Translate this page into:
Hodgkin's lymphoma arising in a case of mycosis fungoides: An unusual association
2 Department of Dermatology, Venereology and Leprosy, Dr. Ram Manohar Lohia Hospital, Post Graduate Institute of Medical Education and Research, New Delhi, India
Correspondence Address:
Surbhi Goyal
Department of Pathology, Vardhman Mahavir Medical College, Safdarjung Hospital, New Delhi - 110 029
India
| How to cite this article: Sharma P, Goyal S, Yadav AK, Singh J, Mandal AK. Hodgkin's lymphoma arising in a case of mycosis fungoides: An unusual association. Indian J Dermatol Venereol Leprol 2018;84:292-297 |
Abstract
Mycosis fungoides is a cutaneous T-cell lymphoma with a high risk for developing secondary malignancies, especially B-cell lymphoproliferative disorders. About 40 cases of Hodgkin's lymphoma associated with mycosis fungoides have been reported in literature till date. We report a case of a 35-year-old gentleman who presented with intensely itchy reddish lesions all over the body. Multiple skin biopsies taken from the lesions on scalp and back confirmed the clinical diagnosis of mycosis fungoides. While on treatment, he presented with multiple bilateral cervical, axillary and inguinal lymphadenopathy 9 years after the primary diagnosis of mycosis fungoides. Excision biopsy of a cervical lymph node revealed partial effacement of architecture by a tumor comprising polymorphous background. Histopathology and immunohistochemistry revealed a diagnosis of Hodgkin's lymphoma - nodular sclerosis subtype. The patient was started on chemotherapy for stage IV Hodgkin's lymphoma. Our case emphasizes the importance of keeping secondary Hodgkin's lymphoma in mind while dealing with a patient of mycosis fungoides. Our case immunohistochemically supports the distinct etiopathogenesis of Epstein–Barr virus-negative Hodgkin's lymphoma vis-à-vis cutaneous mycosis fungoides.
Introduction
Mycosis fungoides is a rare, extranodal cutaneous T-cell lymphoma accounting for 2% of non-Hodgkin lymphomas. It has an annual incidence of 0.3–1 per 1 lakh.[1],[2] It typically begins as slowly progressive dermatitis-like patches and plaques which if untreated evolves to nodules and eventual systemic dissemination.
Patients with mycosis fungoides are at a higher risk for developing secondary malignancies, especially melanoma and B-cell non-Hodgkin lymphomas.[3] Secondary Hodgkin's lymphomas in this cutaneous lymphoma are rather uncommon and infrequently reported. This association was first described in 1963, and only 40 cases have been reported in literature since then;[4] of these, nodular sclerosis Hodgkin's lymphoma is the most frequently reported variant.[5]
We hereby report an unusual case of Hodgkin's lymphoma arising in a patient of mycosis fungoides 9 years after the primary diagnosis.
Case Report
A 35-year-old gentleman was on irregular medication for mycosis fungoides (stage IB) for the past 7 years. He presented to the outpatient department of Safdarjung Hospital in New Delhi with multiple bilateral cervical, axillary and inguinal lymph nodes varying in size from 0.5 to 2 cm in diameter. Cutaneous examination revealed multiple nodules on the scalp coalescing to form a plaque measuring 5 cm × 4 cm [Figure - 1]a. The dorsal aspect of both the hands showed ill-defined hyperpigmented atrophic plaques. Palms were edematous and shiny [Figure - 1]b. Similar lesions were seen on the anterior aspect of both the legs [Figure - 1]c and back. A clinical diagnosis of mycosis fungoides with alopecia mucinosa was made. All routine laboratory investigations, peripheral smear, buffy coat examination and bone marrow studies were within normal limits. Computed tomography of the abdomen and chest showed bilateral enlarged cervical, parotid, axillary and inguinofemoral lymph nodes [Figure - 2]a,[Figure - 2]b,[Figure - 2]c,[Figure - 2]d] with mild hepatosplenomegaly. Excision biopsy of the largest upper cervical lymph node was performed. Hematoxylin and eosin-stained sections showed partial effacement of lymph node architecture [Figure - 3]a by a tumor comprising ill-formed nodules separated by thin fibrous septa. A polymorphous population comprising lymphocytes, plasma cells, histiocytes and numerous eosinophils was seen in the background [Figure - 3]b. Admixed within these were large atypical classical [Figure - 3]c, mononuclear as well as lacunar variants of Reed–Sternberg cells [Figure - 3]d. On immunohistochemistry, Reed–Sternberg cells were positive for CD15 [Figure - 4]a, CD30 [Figure - 4]b and CD20 [Figure - 4]c and negative for CD3 [Figure - 4]d, CD19 and epithelial membrane antigen. Immunohistochemical markers for Epstein–Barr virus (Epstein–Barr virus-encoded RNA-1 and latent membrane protein 1) were negative. Thus, the final diagnosis of classical Hodgkin's lymphoma, nodular sclerosis subtype arising in a patient of mycosis fungoides, was rendered.
