Translate this page into:
Infantile hemangioma: An update
Correspondence Address:
Vibhu Mendiratta
RA- 24, Inderpuri, New Delhi - 12
India
| How to cite this article: Mendiratta V, Jabeen M. Infantile hemangioma: An update. Indian J Dermatol Venereol Leprol 2010;76:469-475 |
Abstract
Infantile hemangiomas (IH) are neoplastic proliferations of endothelial cells, characterized by a period of growth after birth, and eventual spontaneous involution. The course can be uneventful, culminating in spontaneous resolution; or it may be marked by complications such as bleeding; ulceration; infection; visual, feeding and breathing compromise; cosmetic and life-threatening complications such as congestive heart failure. Recognition of associated syndromes and impending complications of hemangiomas is of utmost importance. Great advances have taken place in the nomenclature, pathogenesis, immunohistochemistry, diagnostic workup and management of hemangiomas in the recent years. This article reviews current advances in the understanding of the pathogenesis, diagnostic tools, medical and surgical modalities of treatment for infantile hemangiomas.Introduction
Hemangioma is the commonest vascular tumor in childhood. [1] The etiopathogenesis of hemangioma of infancy remained surrounded by speculations and beliefs. Galen, the Greek physician, thought emotions of the mother to be the cause of vascular birthmark. The term "angioma" was designated by Virchow to refer to all vascular anomalies. The word "hemangioma" is derived from the Greek word haima, meaning blood. Hemangiomas are defined as benign neoplasms composed of proliferative and hyperplastic vascular endothelium. They exhibit rapid postnatal growth followed by slow involution, often leading to complete regression. Although most of these tumors are small and innocuous, some may be life- or function-threatening or have associated structural congenital anomalies. [2] The nomenclature and classification of hemangiomas have been the subject of great confusion. The term "hemangioma" has been used indiscriminately in the past to refer to a number of unrelated conditions, including vascular malformations and congenital hemangiomas. Hemangiomas differ significantly from these vascular lesions with regard to their clinical and histologic characteristics as well as long-term prognosis. [3]
In 1982, Mulliken and Glowacki [4],[5] classified hemangiomas based on the cellular biology and natural history of these lesions, dividing vascular birthmarks into two groups: hemangiomas and vascular malformations. [4],[5] A modification of this classification system was accepted by the International Society for the Study of Vascular Anomalies in 1996. [6]
The term "hemangioma of infancy" is the preferred and accepted term. The division into vascular malformations and tumors is not absolutely exclusive as rarely both coexist. [7] Terms like "cavernous hemangiomas" are best avoided to prevent confusion. Hemangiomas can be seen in 1.1% to 2.6% of term neonates, [8],[9] and their frequency is estimated to be as high as 10% to 12% within the first year of life. [10],[11] Among Indian studies, a prevalence varying from 0.1% to 0.28% has been reported. [12],[13] Female infants are three times as likely to have hemangiomas as compared to male infants, [14] and there is an increased incidence of premature and low-birth weight babies. [4],[15],[16] Approximately 55% of these tumors are present at birth, and 45% develop in the first weeks of life. [17] Infants who are exposed to chorionic villous sampling at 9-12 weeks of gestation develop hemangiomas in 21% of cases. [18]
Pathogenesis
Pathogenesis of infantile hemangioma is still shrouded in mystery, even though various theories have been postulated to explain its origin.
