Translate this page into:
Impressive reddish nodules with neoplastic-like appearance in a patient with Alzheimer’s disease
Corresponding author: Dr. Carmelo Schepis, Oasi Research Institute-IRCCS, Via Conte Ruggero 73, 94018 Troina, Italy. cschepis@oasi.en.it
-
Received: ,
Accepted: ,
How to cite this article: Siragusa M, Lentini M, Schepis C. Impressive reddish nodules with neoplastic-like appearance in a patient with Alzheimer’s disease. Indian J Dermatol Venereol Leprol 2021;87:300-2.
A deaf–mute, 71-year-old woman with Alzheimer’s disease was referred to us who presented with a voluminous left zygomatic reddish neoplastic-like lesion, with hard elastic consistency, well-defined edges and irregular ulcer covered with a thick blackish crust. Another similar smaller lesion, with a large brownish central scale, covered partially the left nasal pyramid, extending up to the inner canthus of the eye [Figure 1a]. The lesions had appeared approximately 5 months earlier. At first, none of the family members had paid any attention to them, considering the management of the behavioral disorder of the patient to be most important. The family doctor, who was consulted after a month, in consideration of the patient’s Alzheimer’s disease, hypothesized a self-injurious process and prescribed oral and topical antibiotic therapy for 1 week, without any benefit. For this reason, a dermatologist was later consulted, who diagnosed the condition as acute dermatitis and prescribed oral steroid therapy, which did not reduce the size of the lesions; instead they continued to grow with an even accelerated rate. The increasing size of the lesions worsened the psychomotor agitation of the patient; therefore, another dermatologist was consulted who confirmed acute dermatitis and administered intralesional steroid therapy with triamcinolone acetonide, once per week for 3 weeks, which only accentuated the neoplastic-like aspect of the lesions. At this clinical stage, the patient’s psychomotor agitation was uncontrollable, causing serious problems for her safety and making admission to our institute necessary.

- Left zygomatic reddish neoplastic-like lesion
The anamnesis, collected from family members, disclosed that the patient had never presented self-injurious behavior, and the inspection of the face, trunk and limbs did not show self-inflicted lesions. A 3-mm diameter biopsy from the larger lesion was then obtained which showed epidermal hyperplasia with acanthosis and mild parakeratosis. The papillary dermis showed ectatic vessels, extravasation of erythrocytes and variable numbers of neutrophils. In the mid dermis, a massive infiltrate of lymphocytes and parasitized macrophages could be seen [Figure 1b]. The parasites were round to oval, 2- to 4-nm basophilic, non-capsulated structures with eccentrically located kinetoplasts. The morphological details of endocellular amastigotes were better seen on Giemsa stain [Figure 1c].
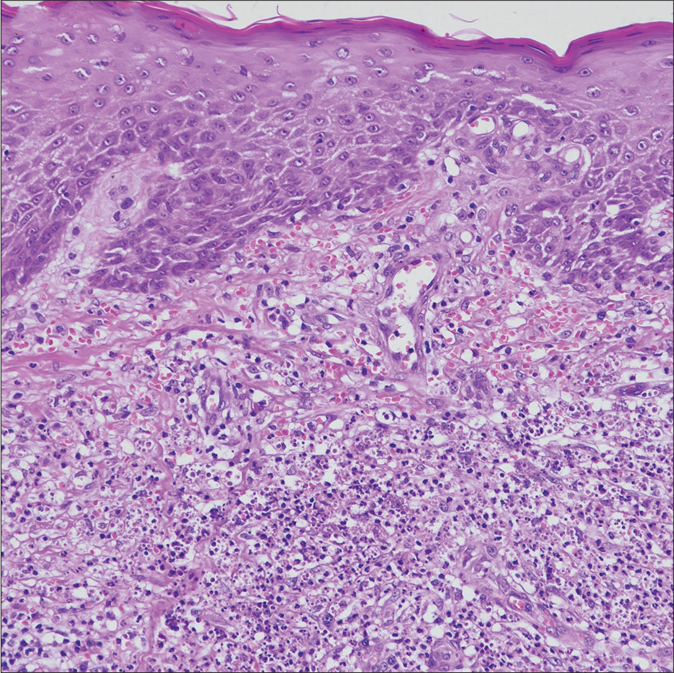
- Biopsy of the lesions showing in the mid dermis, a massive infiltrate of lymphocytes and parasitized macrophages (H and E, ×200)
