319 | 8.30–9.50 | ||
| Posterior tibial nerve | Cases | 4-35 | 14.82±6.355 | 0.000 | 13.17–16.46 |
| Controls | 4-15 | 10.73±1.831 | 10.26–11.21 |
SD: standard deviation, CI: confidence interval
High-resolution ultrasound found 141 out of the 300 (47%) nerves enlarged in contrast to the 60 (20%) diagnosed clinically in leprosy cases; the difference was statistically significant (P < 0.001). Fifty (35.5%) out of the 141 nerves found thickened by high resolution ultrasound showed nerve function impairment while 31 (51.7%) out of the 60 clinically thickened nerves manifested impairment of function. Agreement between nerve thickening detected clinically and by high-resolution ultrasound in leprosy patients varied from −0.040 for the median nerve to 0.215 for lateral popliteal nerve [Table 2].
| Peripheral nerve | Cross-sectional area within normal limits in high-resolution ultrasound study Not enlarged clinically Enlarged clinically | Cross-sectional area above normal limits in high-resolution ultrasound study Not enlarged clinically Enlarged clinically | Agreement between thickening detected by clinical examination and high-resolution ultrasound study (Kappa statistics) | ||
|---|---|---|---|---|---|
| Ulnar nerve | 21 | 7 | 17 | 15 | 0.214 |
| Median nerve | 25 | 2 | 32 | 1 | −0.040 |
| Lateral popliteal nerve | 18 | 5 | 20 | 17 | 0.215 |
| Posterior tibial nerve | 18 | 3 | 29 | 10 | 0.088 |
The maximum cross-sectional area was recorded at the corresponding ‘entrapment’ site in 206 out of the 240 (85.8%) nerves and above the entrapment site in 34 out of the 240 (14.2%) nerves (The other 60 nerves were radial nerves whose mean cross-sectional area was measured at only one site viz., in the radial groove).
Among the 141 nerves found enlarged by the high-resolution ultrasound study, the thickening extended to involve 4–10 cm length of the nerve in 109 (77.3%), less than 4 cm length of the nerve in 26 (18.4%) and more than 10 cm in six (4.3%).
Among the 300 nerves studied in leprosy cases, 63 (21%) showed a mild echotexture abnormality. Five (1.7%) and seven (2.3%) nerves manifested moderate and severe echotexture abnormalities respectively [Figures 3 and 5]. In controls, out of the 300 nerves evaluated, 26 (8.7%) showed a mild abnormality in the echotexture; moderate and severe abnormalities were noted in none. These 26 nerves included all the 10 peripheral nerves assessed in two controls plus bilateral radial, ulnar and lateral popliteal nerves in one control. All these three controls were aged above 50 years (two males and one female).
None of the study participants (cases or controls) showed signals of increased vascularity on colour Doppler analysis.
Clinical examination diagnosed nerve thickening in 31 (44.3%) out of the 70 nerves that manifested nerve function impairment. High-resolution ultrasound detected thickening in 50 (71.4%) out of the 70 nerves with nerve function impairment [Table 3]. The difference was statistically significant (P = 0.002). Among the 230 nerves that showed no nerve function impairment, clinical evaluation detected thickening in 29 (12.6%) and high-resolution ultrasound in 91 (39.6%). This was again statistically significant (P < 0.001). In other words, high-resolution ultrasound was more sensitive in detecting nerve thickening than clinical examination, irrespective of the presence or absence of nerve function impairment. Clinical examination showed thickening limited to single nerve in two of the six paucibacillary cases while none of the nerves were thickened in the remaining four. High resolution ultrasound diagnosed thickening of multiple nerves in both the patients who recorded single nerve enlargement clinically and in two others who did not manifest thickening of any of the nerves on clinical examination.
