Translate this page into:
Increased risk of atrial fibrillation in patients with psoriasis: A meta-analysis of observational studies
Corresponding author: Prof. Chieh-Chen Wu, Ming Chuan University, School of Health Technology, Department of Healthcare Information and Management. drluiswu@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Yang HC, Poly TN, Islam MM, Walther BA, Wu C. Increased risk of atrial fibrillation in patients with psoriasis: A meta-analysis of observational studies. Indian J Dermatol Venereol Leprol 2023;89:18-24.
Abstract
Background:
Several epidemiological studies have shown that psoriasis increases the risk of developing atrial fibrillation but evidence of this is still scarce.
Aims:
Our objective was to systematically review, synthesise and critique the epidemiological studies that provided information about the relationship between psoriasis and atrial fibrillation risk.
Methods:
We searched through PubMed, EMBASE and the bibliographies for articles published between 1 January 2000, and 1 November 2017, that reported on the association between psoriasis and atrial fibrillation. All abstracts, full-text articles and sources were reviewed with duplicate data excluded. Summary relative risks (RRs) with 95% CI were pooled using a random effects model.
Results:
We identified 252 articles, of these eight unique abstracts underwent full-text review. We finally selected six out of these eight studies comprising 11,187 atrial fibrillation patients. The overall pooled relative risk (RR) of atrial fibrillation was 1.39 (95% CI: 1.257–1.523, P < 0.0001) with significant heterogeneity (I2 = 80.316, Q = 45.723, τ2 = 0.017, P < 0.0001) for the random effects model. In subgroup analysis, the greater risk was found in studies from North America, RR 1.482 (95% CI: 1.119–1.964, P < 0.05), whereas a moderate risk was observed in studies from Europe RR 1.43 (95% CI: 1.269–1.628, P < 0.0001).
Limitations:
We were only able to include six studies with 11,178 atrial fibrillation patients, because only a few such studies have been published.
Conclusion:
Our results showed that psoriasis is significantly associated with an increased risk of developing atrial fibrillation. Therefore, physicians should monitor patient’s physical condition on a timely basis.
Keywords
Psoriasis
atrial fibrillation
autoimmune disease
skin disorder
cardiac disease
Plain Language Summary
Previous evidence has shown that psoriasis, a common chronic inflammatory skin disease, increases the risk of developing atrial fibrillation but evidence of this is still unclear. We systematically reviewed, synthesised and critiqued epidemiological studies that provided information about the relationship between psoriasis and atrial fibrillation risk. We found a 39% increased atrial fibrillation risk in patients with psoriasis. Physicians should be aware of this association. However, these results should be interpreted with caution due to the comprehensive analysis and clinical heterogeneity among the six studies. In the future, prospective studies are warranted to clarify this possible association because epidemiological studies do not provide information about a clear causal relationship.
Introduction
The prevalence of psoriasis varies considerably by age group; a higher prevalence in patients in the age group 50–69 years was found than in patients below the age of 50 years.1 Patients with psoriasis have an increased risk of several chronic diseases including hypertension, diabetes mellitus and dyslipidemia.2-4 In recent years, several publications reported that psoriasis is associated with an increased risk of cardiovascular diseases including stroke, heart failure, myocardial infarction, coronary artery disease and cardiovascular mortality.5-7 Recently, there has been a surge of interest in psoriasis because it is an autoimmune inflammatory disease and an independent risk factor for atrial fibrillation.
The relationship between psoriasis and atrial fibrillation remains unknown, and researchers have been unable to find a possible mechanism which might explain their possible relationship. Several epidemiological studies provided evidence which showed that P-wave duration (PWD) and atrial electromechanical delay (AEMD) are higher in patients with psoriasis than in healthy controls.8,9 Both these factors are linked to an increased risk for the development of atrial fibrillation.10,11 However, psoriasis also impaired atrial conduction function and eventually damaged atrial function whenever there was higher severity of psoriasis. In addition, the chronic systemic inflammatory process is responsible for an increased lymphocyte ratio and C-reactive protein (CRP) that can trigger atrial fibrillation by changing the atrial structure.12,13
We conducted a meta-analysis of observational studies to determine the magnitude of the association between psoriasis and atrial fibrillation risk.