Immunohistochemical studies of hemangiomas confirm their vascular origin. Endothelial cells express cluster of differentiation-31 (CD31), von Willebrand factor, vascular endothelial growth factor (VEGF), proliferating nuclear antigen and urokinase. An imbalance has been demonstrated between the expression of angiogenic and antiangiogenic factors. Tissue inhibitors of metalloproteinase, a reported inhibitor of angiogenesis, are expressed in the involution phase. [19],[20] Endogenous steroid hormones (17-oestradiol) may play a role in the growth of infantile hemangiomas. [21]
Glucose transporter 1 (GLUT1), a glucose transporter normally expressed in the microvascular endothelia of blood-tissue barriers such as placenta, was recently described as a specific marker [22] for hemangioma vessels as it is absent in other vascular lesions such as malformation, RICH (rapidly involuting congenital hemangioma) and NICH (non-involuting congenital hemangioma). SKI oncogene protein is differentially expressed in hemangioma tissues, leading to uncontrolled cellular proliferation and transformation. [23]
Clinical Features
The growth characteristics of hemangiomas are often divided into phases: nascent, proliferating, involuting and involuted. [2] In approximately 50% of neonates, a premonitory mark may be evident as a telangiectatic macule surrounded by a pale halo, a pale macule, an erythematous macule or less commonly as a bruise or scratch. [24] By 1 year of age, most hemangiomas achieve their maximum size, ranging from 2 to 20 cm (average, 2 to 5 cm). A stationary phase predominates until 15 months of age. The involuting phase then begins, with the development of pale gray regions within the nodules and diminished firmness. Although superficial hemangiomas usually resolve with minimal atrophy, deep or mixed-type hemangiomas often show incomplete involution, with residual atrophic, wrinkled, telangiectatic, redundant skin. [25] Normal skin is restored in only 50% of all hemangiomas. [26] Hemangiomas of the tip of the nose, lip and parotid area are particularly slow to involute. [17] Finn et al., in a large series, found that 60% of hemangiomas occurred on the head and the neck, 25% on the trunk and 15% on the extremities. [4] Majority (80%) of patients have a single hemangioma; others have multifocal ones. [27] Multiple infantile hemangiomas, usually less than 10 in number, should be differentiated from disseminated or miliary hemangiomatosis with many hundreds of small hemangiomas. Infants with miliary hemangiomas are at a higher risk of having visceral hemangiomas, especially intrahepatic ones. [28]
Based on the location of hemangioma, 3 types are recognized: [25] Superficial plaque type, (65%); deeper, subcutaneous type (15%); and mixed, with both superficial and deep components (20%).
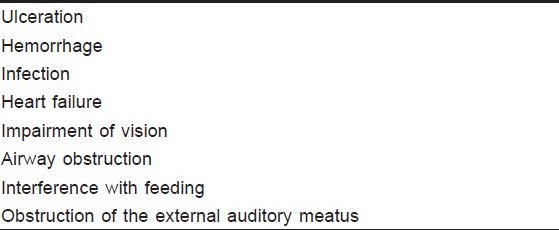
Hemangiomas can develop complications during their course, which can cause functional or cosmetic disability [Table - 1]. Complications depend on the location, size or the rate of growth and are found to occur in 40% of the lesions, the commonest being ulceration (21%) and bleeding (7.5%). [29] Ulceration is the most frequent complication of hemangiomas, possibly affecting 15% of all lesions. [30] It typically occurs during the proliferative phase, being more common in areas of mechanical trauma. Ulcerations are painful, can have secondary infection and bleeding and invariably heal with scarring. Localized bleeding from a hemangioma usually is a venous ooze that responds to pressure. Intralesional bleeding in a large hemangioma, associated with a rapid increase in the size of the lesion, should raise the question of a systemic coagulopathy or a misdiagnosed arteriovenous malformation. [31] Infection usually is the consequence of ulceration, but it is also seen as the primary complication in anatomic areas difficult to care for, such as the intraoral and perianal regions. [31] Multiple hemangiomas can cause shunting of large volumes of blood, which may lead to high-output heart failure. [3] Systemic hemangiomas are often, but not necessarily always, encountered in association with the small, multiple type of infantile hemangiomas. Such lesions may be found in liver, gastrointestinal tract, spleen, pancreas, lungs, heart, kidneys, bladder, testes, bone or brain. [31] Periocular hemangiomas can cause astigmatism, ptosis, strabismus, refractive errors, proptosis, amblyopia and blindness. Untreated subglottic hemangiomas, most concomitantly seen with cutaneous hemangiomas on the neck or lower part of face lesions, are associated with a mortality approaching 50% due to airway obstruction. [32] Feeding difficulties may complicate hemangiomas in the mouth and those that obstruct nasal breathing. Hemangiomas that encroach on the ear may obstruct the external auditory canal. Although this will interfere with hearing in the short term, it will generally not affect the development of normal ear function in the longer term. Very rarely, large infantile hemangiomas of the face may provoke overgrowth of the facial skeleton or of the auricular cartilage.
Syndromic Manifestations
PHACE(S) syndrome
Segmental facial hemangiomas have been reported in association with various anomalies, such as coarctation of the aorta, midline ventral defects and central nervous system (CNS) abnormalities. Frieden and Cohen [33] proposed the acronym PHACE(S) to unify the varying features of this syndrome: posterior fossa malformations, hemangioma, arterial anomalies, coarctation of the aorta and cardiac defects, eye abnormalities and occasionally sternal defects. PHACE(S) represents a spectrum of associated anomalies, as 70% of affected individuals will have only 1 extracutaneous manifestation.