| Peripheral nerve | Presence of nerve function impairment | No nerve function impairment | ||
|---|---|---|---|---|
| Clinically diagnosed nerve thickening (figures in bracket are ercentages of nerves with NFI showing nerve thickening clinically) | Nerve thickening by HRUS (figures in brackets are percentages of nerves with NFI showing nerve thickening by HRUS) | Clinically diagnosed nerve thickening (figures in brackets are percentages of nerves without NFI showing nerve thickening clinically) | Nerve thickening by HRUS (figures in brackets are percentages of nerves without NFI showing nerve thickening by HRUS) | |
| Radial nerve | 0 (0) | 0 (0) | 0 (0) | 0 (0) |
| NFI present 0 | ||||
| No NFI-60 | ||||
| Ulnar nerve | 13 (61.9) | 16 (76.2) | 9 (23.1) | 16 (41) |
| NFI present 21 | ||||
| No NFI-39 | ||||
| Median nerve | 0 (0) | 6 (50) | 3 (6.3) | 27 (56.3) |
| NFI present 12 | ||||
| No NFI 48 | ||||
| Lateral popliteal nerve | 13 (52) | 17 (68) | 9 (25.7) | 20 (57.1) |
| NFI present 25 | ||||
| No NFI 35 | ||||
| Posterior tibial nerve | 5 (41.7) | 11 (91.7) | 8 (16.7) | 28 (58.3) |
| NFI plus 12 | ||||
| No NFI 48 | ||||
| Total | 31 (44.3) | 50 (71.4) | 29 (12.6) | 91 (39.6) |
| NFI present 70 | ||||
| No NFI 230 | ||||
HRUS: high-resolution ultrasound, NFI: nerve function impairment
Discussion
Our findings on the mean cross-sectional area of normal peripheral nerves is comparable to those in previous studies. But the mean cross-sectional area of 7.78mm2 documented for the ulnar nerve by us was higher than the 4.1 mm2 reported by some others.2,3,8,9 This may be due to the relatively younger control population in the two previous studies (mean age of 38–39 years in comparison to the mean age of 44 years documented in controls in the current study) and the female predilection among the controls in Gupta et al.’s study.2,8 Bathala et al. have previously observed male sex and advancing age to be associated with a greater cross-sectional area of the ulnar nerve.9 To overcome the age and gender bias in our study, we opted for age- and sex-matched controls.
The statistically significant increases observed in the mean cross-sectional areas of ulnar, median, lateral popliteal and posterior tibial nerves in our leprosy cases is also consistent with previous reports.2,3,4,8 The maximum site of the cross-sectional area being above the entrapment sites in more than 10% of nerves in the leprosy cases and nerve enlargement extending to involve variable lengths of the nerves as observed by us has been reported previously as well.2 Previous reports noted thickening extending about 22cm length of median and ulnar nerves whereas the maximum length affected was 14 cm (ulnar nerve) in the current study.2
The lack of good agreement on kappa statistics between the clinically diagnosed and the high-resolution ultrasound detected nerve thickening (the latter detecting more numbers) indicates the inadequacy of clinical evaluation in the detection of nerve enlargement in leprosy. This has also been noted by Jain et al., though they reported somewhat greater agreement between the clinical and high-resolution ultrasound findings than in our study.2
High-resolution ultrasound identified nerve enlargement even when there was no evident nerve function impairment in our patients. In our experience, in a suspected case of leprosy, the clinician is more likely to diagnose nerve thickening in the presence of nerve function impairment than in its absence. Our findings indicate that high-resolution ultrasound may be a more objective tool for assessment of peripheral nerve involvement in leprosy.
Though it was limited to a few patients, moderate and severe echotexture abnormalities may assume significance since these findings were not seen in any of the controls. We suggest more studies to confirm whether this could be a specific high-resolution ultrasound finding diagnostic of nerve involvement in leprosy. The mild echotexture abnormalities observed in three controls may possibly be due to age-related changes since all the three were above 50 years and the same feature was documented in 26 out of the 30 (86.7%) nerves evaluated in them.10
None of our patients manifesting increased vascularity in the Doppler study was discordant with previous studies.2,3,4,8,11 However this finding was more frequently reported in lepra reactions and the three lepra reaction cases in our study already being on treatment with systemic steroids could be the reason for this difference.2
The clinical evaluation failing to detect nerve thickening in any of the patients manifesting sensory or motor deficit of the median nerve was expected considering the anatomic location of this particular nerve.2 Conversely, two of the three median nerves diagnosed to have thickening on clinical evaluation being bifid median nerves shows the possible misdiagnoses that may occur (in the setting of physiological variations) by relying on clinical examination and supports the role of high-resolution ultrasound in leprosy.