Methods
This meta-analysis was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).14,15
Database
We developed a search strategy based on our previous experiences with similar studies.14,16,17 We searched in the electronic databases EMBASE, Google, Google Scholar, PubMed and Scopus for articles published between 1 January 2000, and 1 November 2017, that evaluated the association between psoriasis and atrial fibrillation risk. We used the following words as search terms: ‘psoriasis’ and ‘atrial fibrillation’. We also checked all the reference lists of the included full-text articles to find articles which we missed during the initial search. Google Scholar was also used to find academic articles citing eligible articles. However, any unpublished studies or references which existed only as abstracts were not included. We finally compiled all references in EndnoteX7 (Thomson Reuters) with duplicates removed using the Endnote search function.
Eligibility criteria
In the first stage, three authors (M.M.I., T.N.P. and CC, -Wu) screened and reviewed all titles and abstracts independently. First, the following criteria were established for the inclusion of any relevant study: (1) published in English, (2) reported original research using any observational study design (e.g., case–control or cohort study) and (3) reported the risk of atrial fibrillation with psoriasis. We, therefore, excluded all editorials, short communications and case studies.
Second, two authors (M.M.I. and T.N.P.) independently reviewed all the included full-text articles and excluded any duplicated studies. At this stage, studies were included if they, in addition to the above criteria, fulfilled two additional criteria: (1) Reported OR/HR with a 95% CI and (2) the number of participants was ≥50.
All disagreements between these two authors were resolved by consensus.
Data extraction
Using the above criteria, we identified six eligible studies, and the same authors (M.M.I and T.N.P.) then collected all necessary data for analyses. The data retrieved were as follows: (1) study information (e.g., author, year of publication, etc.), (2) study characteristics (age and gender of participants, location and duration of data collection), (3) condition information (i.e., data source, condition definition and total number of participants) and (4) study outcome to calculate summary estimate.
Assessment of methodological quality
The main goal of this meta-analysis was to evaluate the possible association between psoriasis and atrial fibrillation risk. We used the Newcastle-Ottawa Scale (NOS) to assess the methodological quality of the six included studies which were evaluated using three categories: selection (four stars), comparability (two stars) and assessment of the outcome of interest (three stars). The star rating system was used to evaluate the quality with a range 0–9 with 0–6 stars defined as low quality and 7–9 stars as high quality.
Primary and subgroup analysis
We investigated the association between psoriasis and atrial fibrillation risk as the primary analysis. We also performed subgroup analyses subdivided by age (<50 years and ≥50 years), study region (North America, Europe and Asia) and methodological quality (low vs. high, see star rating above).
Statistical analysis
We obtained the hazard ratios (HRs) and risk ratios (RRs) with 95% confidence intervals (CIs) for psoriasis and atrial fibrillation risk. We combined risk ratios with hazard ratios, estimating a common summary of relative risk.16 A relative risk value greater than one indicates an increased risk of atrial fibrillation, and a value less than one indicates a decreased risk of atrial fibrillation. We also assessed statistical significance using 95% CIs. If the 95% CI did not include the neutral value of one, we considered the risk to be statistically significant. The random effect model was used in this meta-analysis to evaluate the heterogeneity among studies. We used the comprehensive meta-analysis package (Version 3) to draw forest plots and for our subgroup analyses. The meta-analysis of proportion uses the binominal distribution for analysis. We quantified heterogeneity using the I2 statistic, and its significance was determined based on the accompanying P value in the Cochran Q test. An I2 value of 0% indicates no observed heterogeneity, and I2 values of 25%, 50% and 75% indicate low, moderate and high levels of heterogeneity, respectively. In addition, τ2 values arising from the random effects models were also used to quantify heterogeneity.
Results
Study selection
A total of 252 unique titles and abstracts were identified. Of these, 246 studies were excluded based on our eligibility criteria described in the methods. Six studies18-23 finally met all of our criteria for inclusion. Figure 1 summarises inclusion and exclusion criteria of the included studies.