Lumbosacral hemangiomas
Lumbosacral hemangiomas should alert the clinician to the possibility of occult spinal dysraphism, as well as genitourinary and anorectal anomalies. [34] Although these infants may initially be asymptomatic, tethering can cause progressive neurologic damage if not released.
Few studies have noted thyroid abnormalities in association with large hepatic hemangiomas. [35] High levels of type 3 iodothyronine de-iodinase were found in hemangioma tissue. This enzyme, normally expressed in the brain and placenta, is involved in the inactivation of thyroxine.
Diagnosis
In most instances, a hemangioma can be diagnosed based on the history and physical examination. However, differentiating between a deep hemangioma and a vascular malformation may be difficult. Doppler ultrasound is the least invasive and the most cost-effective imaging modality for hemangiomas. It is recommended as the initial test of choice to differentiate between vascular tumors and malformations. [36] Sonographic studies of proliferating hemangiomas show variable echogenicity, a high vessel density, high Doppler shift and low resistance. [37] Currently ultrasound and computed tomography (CT) and magnetic resonance imaging (MRI) are of limited value in making the distinction as both the lesions tend to be reported as "hemangioma". MRI with and without intravenous gadolinium is useful to evaluate the lesion extent and the associated anomalies. MRI also helps in differentiating from other high-flow vascular lesions (e.g., arteriovenous malformations vs. proliferating hemangiomas). Involuting hemangiomas have features that resemble low-flow lesions (e.g., venous malformations). Ultrasound is useful in differentiating hemangiomas from other deep dermal or subcutaneous structures, such as cysts or lymph nodes. Dubois et al. found that an evaluation exhibiting high vessel density (5 vessels/cm 2 ) and high peak arterial Doppler shift (exceeding 2 kHz) was both sensitive and specific for infantile hemangiomas compared with other soft tissue masses. [37] Plain radiography is fairly limited but may be useful for evaluating hemangiomas that impinge on the airway.
Invasive studies such as arteriography are best reserved for those patients requiring embolization. No laboratory studies have been universally accepted for the diagnosis and treatment of infantile hemangiomas; however, recent reports in the literature have investigated the use of urinary beta-fibroblast growth factor and serum vascular endothelial growth factor (VEGF) as markers of hemangioma proliferation and differentiation. [38] Platelet studies are not indicated as Kasabach-Meritt phenomenon is not associated with infantile hemangiomas. Biopsy of the proliferating hemangiomas shows masses of plump, rapidly dividing endothelial cells with and without lumens. Multilamination of the basement membrane is also seen. [5] As involution progresses, the vascular lumens dilate, endothelial cells flatten and fibrous tissue is deposited, giving the hemangioma a lobular architecture. Fully involuted hemangiomas contain few capillary-like feeding vessels and draining veins with flattened endothelium in a stroma of fibrofatty tissue, collagen and reticulin fibers. In addition to endothelial cells, hemangiomas contain pericytes, fibroblasts, interstitial cells and mast cells. [14]
Certain special investigations, such as brain imaging, are recommended in infants who have facial, segmental hemangiomas or are suspected to have PHACE syndrome. [2] For infants with open fontanelles, a cranial ultrasound is a valid screening option in detecting major structural defects. MRI is the most sensitive means for viewing the posterior fossa, and magnetic resonance arteriography can delineate arterial abnormalities. A careful cardiac examination with the blood pressure measurement in all 4 extremities to screen for coarctation of the aorta and ophthalmologic referral for suspected eye abnormalities are important.
Radiographic imaging is warranted in infants with hemangiomas overlying the lumbar or sacral spine and those with hemangiomas extending from the anus into the gluteal cleft. MRI best visualizes the spinal cord and thus is the preferred imaging study. [34] Some authors advocate routine hepatic ultrasound as a screening test for any infant with 5 or more cutaneous
hemangiomas. [14] On the other hand, testing can be costly and anxiety provoking, and others recommend using the history and physical examination as a guide to select tests. [39] Helpful studies may include a complete blood cell count, liver function tests, coagulation studies, urinalysis, stool examination for occult blood, chest radiograph, electrocardiogram or echocardiogram, abdominal imaging, CNS imaging and ophthalmology consultation. Thus infants with hemangiomas involving beard area need to be observed closely for signs of respiratory distress, particularly in the first 3 to 4 months of life, and be evaluated promptly with direct laryngoscopy if symptoms like biphasic stridor or croup-like cough develop.
