Translate this page into:
Improvement of oral care in emergency setup including acute skin failure patients
2 Department of Oral Medicine and Radiology, Manipal College of Dental Science, Manipal University, Manipal, India
Correspondence Address:
Smitha Prabhu
Department of Dermatology & Venereology, Kasturba Medical College, Manipal University, Manipal
India
| How to cite this article: Prabhu S, Shenoi SD, Pandey S, Pai KM. Improvement of oral care in emergency setup including acute skin failure patients. Indian J Dermatol Venereol Leprol 2011;77:104-106 |
Introduction
Oral care in patients with dermatological emergency usually takes a back seat when the caregiver is absorbed in other important tasks like hourly movement of the patient, frequent feeds, cleaning and correctly scheduling medication. It is considered less important and understandably neglected. A study [1] has pointed out that emergency care nurses rate the importance of oral care at 53.9 on a scale of 0-100.
This article attempts to highlight the importance of oral health and its maintenance in the midst of daily routine, as it plays a larger than assumed role in the speedy recovery of the dermatological emergency patient.
Importance of Oral Care
There is a synergistic relationship between nutrition, oral health and diseases. The health of oral cavity is critical to general health and nutrition status. [1] In the absence of good health and immunity, even native bacteria may cause infection and a focus of infection can quickly spread to other tissue planes. The dermatological conditions where oral health is to be focused upon include patient with oral malignancy, any patient in intensive care unit, extensive mucocutaneous lesions as in pemphigus, Stevens Johnson syndrome, etc., and those with severe oral candidiasis secondary to immunosuppression, either congenital or acquired.
Factors responsible for poor oral health include oral microbial flora, dental plaque and poor oral immunity.
Oral Microbial Flora
Studies have shown that composition of oropharyngeal flora of critically ill patients undergoes a change from the usual predominance of Gram positive streptococci to predominantly Gram negative organisms, consisting more virulent flora including pathogens that may cause ventilator associated pneumonia (VAP). Oral cavity is the primary source of pathogens like Staphylococcus aureus and Streptococcus pneumoniae that cause VAP. [2]
Dental plaque
Dental plaque is a biofilm found on tooth surfaces, which provides habitat for microorganisms and serves as a reservoir for pathogens in patients with poor oral hygiene.
Oral immunity
Both innate and adaptive immunities are important to control the growth of microorganisms in the oral cavity. Oral immunity is influenced by salivary flow and immune components of saliva including IgA and lactoferrin.
Causes of compromised oral health in the bedridden patients include: [3]
- Primary medical condition or its treatment : Xerostomia is caused by many diseases including Sjogren′s syndrome and certain medications like antihistaminics.
- ICU equipment : Many critically ill patients have medical equipment in place, which traverse the oral or nasopharyngeal cavity, including airways, endotracheal tubes and feeding tubes. Placement of such devices may keep patient′s mouth continuously open, a situation that may contribute to xerostomia, which enhances accumulation of dental plaque and reduces salivary immune factors.
- Patients′ inability to attend to their own oral care : Oral self-care and water intake which counteracts xerostomia is limited in the critically ill patients, though in patients with dermatological conditions like toxic epidermal necrolysis (TEN), Stevens Johnson disease and oral pemphigus, there is increased salivation which aids in innate oral hygiene.
Common oral manifestations in a patient with dermatological emergency may include a combination of the following conditions like candidiasis, ulcers, stomatitis, glossitis, halitosis, gingivitis, periodontitis and odontogenic infection (based on clinical experience). Pseudomembranous candidiasis is one of the commonest oral manifestations in acute skin failure, which may be due to hampered epithelial integrity or steroid therapy.
Oral Care Regimens
The interventions can be broadly classified under mechanical, pharmacologic and combined interventions. [4]
Mechanical intervention
Warm saline gargles
This is one of the simplest and basic procedures which aid in maintaining oral hygiene. The patient is asked to gargle with warmed up normal saline or home prepared solution of warm salt water (in the proportion of 1 tsp salt to 2 glasses of water) at least thrice a day, preferably after meals.