- PRISMA flow diagram for study selection
Study characteristics
All the included studies were cohort studies [Table 1] and were published between 2012 and 2017,20 spanning six years. Two studies were from North America,21,23 three from Europe18,19,22 and one from Asia.20 Two studies categorised the atrial fibrillation risk according to age >50 and <50 years,22,23 two studies reported atrial fibrillation risk depending on the severity of psoriasis and one study analysed the atrial fibrillation risk according to gender difference. A total of 4,655,851 participants were included in our quantitative synthesis of which 11,187 were patients with atrial fibrillation.
| Authors | Year Country | Study design | Identification of AF | Study duration | Number of AF patients | HR/RR 95% CI | Adjustments |
|---|---|---|---|---|---|---|---|
| Rhee et al. | 2017 Korea | Cohort study | ICD-10 | 2004–2013 | 329 | HR=1.65 (1.48–1.84) | 1, 2, 3, 4, 5, 6, 7, 8 |
| Parisi et al. | 2015 UK | Cohort study | - | 1994–2009 | 877 | HR=1.54 (1.36–1.73) | 1, 2, 3, 6, 9, 11 |
| Bang et al. | 2014 USA | Prospective cohort study | Electrocardiograms | - | 506 | HR=1.97 (1.18–3.30) | 1, 2, 3, 16, 17, 18, 19, 20 |
| Armstrong et al. | 2013 USA | Cohort study | Electrocardiograms | 2004–2009 | 196 | HR=0.9 (0.50–1.80) | 1, 2, 3, 6, 9, 17, 19, 20 |
| Ahlehoff et al. | 2012 Denmark | Cohort study | CD-8: 427.94, 427.95, and ICD-10: I48 | 1997–2006 | 7,614 | RR=1.24 (1.16–1.32) | 1, 2, 14, 21, 22, 23, 25, 26, 27, 28, 29, 30 |
AF: Atrial fibrillation, HR: Hazard ratio, RR: Risk ratio. Adjustments: 1. Age, 2. Sex, 3. Diabetes mellitus, 4. Hypertension, 5. Dyslipidaemia, 6. congestive heart failure, 7. History of stroke, 8. History of myocardial infarction, 9. Hypertension, 10. Cardiomegaly, 11. Chronic kidney disease, 12. Use of Methotrexate, 13. Use of acitretin, 14. Use of nonsteroidal anti-inflammatory drugs, 15. Use of digoxin, 16. Serum haemoglobin, 17. Cholesterol level, 18. Serum creatinine, 19. Systolic blood pressure, 20. Diastolic blood pressure, 21. Valvular heart disease, 22. Peripheral vascular disease, 23. Cerebrovascular disease, 24. Ischaemic heart disease, 25. Previous myocardial infarction, 26. Chronic obstructive pulmonary disease, 27. Cancer, 28. Cardiac dysrhythmia, 29. Beta-blockers, 30. Calcium channel blockers
Methodological quality of included studies
Using the Newcastle-Ottawa Scale, the quality score of the six studies ranged from six to nine with a mean value of 7.1 [Table 2].
| Cohort Study | Selection | Comparability | Exposure | Total | |||||
|---|---|---|---|---|---|---|---|---|---|
| Selection of non-exposed cohort | Representativeness of the cohort | Ascertainment of exposure | Outcome of interest | Comparability of cohorts on the basis of the design or analysis | Assessment of outcome | Follow-up long enough for outcomes to occur | Adequacy of Follow-up of cohorts | (0–9) | |
| Rhee et al., 2017 | * | * | * | * | ** | * | * | * | 9 |
| Parisi et al., 2015 | * | * | * | * | * | * | 6 | ||
| Egeberg et al., 2015 | * | * | * | * | * | * | * | 7 | |
| Bang et al., 2014 | * | * | * | * | * | * | 6 | ||
| Armstrong et al., 2013 | * | * | * | ** | * | * | * | 8 | |
| Ahlehoff et al., 2012 | * | * | * | * | * | * | * | 7 | |
A “star (*)” system of the NOS has been developed for the methodological quality assessment: each study can be awarded a maximum of one star for each numbered item within the selection and exposure categories, while a maximum of two stars can be given for the comparability category. NOS: Newcastle-Ottawa Scale
Atrial fibrillation in patients with psoriasis
Based on the six included studies, atrial fibrillation risk was significantly higher in patients with psoriasis because the overall pooled relative risk of atrial fibrillation was 1.39 (95% CI:1.257–1.523, P < 0.0001) but was associated with significant heterogeneity (I2 = 80.316, Q = 45.723, τ2 = 0.017, P < 0.0001) when evaluated with the random effects model [Figure 2].