Management
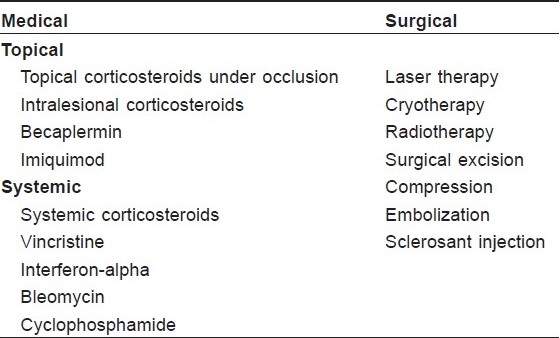
Various factors, namely, the size, site, amount of residual hemangioma, presence of associated complications, govern the selection of management modality of hemangiomas [Table - 2] and [Table - 3]. Active nonintervention is practiced in majority of cases as spontaneous involution is worth waiting for in cases of uncomplicated hemangiomas. Counseling of parents regarding careful observation of the course of hemangioma and reassurance are important aspects of management. Natural history of the lesion and prognosis should be explained to the parents. Periodic photographs will aid in documenting the evolution of hemangioma and to reassure parents that involution is actually occurring. Patients/parents/ caretakers should be advised to apply an emollient over the hemangioma to keep it soft and to keep nails of the baby trimmed. School-going children can have serious issues about their cosmetic appearance and social reactions, hence serious attention should be given to emotional and psychosocial issues in older children with disfiguring lesions.
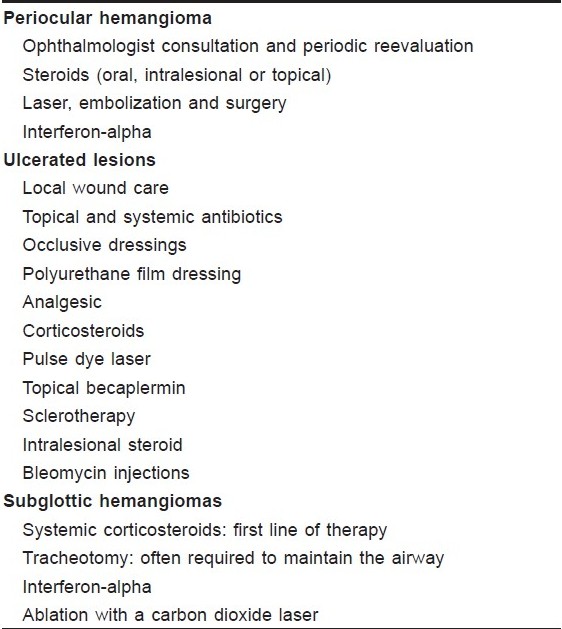
Systemic corticosteroids are the first-line treatment for problematic infantile hemangiomas, especially the large hemangiomas, which cause functional impairment or disfigurement. [40],[41] Steroids cause enhanced expression of genes coding for mitochondrial cytochrome band glycoproteins like clusterin/ ApoJ (markers of apoptosis), increased vasoconstriction and inhibition of angiogenesis. [42],[43],[44] Thus steriods are indicated in the treatment of infantile hemangioma. The recommended starting dose is 2-3 mg/kg of prednisolone given daily as a single morning dose, [2] with better response rate in the proliferative phase. [41]
High dose of steroids cause side effects which are usually transient in nature and include gastrointestinal upset, Cushingoid appearance, hypertension, decreased rate of growth and weight gain. [44],[45] Orbital hemangiomas, especially superficial ones, have been treated with intralesional steroids. Three to six injections of triamcinolone acetonide (10 mg/mL) at monthly intervals are usually given. In a Taiwanese study, 85% of patients responded with greater than 50% reduction in volume. [46] Side effects of intralesional steroids include cutaneous atrophy, depigmentation, eyelid necrosis, anaphylactic shock, embolism to retinal artery and retrobulbar hemorrhage. Topical clobetasol propionate has been used for treating periocular hemangiomas. [47],[48] They are best used for small superficial hemangiomas at risk of ulceration or small periocular lesions, but are not to be considered the first-line treatment for lesions causing ocular compromise.
