Translate this page into:
Infiltrated plaques on the face and back
Correspondence Address:
Marcia Ferreira
Hospital Geral de Santo Ant�nio, Consulta Externa de Dermatologia, Rua D. Manuel II, 4099 - 001 Porto
Portugal
| How to cite this article: Ferreira M, Teixeira M, Sanches M, Selores M. Infiltrated plaques on the face and back. Indian J Dermatol Venereol Leprol 2007;73:283-284 |
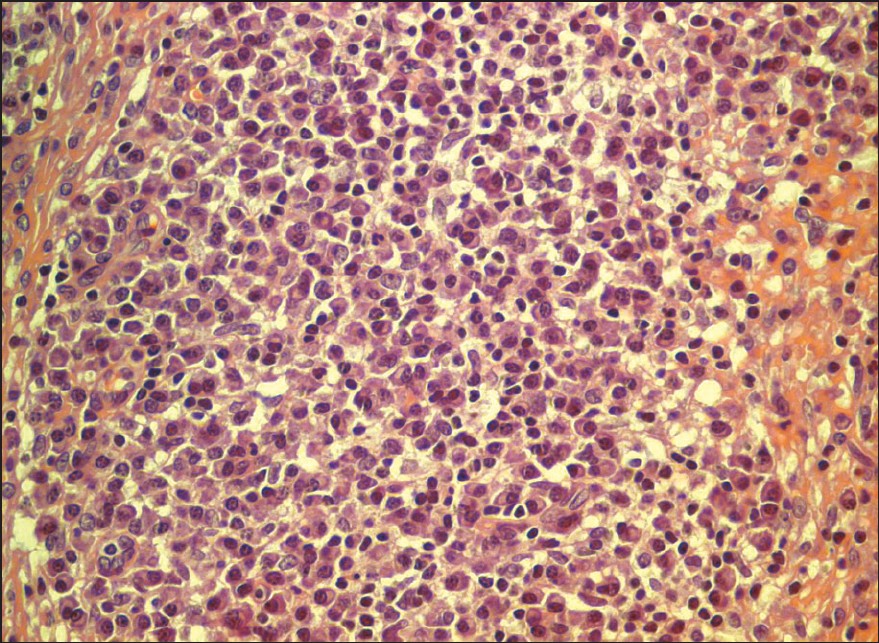 |
| Figure 4: High-power view of the infi ltrate showing lymphocytes and plasma cells (H and E, x400) |
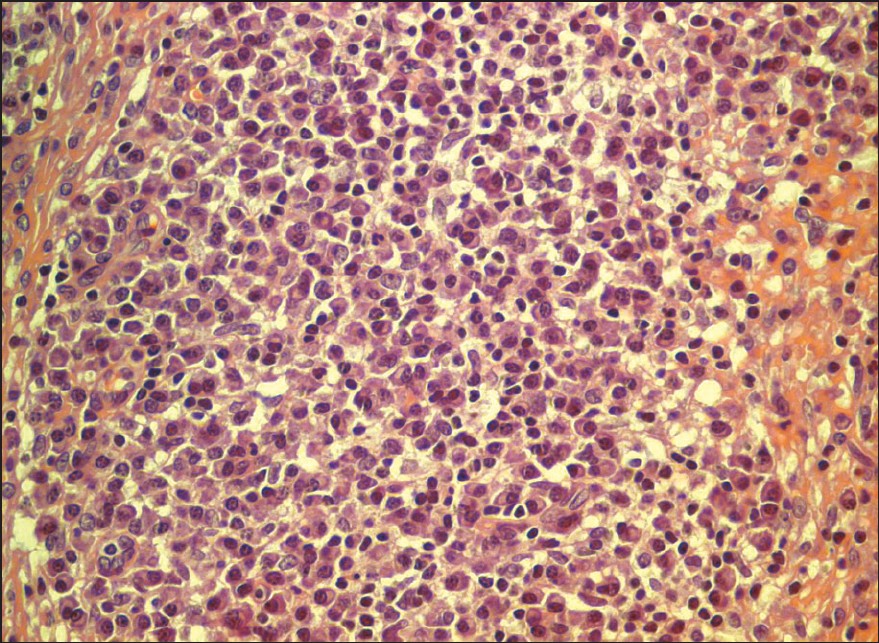 |
| Figure 4: High-power view of the infi ltrate showing lymphocytes and plasma cells (H and E, x400) |
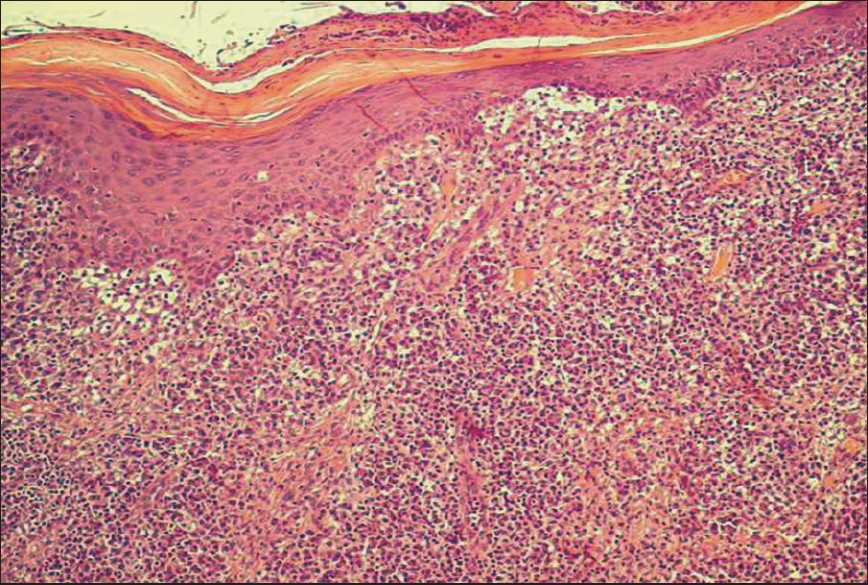 |
| Figure 3: Skin biopsy (H/ E, x100) |
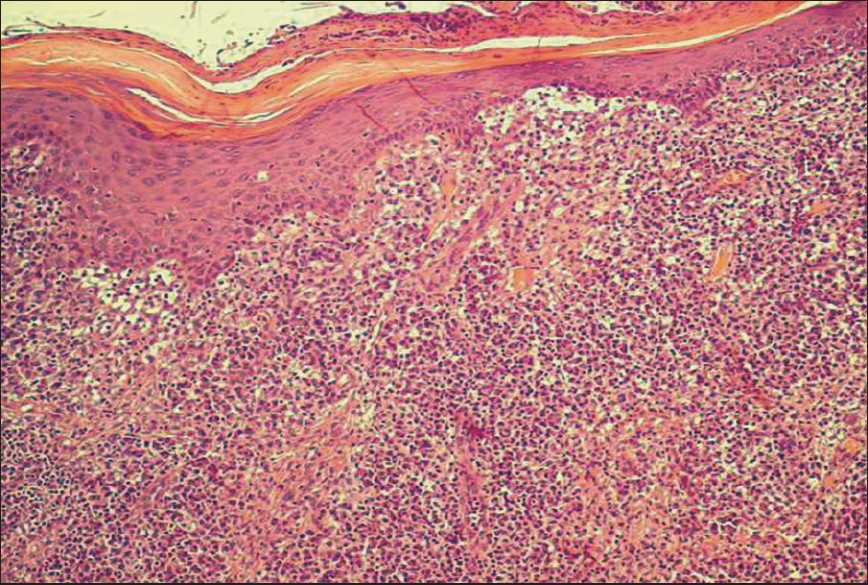 |
| Figure 3: Skin biopsy (H/ E, x100) |
 |
| Figure 2: Infi ltrated plaques on the upper back |
 |
| Figure 2: Infi ltrated plaques on the upper back |
 |
| Figure 1: Infi ltrated plaques on the forehead |
 |
| Figure 1: Infi ltrated plaques on the forehead |
A 31 year-old woman, previously healthy, presented a four-month history of enlarging plaques on the face and back without any constitutional complaints. She referred to one unprotected heterosexual contact but denied any past history of sexually transmitted infections. Physical examination revealed multiple, tumid, nontender erythemato-violaceous, slightly scaly, flat-topped plaques, distributed over her forehead [Figure - 1], left cheek, right oral commissure and back [Figure - 2]. Palms, soles, oral and genital mucosa were all free of lesions. There was no enlargement of lymph