 |
| Figure 1: |
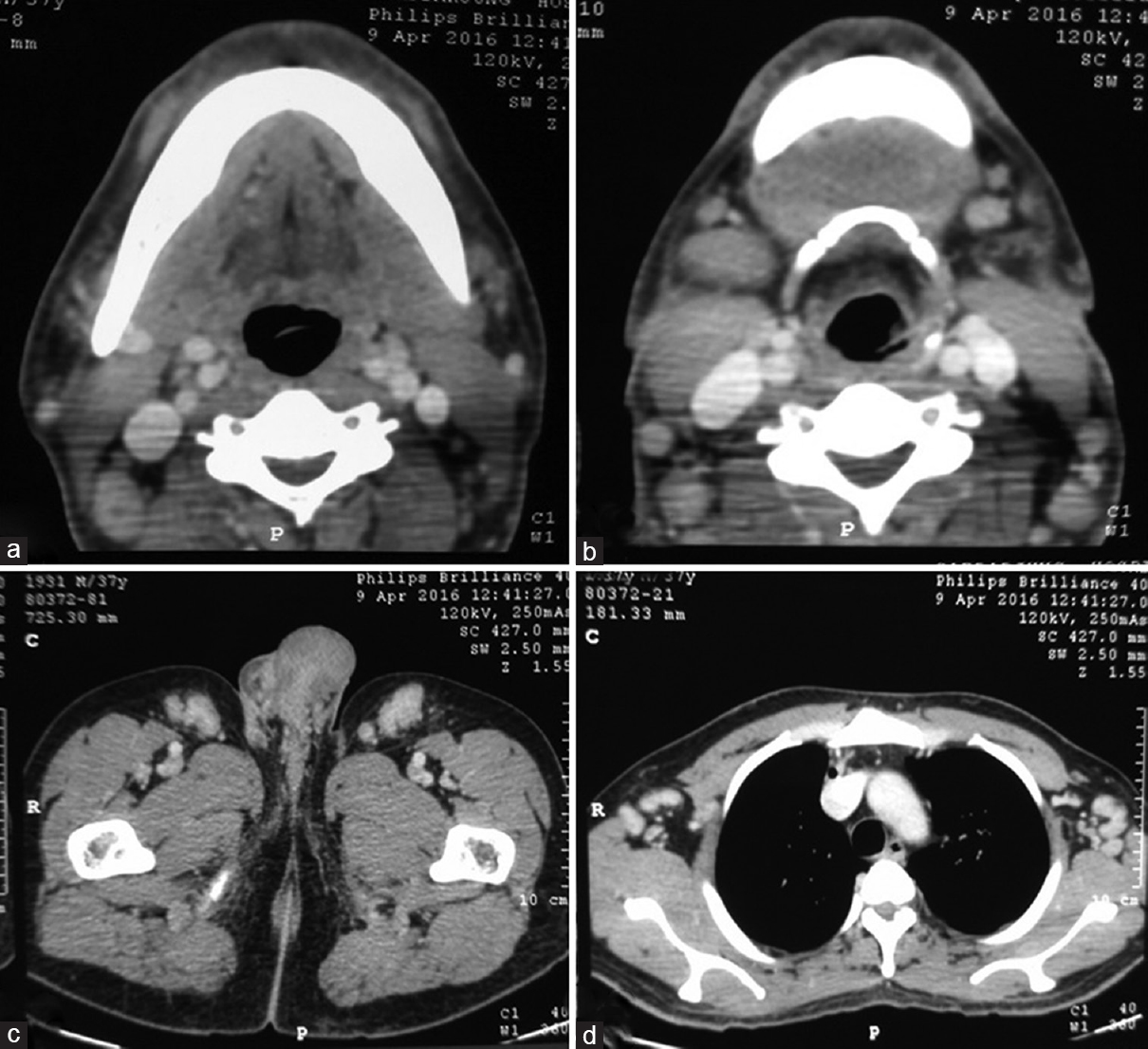 |
| Figure 2: (a) Axial contrast-enhanced computed tomography shows homogeneously enlarged right level 2 lymph nodes. (b) Axial contrast-enhanced computed tomography images of the neck showing multiple enlarged homogeneously enhancing lymph nodes in bilateral submandibular and posterior triangle regions. No necrosis/calcification/periadenitis is seen. (c) Axial contrast-enhanced computed tomography image of the thigh showing multiple enlarged homogeneously enhancing lymph nodes in inguinal region. No necrosis/calcification/periadenitis is seen. (d) Axial contrast-enhanced computed tomography image of the chest showing multiple enlarged homogeneously enhancing lymph nodes in axillary region. No necrosis/calcification/periadenitis is seen |
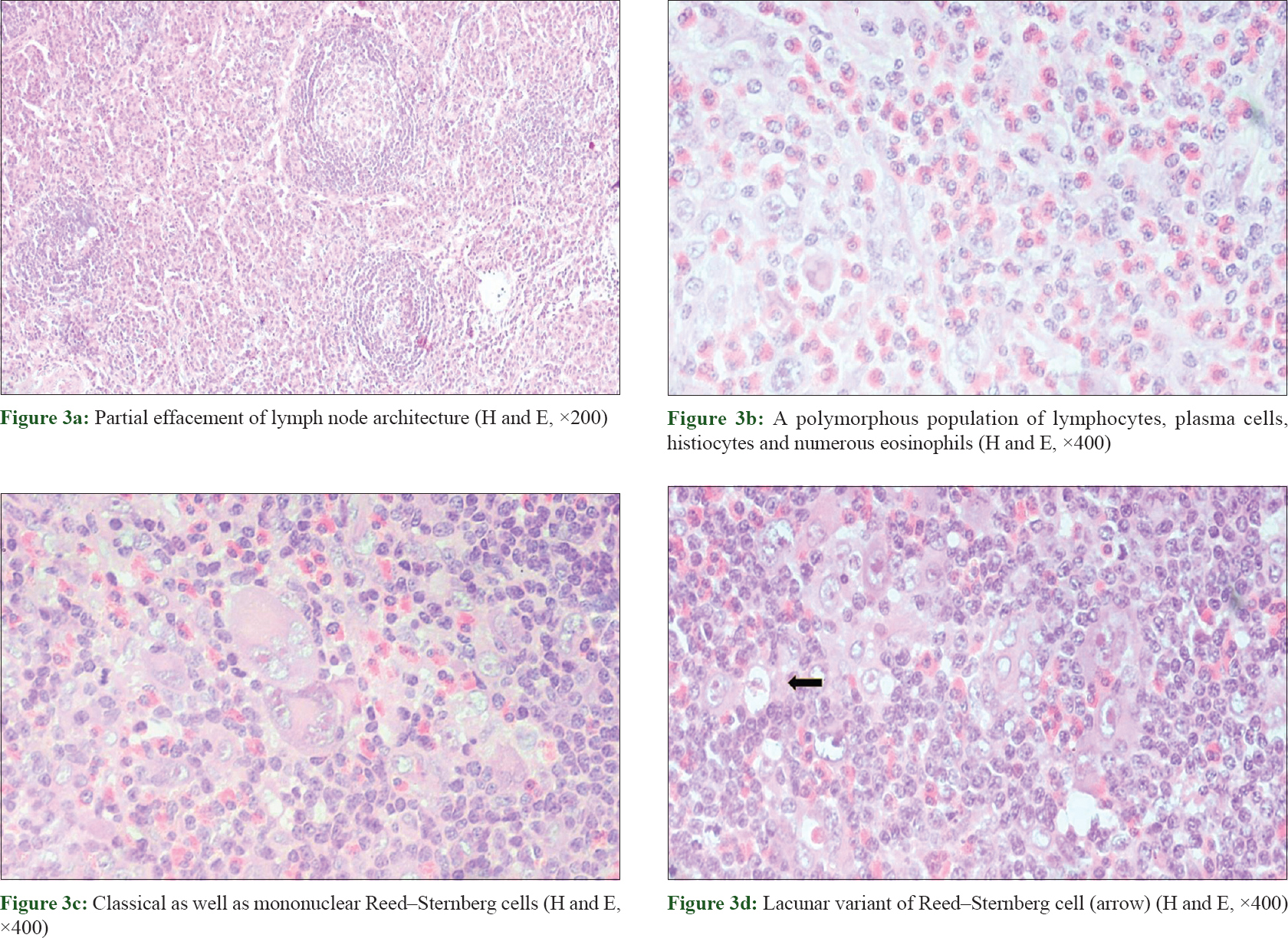 |
| Figure 3: |
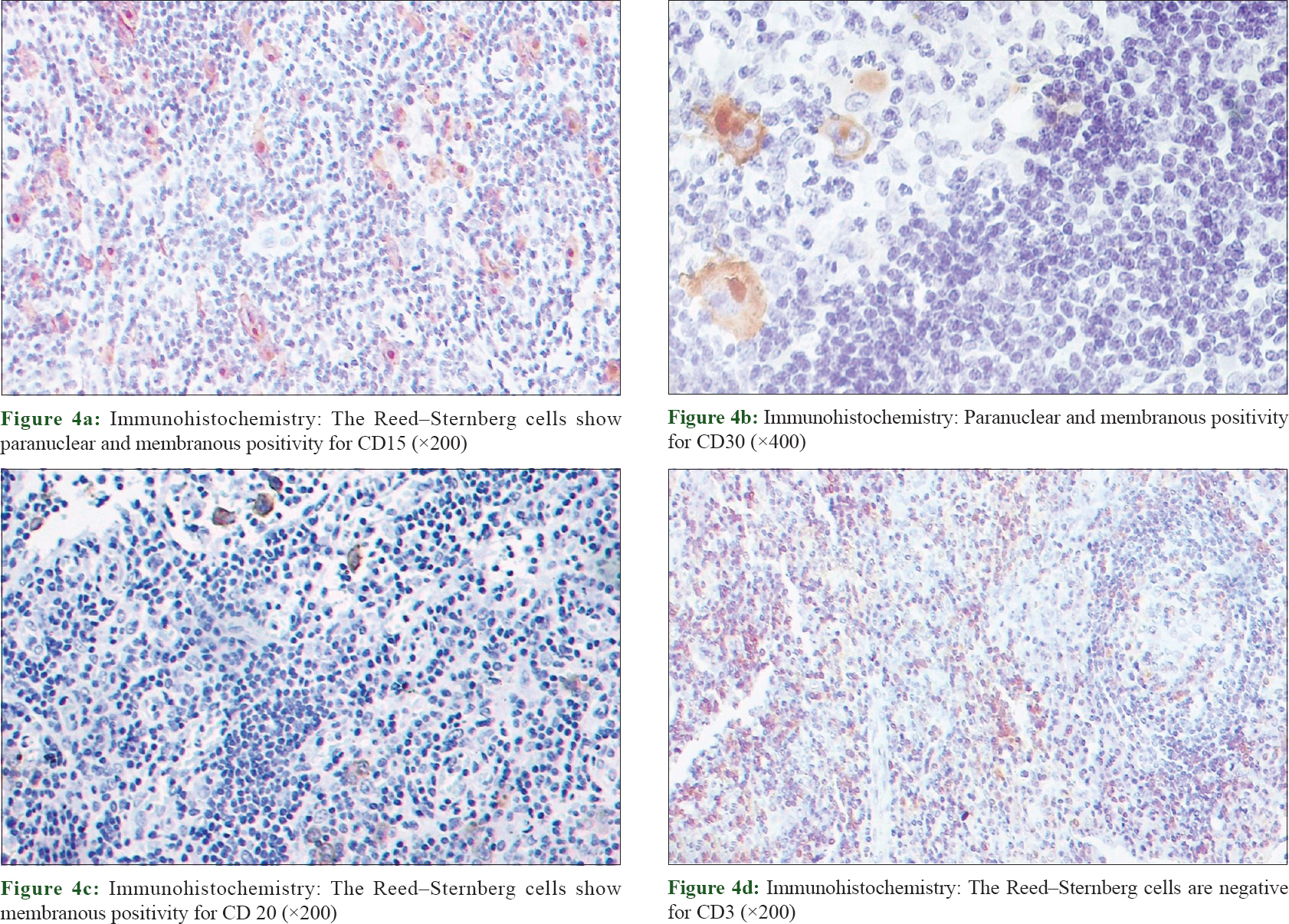 |
| Figure 4 |