Most experts limit the use of interferon alpha to life-threatening hemangiomas which have failed to respond to steroid therapy. [49],[50] It is given subcutaneously at a dose of 1 to 3 million U/m 2 of body surface area daily. It acts by acting as an inhibitor of angiogenesis. Fever, malaise, neutropenia, anemia and spastic diplegia are some of its side effects. Vincristine has been reported to be efficacious for large endangering hemangiomas in infants who fail to respond to steroids. [51],[52] The usual dose is 0.05 mg/kg or 1.5 mg/m 2 given i.v. on a weekly basis. Placement of a central venous line is often necessary to administer this medication because of its caustic nature. Cyclophosphamide has also been used for life-threatening cases (e.g., hemangiomatosis with heart failure) that are refractory to conventional treatment. [53] Intralesional bleomycin injection is an effective treatment option in hemangiomas, obviating the need for invasive primary surgery or systemic treatment regimens in 80% of cases. A complete response is seen in 49% of lesions. [54],[55] Side effects include superficial ulceration and cellulitis. Surgical excision is usually best done in the involuting or involuted phases; often this is done in stages. It is usually indicated in small, well-localized lesions of the eyelid, lip and neck or other parts of the body when it is likely to lead to an esthetically more acceptable scar.
Lasers can be used in proliferating hemangiomas in which active intervention is indicated owing to associated functional impairment or surface ulceration. [56] Flash lamp pulsed dye laser is useful in persistent telangiectasia and staining, (administered during the involuting and involuted stages), ulcerated hemangiomas and thin superficial hemangiomas, especially those on areas likely to result in significant functional or psychological impact (e.g., fingers, eyes, lips, nasal tip, ears, face).
Lasers that appear to be efficacious include the pulsed Neo dymium-Yttrium aluminium garnet (Nd:YAG), frequency-doubled Nd:YAG, and potassium titanyl phosphate (KTP) lasers. Each of these lasers has specific benefits and limitations regarding the depth of penetration, absorption of skin chromophores and caliber of the vessel treated. Complications also vary depending on the laser, settings and site treated.
Becaplermin (recombinant human platelet-derived growth factor) has been reported to be useful in ulcerated infantile hemangiomas, especially those in the diaper area. [57] Data is limited, and no report on a placebo-controlled trial has been published till date.
In proliferating hemangiomas, 5% Imiquimod cream has been found to be useful. [58] The action is mediated through activation of natural killer cells by Interferon-gamma, which has antiangiogenic effect. Side effects are minimal. Recently propranolol, a nonselective beta-blocker, has been found useful in proliferating hemangiomas. [59] Embolization is usually employed for hemangiomas complicated by congestive heart failure when medical management fails. [60] Intermittent pneumatic compression and continuous compression have been used to treat symptomatic hemangiomas, especially for lesions on the extremities, although the mechanism of action is unknown. [61],[62]
Cryosurgery with the use of a contact probe cooled by liquid nitrogen to treat isolated, raised lesions has been reported to hasten involution - though with risk of scarring. [63],[64]
Radiation therapy is rarely used given its carcinogenic risk and availability of better treatment choices, but may be considered as a last resort for infants with refractory life- or function-threatening hemangiomas. [65] Sclerotherapy with 1 to 3 injections of polidocanol has been used to obtain convincing results and is an inexpensive and promising treatment. [66] Local delivery of bisphosphonates as a potential treatment of hemangiomas is under research. [67]
| 1. |
Miller T, Frieden IJ. Vascular tumours. In: Wolff K, Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, editors. Fitzpatrick's dermatology in general medicine. 7 th ed. New York: McGraw-Hill; 2008. p. 1164-7.
th ed. New York: McGraw-Hill; 2008. p. 1164-7.'>[Google Scholar]
|
| 2. |
Bruckner AL, Frieden IJ. Hemangiomas of infancy. J Am Acad Dermatol 2003;48:477-93.
[Google Scholar]
|
| 3. |
Wahrman JE, Honig PJ. Hemangiomas. Pediatr Rev 1994;15:266-71.
[Google Scholar]
|
| 4. |
Finn MC, Glowaski J, Mulliken JB. Congenital vascular lesions: Clinical application of a new classification. J Pediatr Surg 1983;18:894-9.
[Google Scholar]
|
| 5. |
Mulliken JB, Glowacki J. Hemangiomas and vascular malformations in infants and children: A classification based on endothelial characteristics. Plast Reconstr Surg 1982;69:412-20.
[Google Scholar]
|
| 6. |
Enjolras O, Mulliken JB. Vascular tumors and vascular malformations (new issues). Adv Dermatol 1997;13:375-423.
[Google Scholar]
|
| 7. |
Garzon MC, Enjolras O, Frieden IJ. Vascular tumors and vascular malformations: Evidence for an association. J Am Acad Dermatol 2000;42:275-9.
[Google Scholar]
|
| 8. |
Pratt AG. Birthmarks in infants. Arch Derm Syphilol 1953;67:302-5.
