Translate this page into:
Image manipulation and image plagiarism – what's fine and what's not?
Correspondence Address:
Feroze Kaliyadan
Department of Dermatology, College of Medicine, King Faisal University, Hofuf
Saudi Arabia
| How to cite this article: Kaliyadan F. Image manipulation and image plagiarism – what's fine and what's not?. Indian J Dermatol Venereol Leprol 2017;83:519-521 |
The definition of scientific misconduct includes fabrication, falsification, or plagiarism in proposing, performing, or reviewing research or in reporting research results.[1] Images are also a form of scientific data and ideally need to be presented as such. Manipulating an image related to your research, therefore, will clearly fall under the ambit of research misconduct.[1] The question authors often ask is whether this means that images cannot be edited at all.
So What is OK?
- Cropping or resizing images to focus on the area of interest. Rotating the image for proper orientation (for example, to place in an anatomical position)
- Changing the image resolution. For example, most digital cameras give a default output of 72 DPI (Dots per inch), whereas most scientific journals require a minimum resolution of 300 DPI. There are no ethical issues in changing the resolution in such cases
- Tweaking parameters such as colour, contrast, brightness, and saturation. This is a bit of a tricky area. More often than not the raw clinical or histopathology image obtained from a digital camera can be improved by enhancing contrast, saturation, and/or sharpness. While it would be perfectly alright to make minor alterations in these parameters to improve the overall quality of the image, it would be unethical to do the same in situ ations such as pre-post images, where consistency is key to interpretation (A good example in this context is seen in the “instructions to authors” mentioned in the Journal of Cell Biology which mentions that they specifically screen for “whether any specific feature within an image has been enhanced, obscured, moved, removed, or introduced” (http://jcb.rupress.org/editorial-policies#data-integrity). Also, it would be unethical to significantly tweak these parameters in case of nonclinical data, such as fluorescent microscopy outputs, where even changes in saturation and contrast can lead to misinterpretation of data.[1],[2]
- Some amount of colour and sharpness enhancement is done by digital cameras themselves. In the case of pre-post images, this is fine as long as both the images are shot with the same camera using the same settings (flash, exposure, distance, zoom), however, the amount and type of internal image enhancement varies from camera to camera. This has to be kept in mind when using different cameras for pre and post images.
- Correcting the background. A good clinical image ideally needs a clean, nonreflective, and uniform background. Photo-editing software are useful in correcting distracting or cluttered backgrounds.
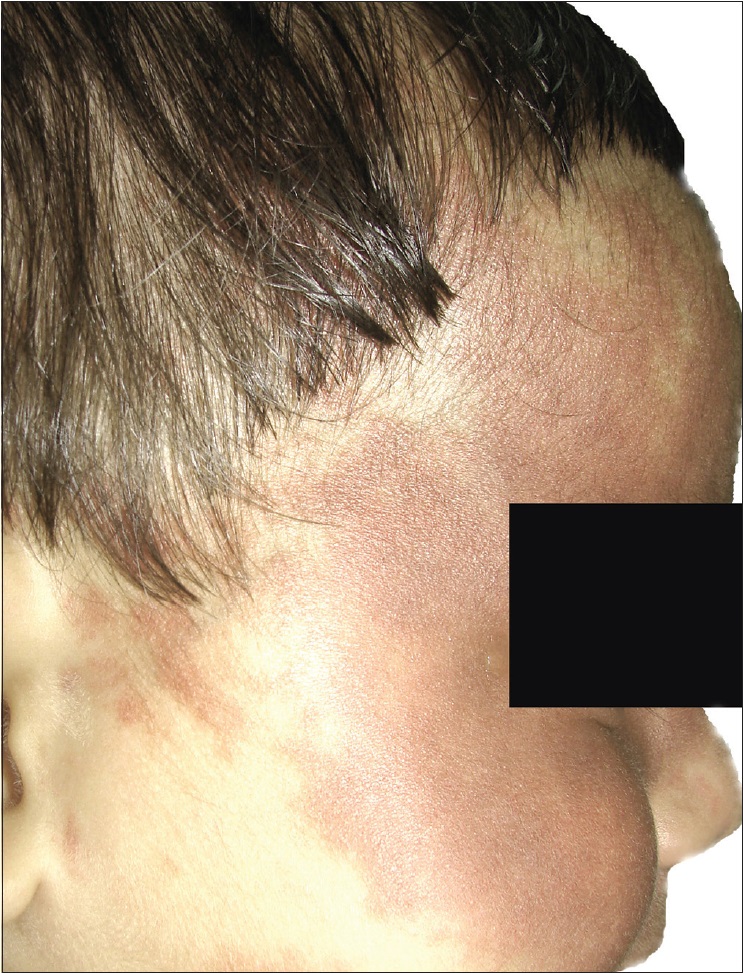
- Blackening out/blurring areas to maintain patient confidentiality [Figure - 1],[Figure 2a],[Figure - 3] and [Figure - 4].