The previous skin biopsies taken from the lesions on scalp and back were also reviewed. Hematoxylin and eosin sections showed a band-like monomorphic lymphoid infiltrate at the dermoepidermal junction showing epidermotropism [Figure - 5]a. Some loose collections of lymphoid cells were seen in the stratum spinosum. Papillary dermis showed edema as well as sclerosis [Figure - 5]b. Tumor cells were seen infiltrating into the reticular dermis and subcutaneous fat [Figure - 5]c. The individual cells were small to medium sized, had scant eosinophilic cytoplasm and hyperchromatic nucleus with nuclear irregularity and grooving [Figure - 5]d. No eosinophils or plasma cells were noted. On immunohistochemistry, these tumor cells were positive for leukocyte common antigen, CD3 and CD4. The histomorphological findings were consistent with the clinical diagnosis of mycosis fungoides.
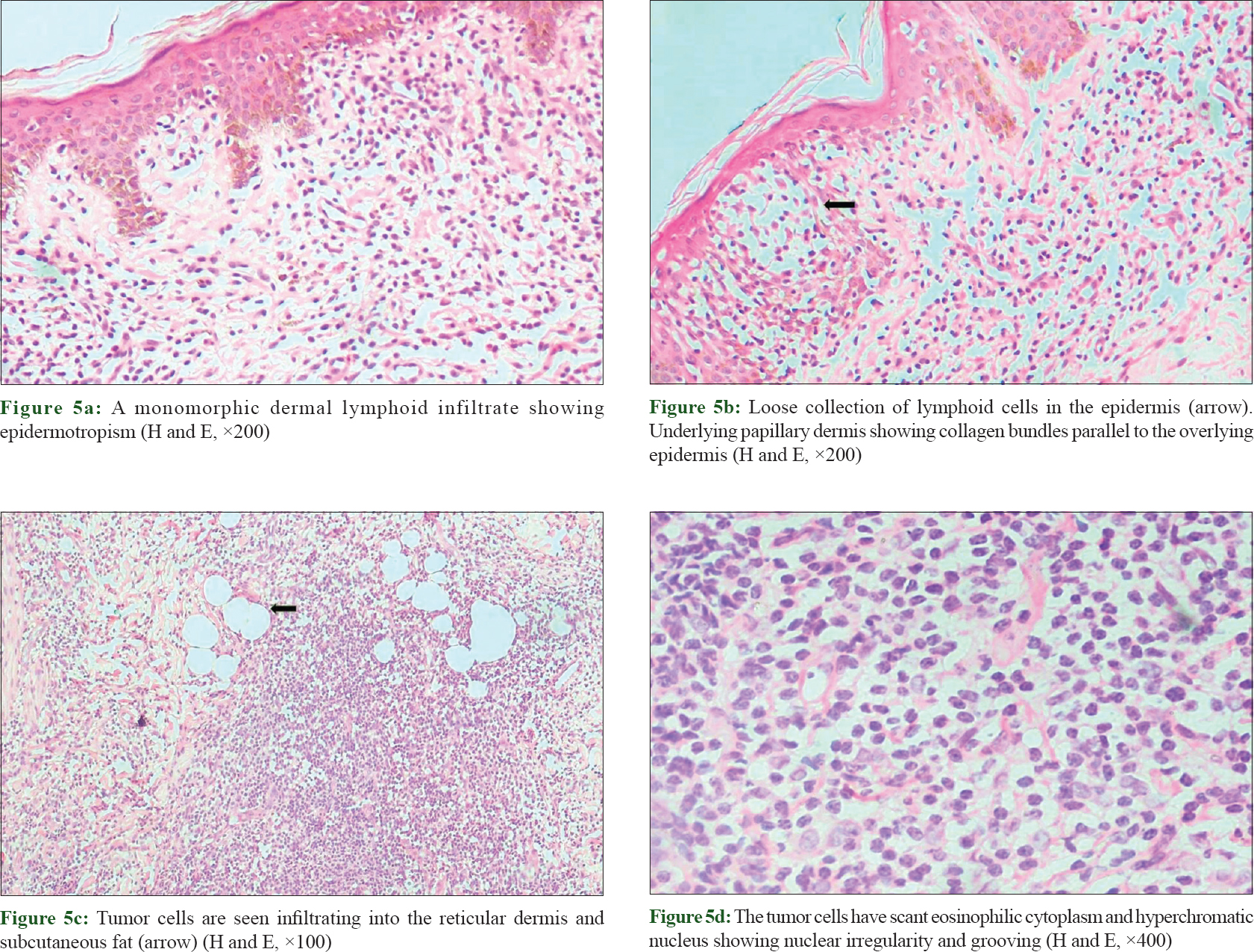 |
| Figure 5 |
The patient was on oral and topical corticosteroids along with low-dose methotrexate for 7 years. There was only slight improvement in the skin lesions along with further development of hair loss as the patient was noncompliant. Following