[Google Scholar]
|
| 9. |
Jacobs AH, Walton RG. The incidence of birthmarks in the neonate. Pediatrics 1976;58:218-22.
[Google Scholar]
|
| 10. |
Jacobs AH. Strawberry hemangiomas: The natural history of the untreated lesion. Calif Med 1957;86:8-10.
[Google Scholar]
|
| 11. |
Holmdahl K. Cutaneous hemangiomas in premature and mature infants. Acta Paediatr 1955;44:370-9.
[Google Scholar]
|
| 12. |
Nanda A, Kaur S, Bhakoo ON, Dhall K. Survey of cutaneous lesions in Indian newborns. Pediatr Dermatol 1989;6:39-42.
[Google Scholar]
|
| 13. |
Baruah CM, Bhat V, Bhargava R, Garg RB, Ku. Prevalence of dermatoses in the neonates in Pondichery. Indian J Dermatol Venereol Leprol 1991;57:25-8.
[Google Scholar]
|
| 14. |
Mulliken JB, Fishman SJ, Burrows PE. Vascular anomalies. Curr Probl Surg 2000;37:517-84.
[Google Scholar]
|
| 15. |
Powell TG, West CR, Pharoah PO, Cooke RW. Epidemiology of strawberry haemangioma in low birthweight infants. Br J Dermatol 1987;116:635-41.
[Google Scholar]
|
| 16. |
Amir J, Metzker A, Krikler R, Reisner SH. Strawberry hemangioma in preterm infants. Pediatr Dermatol 1986;3:331-2.
[Google Scholar]
|
| 17. |
Drolet BA, Esterly NB, Frieden IJ. Hemangiomas in children. N Engl J Med 1999;341:173-81.
[Google Scholar]
|
| 18. |
Burton BK, Schulz CJ, Angle B, Burd LI. An increased incidence of hemangiomas in infants born following chorionic villus sampling (CVS). Prenat Diagn 1995;15:209-14.
[Google Scholar]
|
| 19. |
Takahashi K, Mulliken JB, Kozakewich HP, Rogers RA, Folkman J, Ezekowitz RA.Cellular markers that distinguish the phases of hemangioma during infancy and childhood. J Clin Invest 1994;93:2357-64.
[Google Scholar]
|
| 20. |
Tan ST, Velickovic M, Ruger BM, Davis PF. Cellular and extracellular markers of hemangioma. Plast Reconstr Surg 2000;106:529-38.
[Google Scholar]
|
| 21. |
Mulliken JB, Glowacki J. Hemangiomas and vascular malformations in infants and children: Classification based on endothelial characteristics. Plast Reconstr Surg 1982;69:412-22.
[Google Scholar]
|
| 22. |
North PE, Waner M, Mizeracki A, Mrak RE, Nicholas R, Kincannon J, et al. A unique microvascular phenotype shared by juvenile hemangiomas and human placenta. Arch Dermatol 2001;137:559-70.
[Google Scholar]
|
| 23. |
O TM, Tan M, Tarango M, Fink L, Mihm M, Ma Y, et al. Differential expression of SKI oncogene protein in hemangiomas. Otolaryngol Head Neck Surg 2009;141:213-8.
[Google Scholar]
|
| 24. |
Hidano A, Nakajima S. Earliest features of the strawberry mark in the newborn. Br J Dermatol 1972;87:138-44.
[Google Scholar]
|
| 25. |
Wirth FA, Lowitt MH. Diagnosis and treatment of cutaneous vascular lesions. Am Fam Physician 1998:57:765-73.
[Google Scholar]
|
| 26. |
Enjolras O, Mulliken JB. The current management of vascular birthmarks. Pediatr Dermatol 1993;10:311-3.
[Google Scholar]
|
| 27. |
Atherton DJ, Moss C. Naevi and other Developmental Defects. In: Burns T, Breathnach S, Cox N, Griffiths C, editors. Rook/ Wilkinson/ Ebling Textbook of dermatology. 7 th ed. Blackwell Science: Oxford; 2004. p. 15-60.
[Google Scholar]
|
| 28. |
Cohen RC, Myers NA. Diagnosis and management of hepatic hemangiomas in childhood. J Pediatr Surg 1986;21:6-9.
[Google Scholar]
|
| 29. |
Chiller KG, Passaro D, Frieden IJ. Haemangiomas of infancy: Clinical characteristics, morphologic subtypes and their relationship to race, ethnicity and sex. Arch Dermatol 2002;138:1567-76.
