Translate this page into:
Ichthyosis follicularis, atrichia and photophobia (IFAP) syndrome affecting two successive generations in an Indian family
2 Department of Dermatology, Medical College and Hospital, Kolkata, West Bengal, India
3 Department of Pediatrics, ESI-PGIMSR and ESIC Medical College, Kolkata, West Bengal, India
Correspondence Address:
Niharika Ranjan Lal
32, Prince Rahimuddin Lane, Tollygunge, Kolkata - 700 033, West Bengal
India
| How to cite this article: Lal NR, Bandyopadhyay D, Misra S, Sarkar AK, Rao S. Ichthyosis follicularis, atrichia and photophobia (IFAP) syndrome affecting two successive generations in an Indian family. Indian J Dermatol Venereol Leprol 2016;82:537-539 |
Sir,
The association of ichthyosis follicularis, atrichia and photophobia (IFAP) was first reported as a syndrome by MacLeod in 1909 in three boys.[1] Around 40 patients have been reported since then, some with additional features such as short stature, intellectual disability and seizures.[2] Affected or carrier females may display some of the clinical features such as cutaneous hyperkeratotic lesions along Blaschko's lines, asymmetric distribution of body hair and/or patchy alopecia.[2] We were able to find only a few previous reports of sporadic cases from India. Rai and Shenoi reported a case associated with palmoplantar keratoderma while Laway et al. reported it in association with rickets.[3],[4]
A 12-year-old boy, born of non-consanguineous parentage, presented with complaints of dry and rough skin, alopecia and photophobia since birth [Figure - 1]. There was no history of collodion membrane, hearing deficit, ectropion or eclabium. His intellect, growth and developmental milestones were normal. There was a history of persistent running nose and lacrimation since birth. A history of generalized tonic-clonic seizures was present. The seizures occurred 2 to 3 times a year.
 |
| Figure 1: Index case showing the absence of scalp hair, eyebrows and eyelashes. Note the closure of eyes due to intolerance to light |
Dry skin, photophobia and hair loss was noted in his 2-month-old younger brother and 21-year-old maternal uncle [Figure - 2] and [Figure - 3], respectively]. A family history of atopy was present: his mother had allergic rhinitis and dry skin while his maternal grandmother had dry skin alone.
 |
| Figure 2: Two-month-old younger brother with absent scalp hair, eyelashes and eyebrows |
 |
| Figure 3: Universal alopecia, photophobia and dry skin in index case and his maternal uncle (left) |
Cutaneous examination revealed dry and rough skin with thorn-like follicular papules on the body. There were no scars around the follicles. No hair growth was noted anywhere on the cutaneous surface. Erythematous and eczematous plaques were present in the cubital fossae. Some nails were dystrophic showing onycholysis and trachyonychia. Palms, soles and oral mucosa were normal. There was no cryptorchidism, skeletal deformity or dental abnormalities. Conjunctival and corneal xerosis was noted. Due to extensive photophobia, slit lamp examination and fundoscopy could not be performed to rule out other eye manifestations.
Routine hematological and biochemical investigations were within normal limits. A skin biopsy from a spiny follicular papule revealed hyperkeratotic epidermis, prominent follicular plugging and absence of follicles and sweat glands in the dermis [Figure - 4]. Based on the history and clinical examination, a diagnosis of ichthyosis follicularis with alopecia and photophobia (IFAP) syndrome was made.
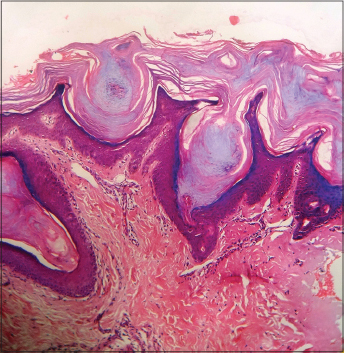 |
| Figure 4: Histopathology showing hyperkeratosis, prominent follicular plugging and absence of hair follicles and sweat glands in dermis (H and E, ×100) |
Ichthyosis follicularis, atrichia and photophobia syndrome is a distinct ichthyosiform disorder defined by the presence of ichthyosis follicularis, atrichia and photophobia having an X-linked recessive mode of inheritance.[2] It results from missense mutations in the membrane-bound transcription factor protease site 2 gene, resulting in impaired cholesterol homeostasis and the ability to cope with endoplasmic reticulum stress.[2]
Ichthyosis and alopecia may be seen in many other conditions such as keratitis-ichthyosis-deafness (KID) syndrome, keratosis follicularis spinulosa decalvans, congenital atrichia with papules and vitamin D resistant rickets. Features that helped to differentiate ichthyosis follicularis, atrichia and photophobia syndrome from keratitis-ichthyosis-deafness syndrome were the absence of hyperkeratotic plaques on an erythematous base (there is erythrokeratoderma rather than ichthyosis in keratitis-ichthyosis-deafness syndrome) and the absence of congenital hearing loss. In addition, the mode of inheritance is autosomal dominant.[5] Keratosis follicularis spinulosa decalvans also shares many features with ichthyosis follicularis, atrichia and photophobia such as follicular hyperkeratosis, alopecia and photophobia. However, alopecia is not congenital and is progressively scarring.[2] Congenital atrichia with papules is characterized by the presence of smooth, skin-colored papules and dermal cysts containing keratinous material.[6] Vitamin D resistant rickets was excluded by the absence of skeletal deformities, normal calcium, phosphate and alkaline phosphatase levels.[7]
The clinical features in our patient that were consistent with ichthyosis follicularis, atrichia and photophobia syndrome were spiny follicular projections typically described as “prickly surface of rose leaf” (ichthyosis follicularis), congenital alopecia, photophobia, dystrophic nails, atopic rhinitis, recurrent chest infections and history of seizures. Genetic studies could not be performed owing to lack of facilities and financial constraints.
