Translate this page into:
Idiopathic eruptive macular pigmentation or acanthosis nigricans?
2 Keshav Skin and Hair Clinic and Dr. Hedgewar Hospital, Aurangabad, Maharashtra- 431 002, India
Correspondence Address:
Rajiv Joshi
14 Jay Mahal, A Road, Churchgate, Mumbai - 400 020
India
| How to cite this article: Joshi R, Palwade PK. Idiopathic eruptive macular pigmentation or acanthosis nigricans?. Indian J Dermatol Venereol Leprol 2010;76:591 |
Abstract
A 21-year-old male presented with numerous asymptomatic dark brown to brown black pigmented macules and barely raised plaques on the face, trunk and extremities, developing over a period of 2 year. The surface of most lesions had a velvety raised surface similar in appearance to acanthosis nigricans and a biopsy from one of the lesions showed pigmented papillomatosis. This case fulfils all the criteria for idiopathic eruptive macular pigmentation (IEMP) with papillomatosis, and the clinical appearance of acanthosis nigricans in most lesions suggests that IEMP is a form of eruptive acanthosis nigricans.Introduction
Idiopathic eruptive macular pigmentation (IEMP) is an uncommon condition characterized by the presence of asymptomatic pigmented macules that involve the face, trunk, and proximal extremities in children and adolescents. These dark brown and brown-black macules occur in crops and resolve gradually over months to years without any residual changes.
IEMP was first described in English literature by Sanz de Galdeano et al. in 1996, [1] and recently a paper by one of the authors (RJ) [2] described nine Indian cases which fulfilled the criteria for IEMP, with additional findings, namely acanthosis nigricans like appearance of some of the lesions and histological findings of pigmented papillomatosis in all the cases. This clinical and histological resemblance to acanthosis nigricans without involvement of sites normally involved in that condition prompted the author to speculate that IEMP may be an eruptive variant of acanthosis nigricans.
We present an additional case that fulfils all the criteria [1] for IEMP, and which also showed the velvety surface over most of the lesions, clinically resembling acanthosis nigricans, to add credence to the contention that IEMP is an eruptive variant of acanthosis nigricans.
Case Report
A 21 year apparently healthy and thinly built male presented to one of the authors (PP) with eruption of numerous asymptomatic dark brown to brown-black pigmented macules and barely elevated lesions on face, both extremities and trunk since 2 years. [Figure - 1],[Figure - 2],[Figure - 3] Lesions were asymptomatic and were not preceded by drug ingestion. Lesions had been present for a year before presentation and were progressively increasing in size and number. Lesions ranged in size from 0.5 cm to 2 cm in diameter and were approximately 30-40 in number. There was no scaling on the surface. Individual lesions had a peculiar velvety surface similar to acanthosis nigricans; however, flexural skin and folds typically affected by acanthosis nigricans were not involved. Mucosae, nail, palms, and soles were normal. None of the lesions had resolved till date and he continues to get new lesions.
He was treated with topical tretinoin 0.025% and emollient cream for a couple of months. There was not much of a change in the lesions except for slight scaling of lesional and perilesional skin.
 |
| Figure 1 : Multiple pigmented macules on trunk |
 |
| Figure 2 : Close up showing pigmentation and acanthosis nigricans like changes |
 |
| Figure 3 : Acanthosis nigricans like a lesion on arm |
The clinical diagnoses considered were lichen planus pigmentosus, fixed drug eruptions, and because of the close similarity of individual lesions to acanthosis nigricans, a possible variant of acanthosis nigricans, albeit without involvement of the typical sites was usually seen in that condition.
A skin biopsy taken from one of the lesions on the back showed prominent papillomatosis with elongated dermal papillae and a thickened basket-weave orthokeratotic, stratum corneum. The basal layer of the epidermis showed prominently increased melanin without any increase in the number of melanocytes at the dermoepidermal junction (pigmented papillomatosis). No significant dermal inflammation or melanin deposits in dermis were seen and no interface changes were evident [Figure - 4],[Figure - 5], [Figure - 6].