[Google Scholar]
|
| 30. |
Bruckner AL, Frieden IJ. Infantile hemangiomas. J Am Acad Dermatol 2006;55:671-82.
[Google Scholar]
|
| 31. |
Howell DM, Gumbiner CH, Martin GE. Congestive heart failure due to giant cutaneous cavernous hemangiomas. Clin Pediatr (Phila) 1984;23:504-6.
[Google Scholar]
|
| 32. |
Shikhani AH, Jones MM, Marsh BR, Holliday MJ. Infantile subglottic hemangiomas: An update. Ann Otol Rhinol Laryngol 1986;95:336-47.
[Google Scholar]
|
| 33. |
Freiden IJ, Reese V, Cohen D. PHACE syndrome. The association of posterior fossa brain malformations, hemangiomas, arterial anomalies, coarctation of aorta and cardiac defects, and eye abnormalities. Arch Dermatol 1996;132:307-11.
[Google Scholar]
|
| 34. |
Albright AL, Gartner JC, Wiener ES. Lumbar cutaneous hemangiomas as indicators of tethered spinal cords. Pediatrics 1989;83:977-80.
[Google Scholar]
|
| 35. |
Huang SA, Tu HM, Harney JW, Venihaki M, Butte AJ, Kozakewich HP, et al. Severe hypothyroidism caused by type 3 iodo thryronine-deiodinase in infantile hemangiomas. N Engl J Med 2000;343:185-9.
[Google Scholar]
|
| 36. |
Burrows PE, Laor T, Paltiel H, Robertson RL. Diagnostic imaging in the evaluation of vascular birthmarks. Dermatol Clin 1998;16:455-88.
[Google Scholar]
|
| 37. |
Dubois J, Garel L. Imaging and therapeutic approach of hemangiomas and vascular malformations in the pediatric age group. Pediatr Radiol 1999;29:879-93.
[Google Scholar]
|
| 38. |
Zhang L, Lin X, Wang W, Zhuang X, Dong J, Qi Z, et al. Circulating level of vascular endothelial growth factor in differentiating hemangioma from vascular malformation patients. Plast Reconstr Surg 2005;116:200-4.
[Google Scholar]
|
| 39. |
Special symposia. The management of disseminated eruptive hemangiomata in infants. Pediatr Dermatol 1984;1:312-7.
[Google Scholar]
|
| 40. |
Frieden IJ, Haggstrom AN, Drolet BA, Mancini AJ, Friedlander SF, Boon L, et al. Infantile hemangiomas: Current knowledge, future directions. Proceedings of a research workshop on infantile hemangiomas, April 7-9, 2005, Bethesda, Maryland, USA. Pediatr Dermatol 2005;22:383-406.
[Google Scholar]
|
| 41. |
Bennett ML, Fleischer AB Jr, Chamlin SL, Frieden IJ. Oral corticosteroid use is effective for cutaneous hemangiomas: An evidence-based evaluation. Arch Dermatol 2001;137:1208-13.
[Google Scholar]
|
| 42. |
Hasan Q, Tan ST, Gush J, Peters SG, Davis PF. Steroid therapy of a proliferating hemangioma: Histochemical and molecular changes. Pediatrics 2000;105:117-20.
[Google Scholar]
|
| 43. |
Hasan Q, Tan ST, Xu B, Davis PF. Effects of five commonly used glucocorticoids on haemangioma in vitro. Clin Exp Pharmacol Physiol 2003;30:140-4.
[Google Scholar]
|
| 44. |
Blei F, Chianese J. Corticosteroid toxicity in infants treated for endangering hemangiomas: Experience and guidelines for monitoring. Int Pediatr 1999;14:146-53.
[Google Scholar]
|
| 45. |
Boon LM, MacDonald DM, Mulliken JB. Complications of systemic corticosteroid therapy for problematic hemangioma. Plast Reconstr Surg 1999;104:1616-23.
[Google Scholar]
|
| 46. |
Chen MT, Yeong EK, Horng SY. Intralesional corticosteroid therapy in proliferating head and neck hemangiomas: A review of 155 cases. J Pediatr Surg 2000;35:420-3.
[Google Scholar]
|
| 47. |
Elsas FJ, Lewis AR. Topical treatment of periocular capillary hemangioma. J Pediatr Ophthalmol Strabismus 1994;31:153-6.
[Google Scholar]
|
| 48. |
Cruz OA, Zarnegar SR, Myers SE. Treatment of periocular capillary hemangioma with clobetasol propionate. Ophthalmology 1995;102:2012-5.