 |
| Figure 1: Image of a port-wine stain over the face. The image is at a resolution of 72 DPI and has a cluttered, distracting background (the only editing done here is black box to cover the patient's eyes) |
 |
| Figure 2a: Acceptable corrections done include - rotation of the image, cropping/resizing, correction of the background, and change in the resolution to 300 DPI |
What is not OK?
- Making gross changes to the image to obscure or deceive the viewer – partially or completely by enhancing or obscuring specific features. In dermatology images, this is especially important in the context of pre-post images [Figure - 1], [Figure 2b] and [Figure 2c][1],[2]
- Image plagiarism – as mentioned before, images are also a form of valid clinical data and therefore all definitions of plagiarism apply to images too. In general, images available on the internet – clinical, histopathological, and line diagrams – have specific copyrights attributed to them. In case you want to use such an image you need to get explicit permission from the copyright holder (which might be either a person, a journal, or a publisher) and needs to be cited clearly. Some images come under the category of “creative commons.” Under the “creative commons,” the images can be used free of charge, but with proper attribution. Details of ideal attribution for creative commons images can be found here: https://wiki.creativecommons.org/wiki/Best_practices_for_attribution#This_is_an_ideal_attribution.
 |
| Figure 2b: Unacceptable corrections - here a photo-editing software has been used to remove pixels giving an apparent appearance of improvement (white arrow showing the area where the editing has been done) |
 |
| Figure 2c: Unacceptable corrections - here the saturation, brightness, and contrast has been adjusted, giving the impression of apparent improvement of the lesion |
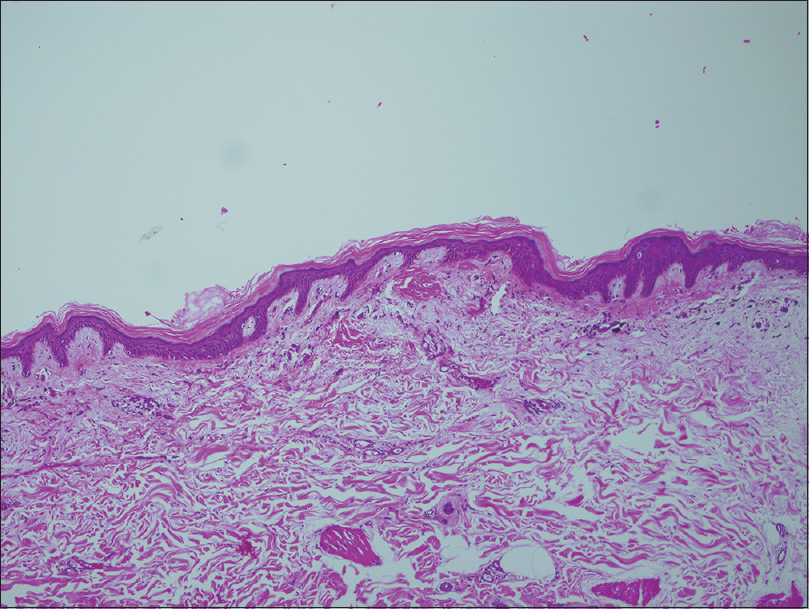 |
| Figure 3: Original histopathology image |
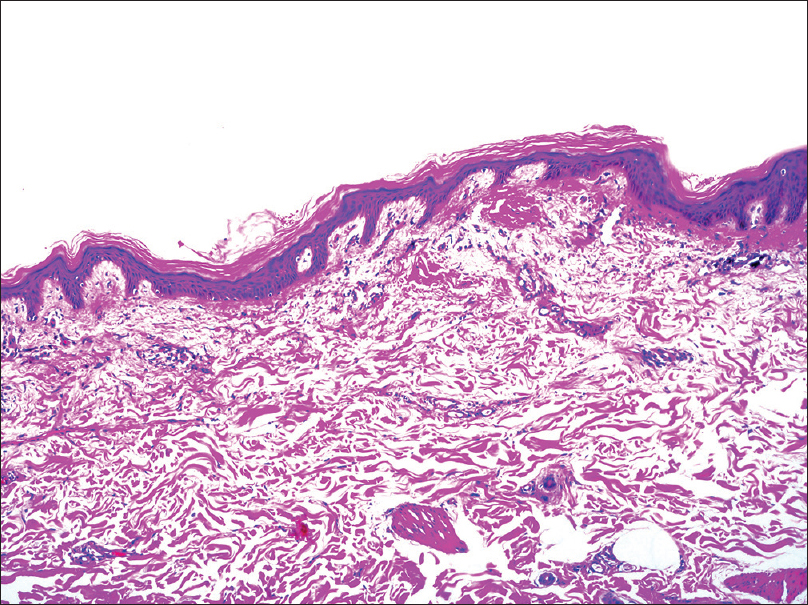 |
| Figure 4: Acceptable corrections for Figure 3 - The changes done include - cropping, resizing, adjusting contrast/brightness, and cleaning of some of the stain spots |
What should journals do?
- Give clear guidelines on image manipulation and adhere to strict practice of policies related to scientific misconduct in case of image manipulation and plagiarism
- Ask authors to submit original images (which automatically comes with the metadata related to the image file, which is normally seen in the direct output file from all digital cameras) along with the edited ones whenever significant editing has been done [Figure - 5]. In the same context, it is important that authors perform all image editing on a copy of the original file and never on the original itself. It should be noted that the metadata should include any data which might affect patient confidentiality, such as the patient's name. Journal policies in general have become stricter as far as patient confidentiality is concerned. In the United States, provisions under the Health Insurance Portability and Accountability Act (HIPAA) mention the following as “identifying information,” which should be removed to be consider “safe”[3]