The greater sensitivity of high-resolution ultrasound in comparison to the clinical examination to detect nerve thickening becomes more significant in the setting of nerve function impairment, since one of the cardinal criteria to diagnose leprosy remains the enlargement of peripheral nerves with nerve function impairment along the supply of those nerves. By defining the diagnostic parameters for peripheral nerve involvement on high-resolution ultrasound, we might improve the sensitivity of this criterion to diagnose leprosy.
We did not attempt to determine the specificity and the positive predictive value of clinical evaluation and high-resolution ultrasound to diagnose peripheral nerve involvement since the absence of nerve function impairment does not rule out leprous neuropathy, and nerve function impairment may succeed nerve thickening in the course of the disease. Nerve biopsy which could have confirmed the involvement of individual nerves was not feasible since all the major nerve trunks affected by the disease are mixed nerves with prominent motor function.
Limitations
The single-center study design was the major study limitation. Further, the cross-sectional area recorded by us may not apply to people from different geographic areas. The other limitations were observer bias in clinical and ultrasound measurements (since there was only one observer each for clinical and high resolution ultrasound evaluation), not blinding the clinician assessing the nerve thickening, the inadequacy of sample size to determine the normal high resolution ultrasound parameters in a population, not carrying out nerve conduction studies in all the participants and not having information on the effect of antileprosy treatment and systemic steroids on ultrasound findings.
Conclusion
This study, though suggesting the importance of high-resolution ultrasound in the diagnosis of leprosy, needs to be replicated in a larger number of cases in different spectra of the disease from various parts of the world.
More studies to confirm our findings may improve the diagnostic efficacy of high-resolution ultrasound in identifying leprous neuropathy.
Acknowledgments
The authors express sincere gratitude to Dr. MP Binitha, Professor and Former Head, Department of Dermatology and Venereology, Government Medical College, Kozhikode for her invaluable suggestions in manuscript preparation.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
None.
Conflicts of interest
There are no conflicts of interest.
References
- Guidelines for the Diagnosis. Treatment and Prevention of Leprosy, Executive Summary. Available from: http://www.searo.who.int/entity/global_leprosy_programme/approvedguidelinesleprosyexecutivessummary.pdf?ua=1 [Last accessed on 2019 Jun 19]
- [Google Scholar]
- High resolution sonography: A new technique to detect nerve damage in leprosy. PLoS Negl Trop Dis. 2009;3:e498.
- [CrossRef] [PubMed] [Google Scholar]
- Role of ulnar nerve sonography in leprosy neuropathy with electrophysiologic correlation. J Ultrasound Med. 2009;28:1201-9.
- [CrossRef] [PubMed] [Google Scholar]
- Evaluation of peripheral nerve lesions with high resolution ultrasonography and color Doppler. Neurol India. 2016;64:1002-9.
- [CrossRef] [PubMed] [Google Scholar]
- Echotexture of peripheral nerves: Correlation between US and histologic findings and criteria to differentiate tendons. Radiology. 1995;197:291-6.
- [CrossRef] [PubMed] [Google Scholar]
- Neuritis: Definition, Clinicopathological manifestations and proforma to record nerve impairment in leprosy In: Kumar B, Kar H K, eds. IAL Textbook of Leprosy Vol 28. (2nd Edition). New Delhi: Jaypee Publisher; 2016. p. :397-415.
- [CrossRef] [Google Scholar]
- Protocol for motor function assessment in leprosy and related research questions. Indian J Lepr. 2001;73:145-58.
- [Google Scholar]
- High resolution sonographic examination: A newer technique to study ulnar nerve neuropathy in leprosy. Lepr Rev. 2016;87:464-75.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasonographic cross sectional area normal values of the ulnar nerve along its course in the arm with electrophysiological correlations in 100 Asian subjects. Muscle Nerve. 2013;47:673-6.
- [CrossRef] [PubMed] [Google Scholar]
- Age related differences in the quantitative echotexture of median nerve. J Ultrasound Med. 2015;34:797-804.
- [CrossRef] [PubMed] [Google Scholar]
- Ultrasonography of leprosy neuropathy: A longitudinal prospective study. PLoS Negl Trop Dis. 2016;10:e0005111.
- [CrossRef] [PubMed] [Google Scholar]