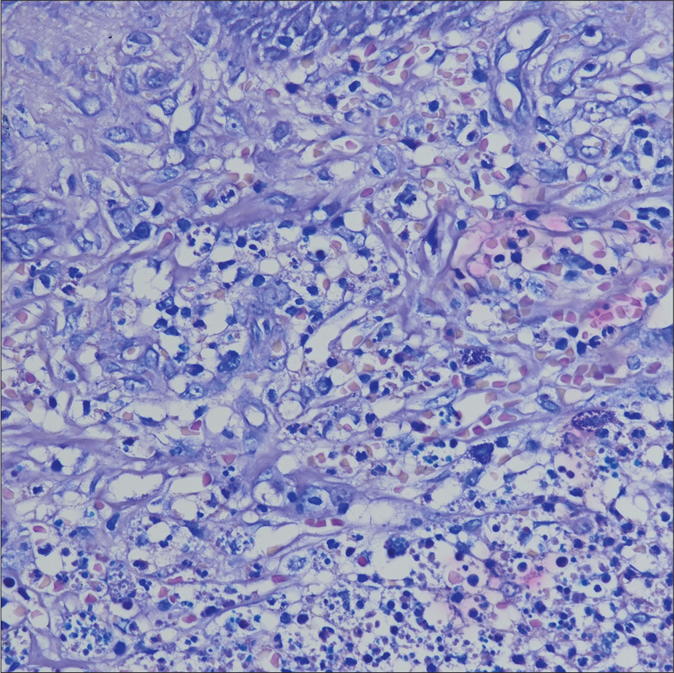
- Parasites in form of round to oval, 2 to 4nm basophilic, non capsulated structures (Giemsa stain preparation, ×400)
What Is Your Diagnosis?
Diagnosis
Atypical cutaneous leishmaniasis.
Discussion
We treated the lesions with intralesional injection of meglumine antemoniate, 1.5 mL/week. The diagnosis was also supported by the at-risk environment in which the patient lived (home was in a bad state, with cracks on the walls, surrounded by uncultivated vegetation where many stray dogs roamed). After 3 months of treatment, the patient was clinically healed [Figure 1d]; at a 1-year follow-up, the lesions had not recurred.

- Facial appearance after 3 months of treatment
Cutaneous leishmaniasis usually manifests itself with one single lesion, the so-called “Oriental sore,” located over the uncovered areas of the face. However, it is possible to observe additional lesions provoked by simultaneous or successive bites of phlebotomine sandfly, the insect that inoculates Leishmania, and this happens, above all, in patients living in endemic areas, as our patient did.1 In the literature, it is well known that cutaneous leishmaniasis can also manifest itself in atypical forms depending on the anatomical site, type of Leishmania species, delayed diagnosis, incorrect treatment (corticosteroids), or immunological status.1-4 We have published earlier a case of cutaneous leishmaniasis on the face and scalp, mimicking sebopsoriasis, in an immunosuppressed patient who was predisposed to psoriasis.3
In this new patient, the lesions did not, unfortunately, receive enough attention because of Alzheimer’s disease and above all, they received a wrong diagnosis and were subjected to incongruous therapies. We report this case to underline the necessity of prevention with an effective control of the vector (phlebotomine sandfly) and personal protection in endemic areas. It is important to remind the importance for dermatologists to correctly diagnose cutaneous leishmaniasis, especially in endemic areas. These measures should serve to avoid aberrant clinical forms with, sometimes pervasive, psychological and neurological repercussions in the most fragile patients, as in the case of our patient who was suffering from Alzheimer’s disease.
Acknowledgment
Special acknowledgments for this article are due to Mrs. Eleonora Di Fatta for her valuable assistance in the translation, preparation and formatting of the text.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Leishmaniosi cutanea atipica-Un interessante caso clinico. G Ital Dermatol Venereol. 2002;137:353-8.
- [Google Scholar]
- Atypical presentations of cutaneous leishmaniasis: A systematic review. Acta Trop. 2017;172:240-54.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic cutaneous leishmaniasis mimicking sebopsoriasis. Acta Derm Venereol. 1998;78:231.
- [CrossRef] [PubMed] [Google Scholar]
- Cutaneous leishmaniasis: An atypical case. Int J Dermatol. 2005;44:38-40.
- [CrossRef] [PubMed] [Google Scholar]





