Translate this page into:
Insight into evolution of a giant congenital nevomelanocytic nevus over 14 years
Correspondence Address:
B D Sathyanarayana
Departments of Dermatology, Venerology and Leprosy, Adichunchanagiri Institute of Medical Sciences, Bellur, Karnataka
India
| How to cite this article: Sathyanarayana B D, Basavaraj H B, Nischal K C, Swaroop M R, Lavanya M S, Okram S. Insight into evolution of a giant congenital nevomelanocytic nevus over 14 years. Indian J Dermatol Venereol Leprol 2014;80:243-246 |
Abstract
Giant congenital nevomelanocytic nevus (GCNN) is a rare variant of congenital melanocytic nevus measuring >20 cm in size that often has a garment-like distribution. Regular follow up is recommended because of a risk of melanoma transformation of 4.6%. We report a 14-year-old boy with gradual regression of giant congenital melanocytic nevus over the left upper limb, chest, back and axilla, whom we have followed-up since birth. At birth, a hyperpigmented jet-black patch without hair was present over the left side of torso and upper limb including palms and nails. Follow up at the ages of 1, 5, 11 and 14 years showed progressive spontaneous regression of the nevus resulting in shiny atrophic skin, diffuse hypopigmentation, lentigo-like macules, nodules and arthrogryphosis of affected areas. Histopathology of the lesions on follow-up revealed absence of pigmented nevus cells in the regressing areas and thickened sclerotic collagen bundles.INTRODUCTION
Congenital nevomelanocytic nevus is defined as a melanocytic neoplasia present at birth. These nevi are arbitrarily classified into 3 types based on their final size: small (up to 1.5 cm), medium (1.5-20 cm) and large (>20 cm). The large nevus is also called giant, garment or bathing trunk nevus. [1] A number of variants like the cerebriform congenital nevus, the spotted grouped pigment nevus, the congenital acral melanocytic nevus and the desmoplastic hairless hypopigmented nevus have also been described. [2] Management of giant nevi poses a problem from a dermatological as well as a cosmetic point of view.
The spontaneous regression of giant nevi has been documented in literature; however, the pattern of evolution has not been described. We report a case of giant nevomelanocytic nevus without hair with unusual features, whom we followed up for 14 years.
CASE REPORT
The patient was a full-term child born of a non-consanguineous marriage following an uneventful delivery. At birth, a hyperpigmented jet-black patch without hair was present over the left side of chest, back, axilla and upper limb including palm and nails [Figure - 1]a and b. The boy also had flexion contractures of the finger joints of the left hand and boggy swelling in the left axilla with inability to move his shoulder joint. Fine needle aspiration cytology of the boggy swelling revealed serous material with a few melanophages and lymphocytes. At 1 year of age, incision and drainage of the axillary swelling was done which healed with a hypertrophic scar. Subsequently, the patient was able to abduct his shoulder. At 5 years of age, some of the pigmented areas were replaced with thin shiny skin [Figure - 2], indicative of spontaneous gradual regression of the nevus. In addition, small firm nodules and plaques had appeared over the area of the nevus.
 |
| Figure 1: (a) At birth, hyperpigmented jet black patch without hairs over left chest, axilla, upper limbs including palms and nails. (b) Hyperpigmented jet black patch without hairs over the left upper back |
 |
| Figure 2: At 5 years, spontaneous regression of nevus is seen with thin shiny skin |
At 11 years of age, shiny atrophic skin, lentigo macules and arthrogryphosis was seen [Figure - 3]. There was an increase in the size and number of firm nodules. A verrucous plaque suggestive of a verrucous epidermal nevus was present over the left lateral neck. Histopathologic examination of lentigo-like lesions revealed nevus cells in the epidermis and dermis while biopsy from a regressed hypopigmented area showed interstitial distribution of nevus cells with thickened sclerotic collagen bundles. Biopsy of a firm nodule showed fibroplasia with superficial perivascular lymphocytic infiltrates. Biopsy of the verrucous plaque revealed acanthosis, basket weave type of ortho-hyperkeratosis and papillomatosis suggestive of verrucous epidermal nevus [Figure - 4]a-c.