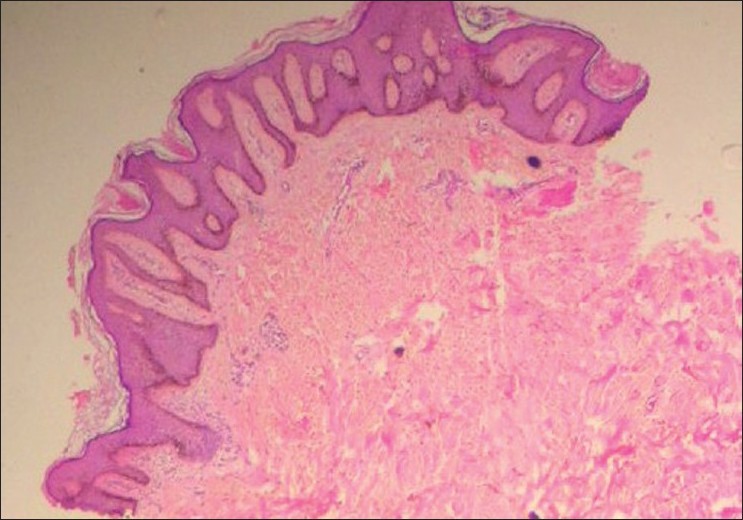 |
| Figure 4 : Scan of the biopsy of pigmented papillomatosis (H and E, ×25) |
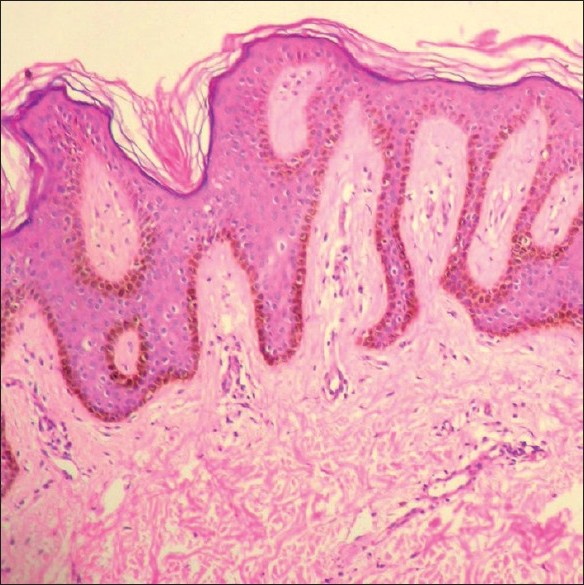 |
| Figure 5 : Photomicrograph showing pigmented papillomatosis (H and E, ×100) |
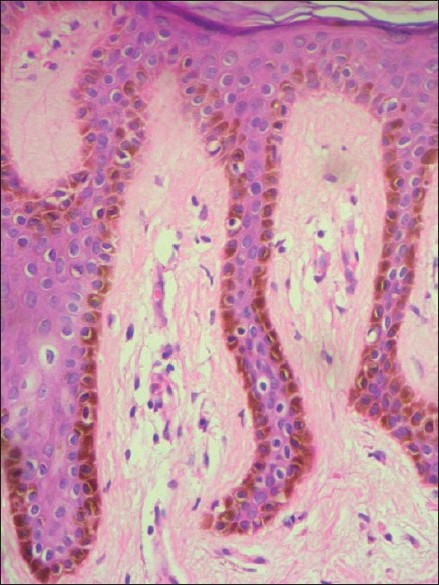 |
| Figure 6 : High power view showing increased pigmentation of the basal layer (H and E, ×400) |
This histology was consistent with acanthosis nigricans and ruled out both Lichen planus pigmentosus and fixed drug eruption.
However, the clinical findings of multiple pigmented macules with the histological findings of pigmented papillomatosis, fit in very well with IEMP with papillomatosis as described in a recent paper by one of the authors. [2]
Discussion
IEMP was first described in English literature by Sanz de Galdeano et al. in 1996, [1] and that paper gave criteria for diagnosis of this condition, namely (1) eruption of brown-black, discrete, non-confluent, asymptomatic macules involving the neck, trunk, and proximal extremities in children and adolescents; (2) absence of any preceding inflammatory lesions; (3) no previous drug exposure; (4) basal cell hyperpigmentation of the epidermis without any basal cell damage or lichenoid infiltrate; and (5) normal number of mast cells.
The clinical presentation of this condition is often mistaken for lichen planus pigmentosus, fixed drug eruption, or urticaria pigmentosa, but the biopsy findings of epidermal hypermelanosis and the absence of either interface changes or lichenoid infiltrate or mast cell infiltrate rules out those conditions.
The first report of this condition in Indian patients by one of the authors [2] highlighted two findings not described before, namely acanthosis nigricans like the clinical appearance of some of the lesions and histology of pigmented papillomatosis, findings consistent with acanthosis nigricans.
The case described in this paper fulfils all the above criteria and can be labeled as IEMP with papillomatosis. However, the lesions in this patient started developing at a later age, namely at age 19, and he continues to develop new lesions without any spontaneous resolution of lesions, which is expected in IEMP. Also most lesions clinically show a velvety dark brown-black surface very reminiscent of acanthosis nigricans, although typical acanthosis nigricans is not seen in flexural areas in this patient.
Is IEMP a distinct disease or is it a variant of Acanthosis nigricans?
Clinically and histologically, individual lesions of our patient and all the nine Indian cases described earlier [2] are indistinguishable from acanthosis nigricans.
Although this disseminated presentation of acanthosis nigricans has not been described before, we have an entity called IEMP which has multiple pigmented lesions that individually resemble acanthosis nigricans both clinically and histologically. It is logical therefore to assume that the entity IEMP is in fact nothing but a variation of acanthosis nigricans, to wit, eruptive acanthosis nigricans!
Acanthosis nigricans is known to occur in sites other than typical flexural sites like the dorsae of finger, lips, etc. and it is believed that certain growth factors stimulate the epidermis to give rise to the papillomatosis.
Trigger factors in developing acanthosis nigricans include obesity, underlying malignancy, and endocrine disturbances particularly peripheral insulin resistance.
The triggering factor/s in IEMP are not known and when more cases are described in the literature it is likely that the idiopathic from IEMP will be discarded and the condition be recognized for what it is, namely eruptive acanthosis nigricans.
| 1. |
Sanz de Galdeano CS, Leaute-Labreze C, Bioulac-Sage P, Nikolic M, Taieb A. Idiopathic eruptive macular pigmentation report of 5 patients. Pediatr Dermatol 1996;13:274-7.
[Google Scholar]
|
| 2. |
Joshi R. Idiopathic eruptive macular pigmentation with papillomatosis. Report of nine cases. Indian J Dermatol Venereol Leprol 2007;73:402-5.
[Google Scholar]
|
Fulltext Views
4,973
PDF downloads
2,580