the final diagnosis of classical Hodgkin's lymphoma - nodular sclerosis subtype, arising in the setting of mycosis fungoides, the patient was started on a cyclophosphamide-hydroxydaunorubicin-vincristine -prednisolone regimen and is currently on follow-up.
Discussion
Coexisting lymphomas in the same patient are classified by the working formulation of non-Hodgkin's lymphoma as discordant, composite and secondary lymphomas.[6] Discordant lymphomas are two simultaneously occurring, histologically distinct lymphomas at two different anatomic sites. Two types of lymphoma arising within the same anatomic site are termed as composite lymphomas. Our case belongs to the third category of secondary lymphoma, in which the patient developed Hodgkin's lymphomas, 9 years after the diagnosis of mycosis fungoides.
One should keep in mind the spectrum of diseases while dealing with lymphadenopathy in a patient of mycosis fungoides. These include more common entities such as reactive hyperplasia, dermatopathic lymphadenopathy, opportunistic infections such as tuberculous lymphadenitis and neoplastic causes such as nodal involvement by mycosis fungoides, coexisting non-Hodgkin's lymphoma or rarely Hodgkin's lymphomas.
Various hypotheses have been postulated in literature for the uncommon association of mycosis fungoides and Hodgkin's lymphoma. Apart from genetic factors, the use of immunosuppressants in the treatment of this cutaneous lymphoma and role of Epstein–Barr virus have also been implicated in the development of B-cell lymphoproliferative disorders in these patients.[7] In contrast to previous reports, these two malignancies have now been proved to be distinct. Reed–Sternberg-like cells observed in the transformation of mycosis fungoides are distinct from those seen in Hodgkin's lymphoma as the former retains the expression of T-cell markers. In our patient, there were two distinct lymphomas of different lineages, i.e., T-cell and B-cell in the skin and lymph node, respectively. Further, the frequent association of Epstein–Barr virus-negative Hodgkin's lymphoma and mycosis fungoides suggests a distinct etiopathogenesis.[8],[9]