Figure 5: Metadata from the original image file showing all relevant data tagged to the image - Patient's face
- Patient's name/initials
- Patient's date of birth
- Date of the medical service/visit
- Other obvious identifiers – birthmarks, moles, tattoos.
For journals, if removing some aspects is difficult (for example, if the lesion is on the face), the image should be accompanied with a clear and explicit signed consent form from the patient. Incidentally, HIPAA has relatively clear guidelines related to ideal practices of storage and sharing of patient images, but as of now such guidelines do not exist in the Indian context.[3]
- Strict screening for image plagiarism. Although checking for image plagiarism is not as effective as text plagiarism, it is now possible to detect gross image plagiarism with tools ranging from “Google image search” to specialized tools such as Plaghunter® (http://www.plaghunter.com/en/). Image plagiarism, like any other form of plagiarism, can significantly damage the reputation of researcher, besides having to deal with the legal implications of the same. A related form of unacceptable data manipulation is pairing of clinical images with histopathology images not related to the same case. This may be done primarily or in response to a referee's request for a better image
- IJDVL has started following a strict policy of screening for all kinds of plagiarism and scientific misconduct including those pertaining to images. The journal, after appropriate enquiry, will not shy away from acting strict action in cases where such misconduct is proven. Punitive actions can include blacklisting of authors involved
- To conclude, authors should treat images as they would treat any form of scientific data and need to practice due diligence when dealing with images to avoid any form of image manipulation or plagiarism amounting to scientific misconduct.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the legal guardian has given consent for images and other clinical information to be reported in the journal. The guardian understands that names and initials will not be published and due efforts will be made to conceal patient identity, but anonymity cannot be guaranteed.
| 1. |
Rossner M, Yamada KM. What's in a picture? The temptation of image manipulation. J Cell Biol 2004;166:11-5.
[Google Scholar]
|
| 2. |
Cromey DW. Avoiding twisted pixels: Ethical guidelines for the appropriate use and manipulation of scientific digital images. Sci Eng Ethics 2010;16:639-67.
[Google Scholar]
|
| 3. |
Alten E. Keep your dermatology practice HIPAA compliant with these 5 photo tips. Pract Dermatol 2017;14:56-8.
[Google Scholar]
|
Fulltext Views
4,800
PDF downloads
1,510