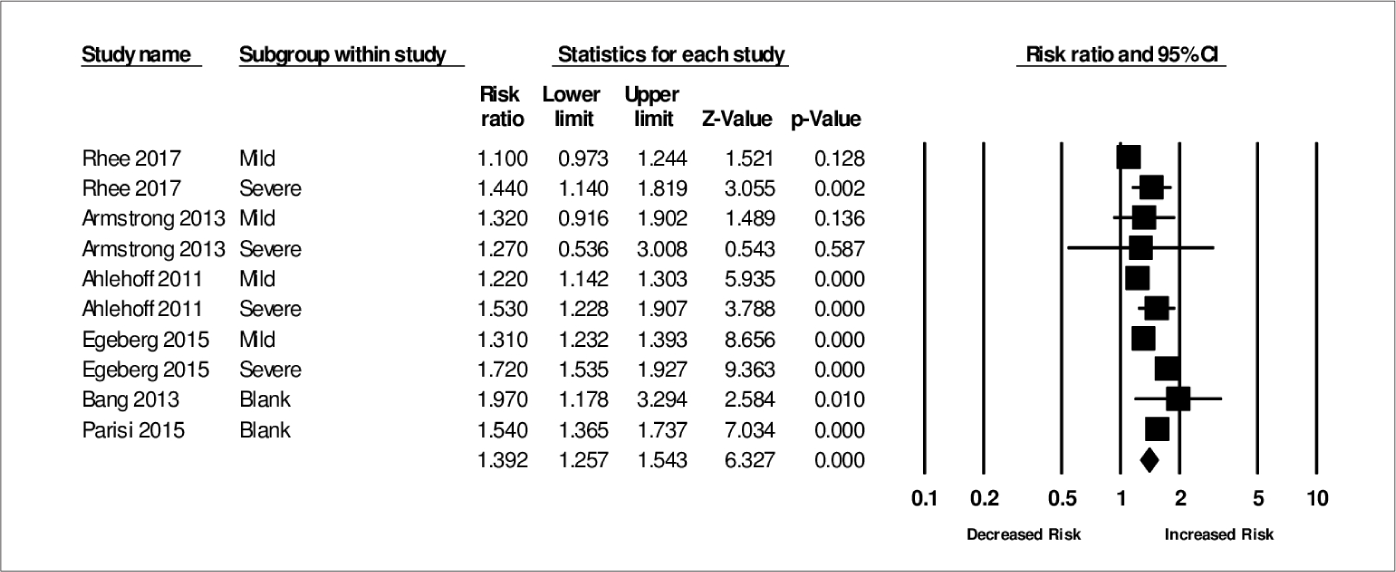
- Association between psoriasis and atrial fibrillation risk in the random effect model
Subgroup analyses
We also performed subgroup analyses to assess the influence of the study design, severity of psoriasis, region and age groups for atrial fibrillation risk and evaluated whether these characteristics could be the possible sources of heterogeneity [Table 3].
| Study | Pooled estimate | Test of heterogeneity | |||||
|---|---|---|---|---|---|---|---|
| Number of study | RR (95% CI) | P-value | τ2 | I2 (%) P-value | Model | ||
| All studies | 6 | 1.39 (1.257–1.523) | <0.0001 | 0.017 | 80.316 | <0.0001 | RE |
| Methodological quality | |||||||
| High quality | 4 | 1.351 (1.210–1.509) | <0.0001 | 0.016 | 81.037 | <0.0001 | RE |
| Low quality | 2 | 1.560 (1.387–1.754) | <0.0001 | 0.00 | 0.00 | 0.361 | RE |
| Region | |||||||
| Europe | 3 | 1.437 (1.269–1.628) | <0.0001 | 0.017 | 88.029 | <0.0001 | RE |
| America | 2 | 1.482 (1.119–1.964) | 0.006 | 0.00 | 0.0 | 0.430 | RE |
| Asia | 1 | 1.235 (0.951–1.603) | 0.114 | 0.027 | 74.956 | 0.046 | RE |
| Severity of psoriasis | |||||||
| Severe | 4 | 1.634 (1.490–1.791) | <0.0001 | 0.00 | 0.00 | 0.462 | RE |
| Mild | 4 | 1.229 (1.139–1.327) | <0.0001 | 0.003 | 57.291 | 0.071 | RE |
| Age | |||||||
| ≥50 | 2 | 1.170 (1.096–1.249) | <0.0001 | 0.00 | 0.00 | 0.709 | RE |
| <50 | 2 | 1.646 (0.865–3.129) | 0.129 | 0.224 | 77.056 | 0.013 | RE |
τ: Tau, RR: Risk ratio, RE: Random effect
Four studies provided atrial fibrillation risk estimates depending on the severity of psoriasis, defined as mild or severe psoriasis. The pooled relative risk for mild psoriasis was 1.229 (95% CI: 1.139–1.327, P < 0.0001), and the pooled relative risk for severe psoriasis was 1.634 (95% CI: 1.490–1.791, P < 0.0001).