nodes, liver or spleen and the remaining physical examination was normal. Routine blood tests revealed an erythrocyte sedimentation rate of 84 mm at the end of one hour. Serological tests were negative for syphilis, hepatitis B and C and human immunodeficiency virus (HIV). Skin biopsy showed hyperkeratosis, focal parakeratosis and irregular acanthosis of the epidermis. There was a dense cellular infiltrate, grossly nodular, in the entire dermis [Figure - 3],[Figure - 4]. The results of the periodic acid-Schiff, Ziehl-Neelsen and Warthin-Starry stains were all negative. Cell-marker studies showed a heterogeneous population of cells without any phenotypic changes.
What is your Diagnosis ?
| 1. |
Sanchez MR. Syphilis. In : Freedberg IM, Eisen AZ, Wolff K, Austen KF, Goldsmith LA, Katz SI, editor. Fitzpatrick's dermatology in general medicine. 6 th ed. McGram-Hill: New York; 2003. p. 2163-87.
th ed. McGram-Hill: New York; 2003. p. 2163-87.'>[Google Scholar]
|
| 2. |
Hoang MP, High WA, Molberg KH. Secondary syphilis: A histologic and immunohistochemical evaluation. J Cutan Pathol 2004:31:595-9.
[Google Scholar]
|
| 3. |
Wenhai L, Jianzhong Z, Cao Y. Detection of Treponema pallidum in skin lesions of secondary syphilis and characterization of the inflammatory infiltrate. Dermatology 2004;208:94-7.
[Google Scholar]
|
| 4. |
Blum L, Bachmeyer C, Caumes E. Seronegative secondary syphilis in an HIV-infected patient. Clin Exp Dermatol 2005;30:158-9.
[Google Scholar]
|
| 5. |
Papini M, Bettacchi A, Guiducci A. Nodular secondary syphilis. Br J Dermatol 1998;138;704-5.
[Google Scholar]
|
Fulltext Views
4,713
PDF downloads
3,482