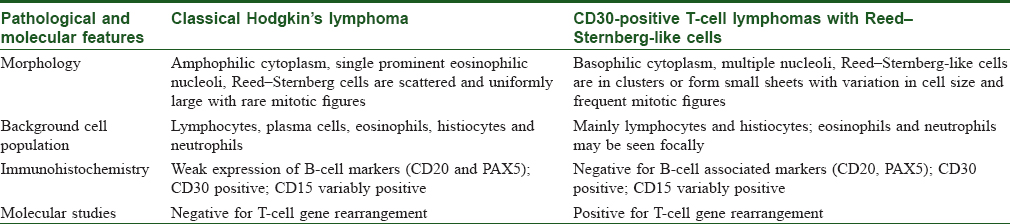
Reports of CD30 transformation of mycosis fungoides mimicking classical Hodgkin's lymphoma are on record. In such cases, CD15 and CD30 immunohistochemistry is not reliable and further testing such as T-cell rearrangement studies and T-cell clonality is needed to differentiate these close mimickers [Table - 1]. A CD30-positive, CD15-positive immunophenotype was earlier regarded as highly specific for Hodgkin's lymphomas. However, recent studies have shown similar immunoreactivity in T-cell lymphomas.[10] Thus, the absence of PAX5 immunostaining and molecular studies helps to confirm the T-cell lineage. Surprisingly, PAX5 positivity has been reported in rare cases of T-cell lymphomas further adding to the ambiguity in the diagnostic methodology. In our case, immunoreactivity of Reed–Sternberg cells for CD20 established the B-cell origin. However, a limiting factor was lack of confirmatory studies such as T-cell gene rearrangement testing.