The atrial fibrillation risk in patients with psoriasis was significantly higher in the two studies from North America with a relative risk of 1.482 (95% CI: 1.119–1.964, P < 0.001) and also in the three studies from Europe with a relative risk of 1.43 (95% CI: 1.269–1.628, P < 0.0001). However, the one study from Asia showed an increased but not statistically significant risk of atrial fibrillation in patients with psoriasis with a relative risk of 1.230 (95% CI: 0.951–1.603, P > 0.05).
We also separately assessed the four high-quality studies and found an increased risk of atrial fibrillation with a relative risk of 1.351 (95% CI: 1.210–1.509, P < 0.0001), while the relative risk was 1.560 (95% CI: 1.387–1.754, P < 0.0001) for the two low-quality studies.
In addition, two studies provided the risk estimation on the basis of age. The pooled relative risk for patients <50 years was 1.646 (95% CI: 0.865–3.129, P = 0.129) while for patients ≥50 years it was 1.170 (95% CI: 1.096–1.249, P < 0.0001).
Sensitivity analysis
Rhee et al.20 reported that atrial fibrillation risk was 77% higher in men with psoriasis (HR: 1.77, 95% CI: 1.58–2.04) and that women had a 51% increased atrial fibrillation risk (HR: 1.51, 95% CI: 1.28–1.79).
Publication bias
The meta-analysis of observational studies revealed several types of bias. If the number of included studies is not large, the visual interpretation and the test for asymmetry of the funnel plot help to understand potential publication bias.16,17
The funnel plot in Figure 3 indicates the existence of some publication bias. Using the Egger’s regression test of funnel asymmetry, we observed statistically non-significant publication bias (P > 0.05).
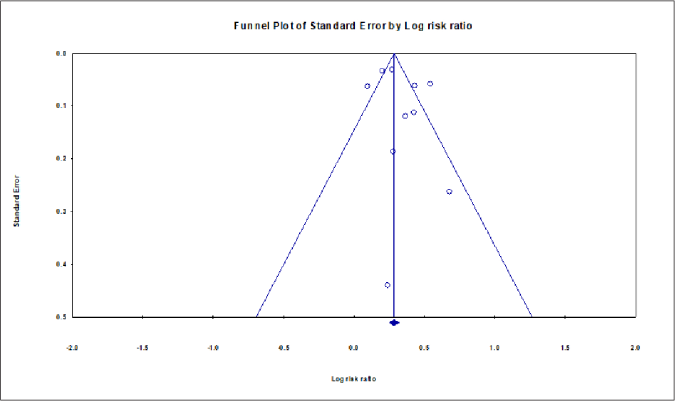
- Funnel plot shows the association between atrial fibrillation and psoriasis
Discussion
Principal findings
We conducted a meta-analysis to estimate the risk of atrial fibrillation in patients with psoriasis and found a 39% increased risk. These findings should alert physicians, but should be interpreted with caution due to the comprehensive analysis and clinical heterogeneity among the six studies. It is well known that results from epidemiological studies cannot clarify causal effects because they always have some unmeasured confounding variables. Our recommendation is, nevertheless, to closely observe the patient’s disease condition on a regular basis. If any symptoms of atrial fibrillation appear, then a more rigorous assessment is needed for diagnosis and appropriate treatment.