Photophobia can present early in life or later in childhood. Superficial corneal ulceration and vascularization may lead to progressive corneal scarring and photophobia. Atopic keratoconjunctival inflammation, chronic tearing, cataract, horizontal nystagmus, astigmatism and myopia have been reported as well.[8] The most frequent neurological features are intellectual disability and seizures.[2] Other clinical features reported with this syndrome are short stature, dysmorphic features such as frontal bossing, choanal atresia and large ears. Various intestinal anomalies, renal, cardiac, vertebral anomalies and cleft hands have been reported.[9] Recurrent infections are often noted.
We found only a few previous reports of familial cases of this syndrome. The largest kindred till date has been reported by Ming et al. in an Australian family.[10] Oeffner et al. have reported three families, while Tang et al. have reported it in five generations in a Chinese family.[11],[12] We were unable to find any reports on familial cases from India.
We managed the patient with emollients and keratolytics and oral isotretinoin in a dose of 0.5 mg/kg. After 3 months of therapy, near complete resolution of the cutaneous lesions was seen. Life expectancy in patients can vary from normal survival to death in the neonatal period from cardiopulmonary complications.[2]
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
MacLeod JM. Three Cases of ichthyosis follicularis associated with baldness.Br J Dermatol 1909;21:165-89.
[Google Scholar]
|
| 2. |
Mégarbané H, Mégarbané A. Ichthyosis follicularis, alopecia, and photophobia (IFAP) syndrome. Orphanet J Rare Dis 2011;6:29.
[Google Scholar]
|
| 3. |
Rai VM, Shenoi SD. Ichthyosis follicularis with congenital atrichia, nail dystrophy and palmoplantar keratoderma. Variant of IFAP syndrome or a new entity? Dermatol Online J 2005;11:36.
[Google Scholar]
|
| 4. |
Laway BA, Verma SK, Bashir MI, Ganie MA, Mir SA, Ahmad SM, et al. IFAP syndrome with rickets and normal Vitamin D status. Indian J Dermatol 2012;57:161-3.
[Google Scholar]
|
| 5. |
Araújo C, Gonçalves-Rocha M, Resende C, Vieira AP, Brito C. A Case of IFAP Syndrome with Severe Atopic Dermatitis. Case Rep Med 2015;2015:450937.
[Google Scholar]
|
| 6. |
Verma R, Vasudevan B, Pragasam V, Badad A, Neema S. Congenital atrichia with papular lesions. Indian J Paediatr Dermatol 2014;15:94-5.
[Google Scholar]
|
| 7. |
Hypocalcemic Vitamin D – Resistant Rickets. Available from: http://www.orpha.net/consor4.01/www/cgi-bin/OC_Exp.php?lng=EN&Expert=93160. [Last accessed on 2015 Jun 27].
[Google Scholar]
|
| 8. |
Traboulsi E, Waked N, Mégarbané H, Mégarbané A. Ocular findings in ichthyosis follicularis-alopecia-photophobia IFAP syndrome. Ophthalmic Genet 2004;25:153-6.
[Google Scholar]
|
| 9. |
Mégarbané H, Zablit C, Waked N, Lefranc G, Tomb R, Mégarbané A. Ichthyosis follicularis, alopecia, and photophobia IFAP syndrome: Report of a new family with additional features and review. Am J Med Genet A 2004;124A: 323-7.
[Google Scholar]
|
| 10. |
Ming A, Happle R, Grzeschik KH, Fischer G. Ichthyosis follicularis, alopecia, and photophobia IFAP syndrome due to mutation of the gene MBTPS2 in a large Australian kindred. Pediatr Dermatol 2009;26:427-31.
[Google Scholar]
|
| 11. |
Oeffner F, Fischer G, Happle R, König A, Betz RC, Bornholdt D, et al. IFAP syndrome is caused by deficiency in MBTPS2, an intramembrane zinc metalloprotease essential for cholesterol homeostasis and ER stress response. Am J Hum Genet 2009;84:459-67.
[Google Scholar]
|
| 12. |
Tang L, Liang J, Wang W, Yu L, Yao Z. A novel mutation in MBTPS2 causes a broad phenotypic spectrum of ichthyosis follicularis, atrichia, and photophobia syndrome in a large Chinese family. J Am Acad Dermatol 2011;64:716-22.
[Google Scholar]
|
Fulltext Views
5,811
PDF downloads
1,878