[Google Scholar]
|
| 49. |
Ricketts RR, Hatley RM Corden BJ, Sabio H, Howell CG. Interferon-alpha 2a for the treatment of complex hemangiomas of infancy and childhood. Ann Surg 1994;219:605-14.
[Google Scholar]
|
| 50. |
Chang E, Boyd A, Nelson CC, Crowley D, Law T, Keough KM, et al. Successful treatment of infantile hemangiomas with interferon-alpha-2b. J Pediatr Hematol Oncol 1997;19:237-44.
[Google Scholar]
|
| 51. |
Fawcett SL, Grant I, Hall PN, Kelsall AW, Nicholson JC. Vincristine as a treatment for a large haemangioma threatening vital functions. Br J Plast Surg 2004;57:168-71.
[Google Scholar]
|
| 52. |
Moore J, Lee M, Garzon M, Soffer S, Kim E, Saouaf R, et al. Effective therapy of a vascular tumor of infancy with vincristine. J Pediatr Surg 2001;36:1273-6.
[Google Scholar]
|
| 53. |
Hurvitz SA, Hurvitz CH, Sloninsky L, Sanford MC. Successful treatment with cyclophosphamide of life-threatening diffuse hemangiomatosis involving the liver. J Pediatr Hematol Oncol 2000;22:527-32.
[Google Scholar]
|
| 54. |
Kullendorff CM. Efficacy of bleomycin treatment for symptomatic hemangiomas in children. Pediatr Surg Int 1997;12:526-8.
[Google Scholar]
|
| 55. |
Muir T, Kirsten M, Fourie P, Dippenaar N, Ionescu GO. Intralesional bleomycin injection (IBI) treatment for haemangiomas and congenital vascular malformations. Pediatr Surg Int 2004;19:766-73.
[Google Scholar]
|
| 56. |
Tan OT, Gilchrest BA. Laser therapy for selected cutaneous vascular lesions in the paediatric population: A review. Pediatrics 1988;82:652-62.
[Google Scholar]
|
| 57. |
Metz BJ, Rubenstein MC, Levy ML, Metry DW. Response of ulcerated perineal hemangiomas of infancy to becaplermin gel, a recombinant human platelet-derived growth factor. Arch Dermatol 2004;140:867-70.
[Google Scholar]
|
| 58. |
Martinez MI, Sanchez-Carpintero I, North PE, Mihm MC Jr. Infantile Hemangioma: Clinical resolution with 5% imiquimod cream. Arch Dermatol 2002;138:881-4.
[Google Scholar]
|
| 59. |
Lιautι-Labrθze C, Dumas de la Roque E, Hubiche T, Boralevi F, Thambo JB, Taοeb A. Propranolol for severe hemangiomas of Infancy. New Engl J Med 2008;358:2649-51.
[Google Scholar]
|
| 60. |
Kassarjian A, Dubois J, Burrows PE. Angiographic classification of hepatic hemangiomas in infants. Radiology 2002;222:693-8.
[Google Scholar]
|
| 61. |
Stringel G. Giant hemangioma: Treatment with intermittent pneumatic compression. J Pediatr Surg 1987;22:7-10.
[Google Scholar]
|
| 62. |
Kaplan M, Paller AS. Clinical pearl: Use of self-adhesive, compressive wraps in the treatment of limb hemangiomas. J Am Acad Dermatol 1995;32:117-8.
[Google Scholar]
|
| 63. |
Cremer H. Cryosurgery for hemangiomas. Pediatr Dermatol 1998;15:410-1.
[Google Scholar]
|
| 64. |
Reischle S, Schuller-Petrovic S. Treatment of capillary hemangiomas of early childhood with a new method of cryosurgery. J Am Acad Dermatol 2000;42:809-13.
[Google Scholar]
|
| 65. |
Ogino I, Torikai K, Kobayasi S, Aida N, Hata M, Kigasawa H. Radiation therapy for life- or function-threatening infant hemangioma. Radiology 2001;218:834-9.
[Google Scholar]
|
| 66. |
Winter H, Drδger E, Sterry W. Sclerotherapy for treatment of hemangiomas. Dermatol Surg 2000;26:105-8.
[Google Scholar]
|
| 67. |
Yu H, Qin A. Could local delivery of bisphosphonates be a new therapeutic choice for hemangiomas? Med Hypotheses 2009;73:495-7.
[Google Scholar]
|
Fulltext Views
12,905
PDF downloads
5,107