Biological plausibility
The mechanisms of the epidemiological association between psoriasis and atrial fibrillation risk remains unclear. There is no biological hypothesis yet which could explain how psoriasis could trigger the onset of atrial fibrillation. Nevertheless, several biological and pathophysiological mechanisms have been proposed as being responsible for this association. First, a study suggested that psoriasis enhances the chronic inflammatory process which might be associated with atrial fibrillation.24 Inflammatory components such as interleukin (IL)-2, IL-6, IL-12 and tumour necrosis factor, (TNF)-α, are independently associated with increased arterial stiffness which is a risk factor for atrial fibrillation.23,25 Second, a mouse model revealed that elevated levels of TNF-α and IL-17 in psoriasis patients could contribute to the onset of subsequent atrial fibrillation.26,27
Third, P wave dispersion (PWD) is an electrocardiographic marker which is related to the inhomogeneous and discontinuous distribution of the sinus impulse28 and is regarded as a non-invasive clinical biomarker of atrial fibrillation.29 Prolonged P wave dispersion has been associated with an increased risk for the development of atrial fibrillation.30 Similarly, atrial electromechanical delay (AEMD) is an echocardiographic parameter which is correlated with the onset of atrial fibrillation in some clinical conditions.11 Several studies reported that a prolonged P wave dispersion and atrial electromechanical delay were observed in psoriasis patients more often than in healthy people.9,31,32 This is attributed to the electrophysiological and atrium structural changes induced by increased inflammation in psoriasis. Though the exact biological link between atrial fibrillation risk and psoriasis remains inconclusive, our findings may prompt a fresh look at this problem and lead to better explanations for the epidemiological association which we report in this study.
Limitations
The results of this meta-analysis need to be interpreted within several limitations. First, we were only able to include six studies with 11,178 atrial fibrillation patients, because only a few such studies have been published so far. Second, there was substantial heterogeneity across the studies with different study designs, patients’ ascertainments, sample characteristics, assessments, outcomes and regional effects. It is known that the use of random effect models helps to reduce heterogeneity among studies. Third, we used the Egger test to evaluate the heterogeneity but the result was insignificant. Fourth, our finding was summarised from observational studies so that the main and subgroup analyses could not clarify the causal relationship between psoriasis and atrial fibrillation. Fifth, our study was unable to address several confounding factors such as smoking, depression and hypertension with left ventricular hypertrophy.
Recommendations and future research
Evidence from a number of biological and epidemiological studies suggests that the atrial fibrillation risk is increased in patients with psoriasis. In view of this evidence, it is necessary to encourage physicians to carefully monitor the patient’s condition and assess the risk of atrial fibrillation. In addition, more studies are warranted to support or refute this association. Finally, the exact role of genes, inflammatory pathways and other risk factors should also be evaluated.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Global epidemiology of psoriasis: a systematic review of incidence and prevalence. Journal of Investigative Dermatology. 2013;133:377-85.
- [CrossRef] [PubMed] [Google Scholar]
- Psoriasis is associated with lipid abnormalities at the onset of skin disease. J Am Acad Dermatol. 2006;54:614-21.
- [CrossRef] [PubMed] [Google Scholar]
- Psoriasis severity and the prevalence of major medical comorbidity: A population-based study. JAMA Dermatol. 2013;149:1173-9.
- [CrossRef] [PubMed] [Google Scholar]
- Increased risk of glomerulonephritis and chronic kidney disease in relation to the severity of psoriasis, concomitant medication, and comorbidity: A nationwide population-based cohort study. Br J Dermatol. 2015;173:146-54.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiological profile of atrial fibrillation: A contemporary perspective. Prog Cardiovasc Dis. 2005;48:1-8.
- [CrossRef] [PubMed] [Google Scholar]
- Coronary ischemic events after first atrial fibrillation: Risk and survival. Am J Med. 2007;120:357-63.
- [CrossRef] [PubMed] [Google Scholar]
- Inflammation, atherosclerosis, and coronary artery disease. N Engl J Med. 2005;352:1685-95.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of atrial electromechanical delay and left atrial mechanical functions in patients with psoriasis vulgaris. Echocardiography. 2015;32:615-22.
- [CrossRef] [PubMed] [Google Scholar]
- Electrocardiographic P-wave characteristics in patients with psoriasis vulgaris. Upsala J Med Sci. 2013;118:35-41.
- [CrossRef] [PubMed] [Google Scholar]
- P wave dispersion in hypertensive patients with paroxysmal atrial fibrillation. Pacing Clin Electrophysiol. 2000;23:1859-62.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of atrial electromechanical coupling and influential factors in nonrheumatic paroxysmal atrial fibrillation. Clin Cardiol. 2008;31:74-8.