Due to rarity of this association and paucity of case series with long-term follow-up, clinical outcome in such patients cannot be conclusively predicted. According to previous data, prognosis in these patients is not worse vis-à-vis malignancy alone. However, old age and a subdiaphragmatic disease, as in our case, carry a poorer prognosis.[5]
To conclude, it is important for the clinicians as well as the pathologists to keep in mind the occurrence of secondary lymphomas such as Hodgkin's lymphomas in patients of mycosis fungoides. Our case further supports the hypothesis of cutaneous mycosis fungoides and Hodgkin's disease as two distinct entities.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Willemze R, Jaffe ES, Burg G, Cerroni L, Berti E, Swerdlow SH, et al. WHO-EORTC classification for cutaneous lymphomas. Blood 2005;105:3768-85.
[Google Scholar]
|
| 2. |
Bradford PT, Devesa SS, Anderson WF, Toro JR. Cutaneous lymphoma incidence patterns in the United States: A population-based study of 3884 cases. Blood 2009;113:5064-73.
[Google Scholar]
|
| 3. |
Smoller BR. Risk of secondary cutaneous malignancies in patients with long-standing mycosis fungoides. J Am Acad Dermatol 1994;31(2 Pt 1):295.
[Google Scholar]
|
| 4. |
Block JB, Edgcomb J, Eisen A, Van Scott EJ. Mycosis fungoides. Natural history and aspects of its relationship to other malignant lymphomas. Am J Med 1963;34:228-35.
[Google Scholar]
|
| 5. |
Bee CS, Blaise YP, Dunphy CH. Composite lymphoma of Hodgkin lymphoma and mycosis fungoides: Previously undescribed in the same extracutaneous site. Leuk Lymphoma 2001;42:543-9.
[Google Scholar]
|
| 6. |
Maughan C, Boudreaux L, Lear W, Bohlke A. Discordant mycosis fungoides and cutaneous B-cell lymphoma: A case report and review of the literature. JAAD Case Rep 2015;1:219-21.
[Google Scholar]
|
| 7. |
Ohshima K, Kikuchi M, Yoshida T, Masuda Y, Kimura N. Lymph nodes in incipient adult T-cell leukemia-lymphoma with Hodgkin's disease-like histologic features. Cancer 1991;67:1622-8.
[Google Scholar]
|
| 8. |
Brousset P, Lamant L, Viraben R, Schlaifer D, Gorguet B, Duhault P, et al. Hodgkin's disease following mycosis fungoides: Phenotypic and molecular evidence for different tumour cell clones. J Clin Pathol 1996;49:504-7.
[Google Scholar]
|
| 9. |
Levi E, Kourea HP, Butmarc J, Kadin ME. Low frequency of Epstein-Barr virus in Reed-Sternberg cells of Hodgkin's disease associated with cutaneous T-cell lymphomas. Mod Pathol 1998;11:135.
[Google Scholar]
|
| 10. |
Eberle FC, Song JY, Xi L, Raffeld M, Harris NL, Wilson WH, et al. Nodal involvement by cutaneous CD30-positive T-cell lymphoma mimicking classical Hodgkin lymphoma. Am J Surg Pathol 2012;36:716-25.
[Google Scholar]
|
Fulltext Views
4,407
PDF downloads
2,888