Toothbrushes
Toothbrushes are the best tools for mechanical oral care and are found to be more effective than foam swab in plaque removal and gingival stimulation. In the bedridden patient, electrical toothbrushes may be used, which eliminate extensive arm action and are efficient plaque removers. Suction toothbrush units are best for patients who have lost their ability to swallow as in severe Stevens Johnson syndrome, TEN and oral pemphigus patients. Here, a suction reservoir evacuates the pooled toothpaste foam and saliva, thereby decreasing the chances of choking or aspiration pneumonia.
Swabs
Foam swabs, though not effective for plaque removal, provide mucosal stimulation and increase salivary flow, which contributes to local oral immunity. Hydrogen peroxide and sodium bicarbonate swabs are effective in removing debris, but may cause burns if not carefully diluted. Lemon and glycerin swabs were earlier used to stimulate production of saliva, but are now abandoned due to side effects.
Pharmacologic intervention
Chlorhexidine
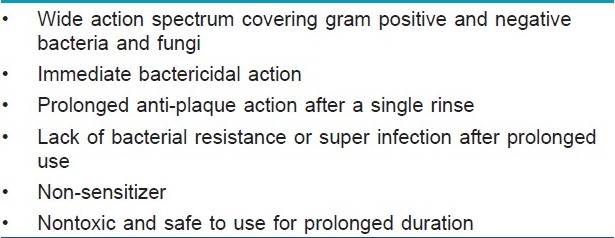
Chlorhexidine is considered to be the "gold standard mouth rinse" [5],[6] due to its various properties [Table - 1]. However, the following precautions need to be taken while using chlorhexidine. i) Not to use immediately before or after using tooth paste (interaction with anionic surfactants in the toothpaste will reduce the effective delivery of active form of chlorhexidine to the tooth surface). ii) Toothpaste to be used at least 30 minutes prior to chlorhexidine. iii) Excessive toothpaste to be rinsed off before applying chlorhexidine. Chlorhexidine sprays are also available.
Supportive therapy
This includes maintenance of proper nutrition and general care, use of topical analgesics (e.g. Diclofenac and Benzydamine hydrochloride 0.15%) and topical anesthetic (e.g. Lignocaine 2%) for painful conditions and proper rehydration.
Definitive therapy
This includes antiseptic mouth washes like triclosan 0.15% and topical antibiotics like tetracycline mouth wash (empty cap 250 mg in 5-10 ml of water and rinse four times daily). Topical corticosteroids like triamcinolone acetonide 0.1% in orabase, desensitizing and anticariogenic tooth pastes and topical/systemic antifungal drugs like clotrimazole, fluconazole are used whenever indicated.
Combination interventions
Combining the use of mechanical means with bactericidal agents is very effective in removal of dental plaque and pathogenic oral flora.
Conclusions
Oral health has a profound effect on the general health of the patient. Supportive oral care, either through mechanical intervention or combined with pharmacologic means, is very essential for the maintenance of health of bedridden and sick patients. So far, there have been no evidence-based oral care protocols for sick and bedridden. There is a sore need of studies for the development of best practice of oral care for the overall health of a critically ill patient.
| 1. |
Grap MJ, Munro C, Ashtiani B, Bryant S. Oral care interventions in critical care. Am J Crit Care 2003;12:113-9.
[Google Scholar]
|
| 2. |
Munro CL, Grap MJ. Oral health and care in the intensive care unit: State of science. Am J Crit Care 2004;13:25-34.
[Google Scholar]
|
| 3. |
Oral Care for the Patient with ALS: A Guide for the Caregiver. Available from: http://www.alsa.org/files/cms/Resources/Oral_Care.pdf [last accessed on 2010 Jun 17].
[Google Scholar]
|
| 4. |
Fitch JA, Munro CL, Glass CA, Pellegrini JM. Oral care in the adult intensive care unit. Am J Crit Care 1999;8:314-8.
[Google Scholar]
|
| 5. |
Jones CG. Chlorhexidine: Is it still the gold standard? Periodontol 2000;15:55-62.
[Google Scholar]
|
| 6. |
Addy M. The use of antiseptics in periodontal therapy. Chapter 22. In: Lindhe J, Karring T, Lang NP, editors. Clinical periodontology and implant dentistry. 4 th ed. Denmark: Blackwell Munksgaard; 2003. p. 41-7.
[Google Scholar]
|
Fulltext Views
6,737
PDF downloads
4,153