At the age of 14 years, diffuse atrophy and hypopigmentation of skin with hypopigmentation was seen along with hyperpigmented macules and patches of varying sizes, concentrated mainly around the margins of the nevus and around the areola [Figure - 5]. Melanonychia was evident in all the finger nails along with contractures in all fingers of the left hand excluding the thumb [Figure - 6]. A firm 1 × 1 cm nodule was present over the lateral aspect of the left wrist overlying the styloid process of radius [Figure - 7]. Biopsy of the nodule revealed thickened collagen fibers in the papillary as well as reticular dermis. Collagen fibers were arranged in bundles in the reticular dermis. Pigmented nevus cells were not visualized in the epidermis and dermis. [Figure - 8]. Contractures were released and physiotherapy was recommended.
 |
| Figure 3: At 11 years, thin shiny atrophic skin, lentigo like macules and arthrogryphosis |
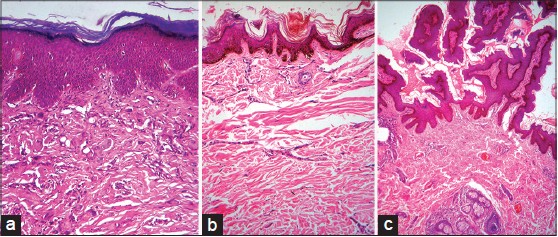 |
| Figure 4: (a) Biopsy from a lentigo-like macule: nevus cells in epidermis and dermis. (b) Biopsy from a hypopigmented area: interstitial distribution of nevus cells with thickened sclerotic collagen bundles. (c) Biopsy from a fi rm nodule: fi broplasia with a superfi cial perivascular lymphocytic infi ltrate |
 |
| Figure 5: At 14 years, diffuse atrophy and hypopigmentation of skin over the nevus with scattered hyperpigmented macules |
 |
| Figure 6: Hyperpigmented macules over left palm and melanonychia of all fi nger nails |
 |
| Figure 7: A fi rm nodule 1 × 1 cm present over lateral aspect of the left wrist overlying the styloid process of left radius |
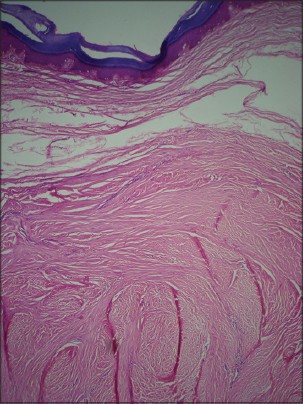 |
| Figure 8: Biopsy from a nodule on the left wrist: collagen fibers arranged in bundles in the reticular dermis with no pigmented nevus cells in the epidermis and dermis. Lamellated orthohyperkeratosis was seen in the epidermis |
DISCUSSION
Most congenital nevomelanocytic nevi are small and single. There is no sex predilection. Small nevi are seen at a frequency of 1 in 20,000 births, whereas giant congenital nevomelanocytic nevi are rarer and seen at a frequency of 1 in 500,000 births. [1] They manifest as hyperpigmented (black to brown in color), round, oval or irregular circumscribed areas of skin covering 1% of the body surface area on the face and neck and 2% elsewhere on the body. They often have a garment-like or bathing-trunk distribution. The lesions may be covered with a mild to moderate amount of hair initially with a gradual increase in density in later childhood. The surface may be smooth, pebbly, verrucous, cerebriform or lobular. Multiple small satellite nevi may be present either at birth or during early childhood (tardive satellite). [1],[3]
The follow-up of giant congenital nevomelanocytic nevi is important because of their tendency toward melanoma transformation. It is estimated that 4.6% of patients with congenital giant nevi are at a risk of developing malignant melanoma. [4] The risk of malignant transformation is well documented in lesions involving more than 5% of the body surface area. [5] These nevi might be associated with several other conditions namely neurocutaneous melanosis, rhabdomyosarcoma, liposarcoma, tethered cord syndrome, diffuse lipomatosis, structural brain malformations, hypertrophy of skull bones, limb atrophy, musculoskeletal asymmetry, von Recklinghausen disease and vitiligo. [6],[7] Spontaneous regression occurs rarely in pigmented lesions and this process may be associated with the development of a depigmented halo or vitiligo. [8]
Discrete dermal nodular proliferations commonly referred to as "proliferative nodules," "atypical dermal nodules," "atypical epithelioid tumors in congenital nevi" or "proliferative dermal lesions" can be identified in congenital nevi. Later, these nodules may reduce in size, become soft and even regress completely. [9] Similar such nodules were also seen in our case which regressed in size in later stages. An unusual case of congenital melanocytic nevus was reported in a 19-year-old African woman by Rose et al., in which widespread papules and variably sized nodules and tumors were present. Fibrosis was reported in the histopathology of the nodules. [10]
Our patient showed some unusual features: absence of hair on the nevus, development of lentigo-like pigmented macules, sclerodermoid fibrosis, fibrous nodules and hypopigmented patches at areas of spontaneous regression and association with a verrucous epidermal nevus. Long term follow up provided an opportunity to record the evolution of this giant congenital nevomelanocytic nevus.