- [CrossRef] [PubMed] [Google Scholar]
- Inflammation, oxidative stress and postoperative atrial fibrillation in cardiac surgery. Pharmacol Ther. 2015;154:13-20.
- [CrossRef] [PubMed] [Google Scholar]
- Inflammation and C-reactive protein in atrial fibrillation: Cause or effect? Tex Heart Inst J. 2014;41:461-8.
- [CrossRef] [PubMed] [Google Scholar]
- Exploring association between statin use and breast cancer risk: An updated meta-analysis. Arch Gynecol Obstet. 2017;296:1043-53.
- [CrossRef] [PubMed] [Google Scholar]
- The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009;6:e1000100.
- [CrossRef] [PubMed] [Google Scholar]
- Benzodiazepine use and risk of dementia in the elderly population: A systematic review and meta-analysis. Neuroepidemiology. 2016;47:181-91.
- [CrossRef] [PubMed] [Google Scholar]
- Exploring the association between statin use and the risk of Parkinson’s disease: A meta-analysis of observational studies. Neuroepidemiology. 2017;49:142-51.
- [CrossRef] [PubMed] [Google Scholar]
- Association between depression and risk of atrial fibrillation and stroke in patients with psoriasis: A Danish nationwide cohort study. Br J Dermatol. 2015;173:471-9.
- [CrossRef] [Google Scholar]
- Psoriasis and the risk of major cardiovascular events: Cohort study using the clinical practice research datalink. J Invest Dermatol. 2015;135:2189-97.
- [CrossRef] [PubMed] [Google Scholar]
- Increased risk of atrial fibrillation and thromboembolism in patients with severe psoriasis: A nationwide population-based study. Sci Rep. 2017;7:9973.
- [CrossRef] [PubMed] [Google Scholar]
- Psoriasis is associated with subsequent atrial fibrillation in hypertensive patients with left ventricular hypertrophy: The losartan intervention for endpoint study. J hypertens. 2014;32:667-72.
- [CrossRef] [PubMed] [Google Scholar]
- Psoriasis and risk of atrial fibrillation and ischaemic stroke: A Danish nationwide cohort study. Eur Heart J. 2012;33:2054-64.
- [CrossRef] [PubMed] [Google Scholar]
- Psoriasis, electrocardiographic characteristics, and incidence of atrial fibrillation. Arch Dermatol Res. 2013;305:891-7.
- [CrossRef] [PubMed] [Google Scholar]
- Heart rate and arrhythmia in patients with psoriasis vulgaris. Arch Med Res. 2007;38:64-9.
- [CrossRef] [PubMed] [Google Scholar]
- Aortic arterial stiffness is a moderate predictor of cardiovascular disease in patients with psoriasis vulgaris. Angiology. 2014;65:74-8.
- [CrossRef] [PubMed] [Google Scholar]
- Downregulation of connexin40 and increased prevalence of atrial arrhythmias in transgenic mice with cardiac-restricted overexpression of tumor necrosis factor. Am J Physiol Heart Circ Physiol. 2007;292:H1561-7.
- [CrossRef] [PubMed] [Google Scholar]
- Atrial contractile dysfunction, fibrosis, and arrhythmias in a mouse model of cardiomyopathy secondary to cardiac-specific overexpression of tumor necrosis factor-{alpha} Am J Physiol Heart Circ Physiol. 2005;289:H1456-67.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical and electrocardiographic predictors of recurrent atrial fibrillation. Pacing Clin Electrophysiol. 2000;23:352-8.
- [CrossRef] [PubMed] [Google Scholar]
- P-wave duration and the risk of atrial fibrillation: Results from the Copenhagen ECG study. Heart Rhythm. 2015;12:1887-95.
- [CrossRef] [PubMed] [Google Scholar]
- P wave duration and risk of longitudinal atrial fibrillation in persons = 60 years old (from the Framingham heart study) Am J Cardiol. 2011;107:917-21.e1.
- [CrossRef] [PubMed] [Google Scholar]
- Atrial electromechanical delay is impaired in patients with psoriasis. Med Princ Pract. 2015;24:30-5.
- [CrossRef] [PubMed] [Google Scholar]
- Assessment of atrial electromechanical delay and P-wave dispersion in patients with psoriasis. Echocardiography. 2014;31:1071-6.
- [CrossRef] [PubMed] [Google Scholar]