| 1. |
Grichnik JM, Rhodes AR, Sober AJ. Benign neoplasias and hyperplasias of melanocytes. In: Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K, editors. Fitzpatrick's Dermatology in General Medicine. 8 th ed. New York: McGraw Hill; 2012. p. 1377-82.
th ed. New York: McGraw Hill; 2012. p. 1377-82.'>[Google Scholar]
|
| 2. |
Elder DE, Elenitsas R, Murphy GF, Xu X. Benign pigmented lesions and malignant melanoma. In: Elder DE, editor. Lever's Histopathology of the Skin. 10 th ed. New Delhi: Wolters Kluwer Health/Lippincott Williams and Wilkins; 2009. p. 725-38.
th ed. New Delhi: Wolters Kluwer Health/Lippincott Williams and Wilkins; 2009. p. 725-38.'>[Google Scholar]
|
| 3. |
Bhagyalakshmi A, Sudhakar P, Uma P, Devi PU. Giant congenital melanocytic nevus scalp: report of a rare case. Int J Res Med Sci 2013;1:317-9.
[Google Scholar]
|
| 4. |
Lorentzen M, Pers M, Bretteville-Jensen G. The incidence of malignant transformation in giant pigmented nevi. Scand J Plast Reconstr Surg 1977;11:163-7.
[Google Scholar]
|
| 5. |
Swerdlow AJ, English JS, Qiao Z. The risk of melanoma in patients with congenital nevi: A cohort study. J Am Acad Dermatol 1995;32:595-9.
[Google Scholar]
|
| 6. |
Chung C, Forte AJ, Narayan D, Persing J. Giant nevi: A review. J Craniofac Surg 2006;17:1210-5.
[Google Scholar]
|
| 7. |
Bhagwat PV, Tophakhane RS, Shashikumar BM, Noronha TM, Naidu V. Giant congenital melanocytic nevus (bathing trunk nevus) associated with lipoma and neurofibroma: Report of two cases. Indian J Dermatol Venereol Leprol 2009;75:495-8.
[Google Scholar]
|
| 8. |
Nath AK, Thappa DM, Rajesh NG. Spontaneous regression of a congenital melanocytic nevus. Indian J Dermatol Venereol Leprol 2011;77:507-10.
[Google Scholar]
|
| 9. |
Scalvenzi M, Palmisano F, Cacciapuoti S, Migliaro F, Siano M, Staibano S, et al. Giant congenital melanocytic naevus with proliferative nodules mimicking congenital malignant melanoma: A case report and review of the literature of congenital melanoma. Case Rep Dermatol Med 2013;2013:473635.
[Google Scholar]
|
| 10. |
Rose C, Kaddu S, El-Sherif TF, Kerl H. A distinctive type of widespread congenital melanocytic nevus with large nodules. J Am Acad Dermatol 2003;49:732-5.
[Google Scholar]
|
Fulltext Views
4,345
PDF downloads
2,067





