Translate this page into:
Intertriginous bullous morphea: A clue for the pathogenesis?
2 Department of Pathology, Istanbul University Cerrahpasa Medical School, Istanbul, Turkey
Correspondence Address:
Ilkin Zindanci
Goztepe Egitim Hastanesi Dermatoloji Klinigi Kadikoy, Istanbul
Turkey
| How to cite this article: Kavala M, Zindanci I, Demirkesen C, Beyhan ES, Turkoglu Z. Intertriginous bullous morphea: A clue for the pathogenesis?. Indian J Dermatol Venereol Leprol 2007;73:262-264 |
Abstract
Bullae occurring in lesions of morphea are uncommon. The cause of bullae formation in morphea is multifactorial, although lymphatic obstruction from the sclerodermatous process is considered the likeliest cause. Bullous morphea may be confused clinically with lichen sclerosus et atrophicus since both diseases may cause bullae in sclerodermatous plaques. A 69-year-old woman presented with a history of generalized morphea diagnosed 9 years earlier; and a 1-month history of pruritic bullae on her inframammary folds, axillary regions, lower abdomen, upper extremities and inguinal folds. Physical examination revealed multiple erythematous erosions, hemorrhagic vesicles and eroded bullae with slight scale or crusts overlying hypopigmented, indurated, shiny plaques. Skin biopsy revealed prominent edema in the papillary dermis, resulting in bulla formation and thickening of collagen fibers within the dermis. Direct immunofluorescence was negative. According to histologic and clinical features, the diagnosis of bullous morphea was established.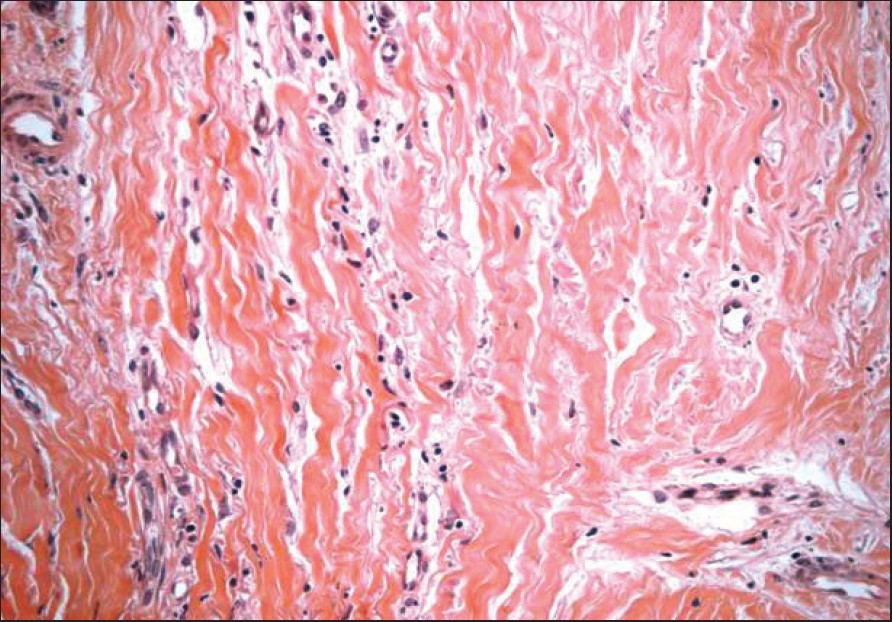 |
| Figure 4: Coarse, eosinophilic collagen fibers lying parallel under the epidermis (H and E, x200) |
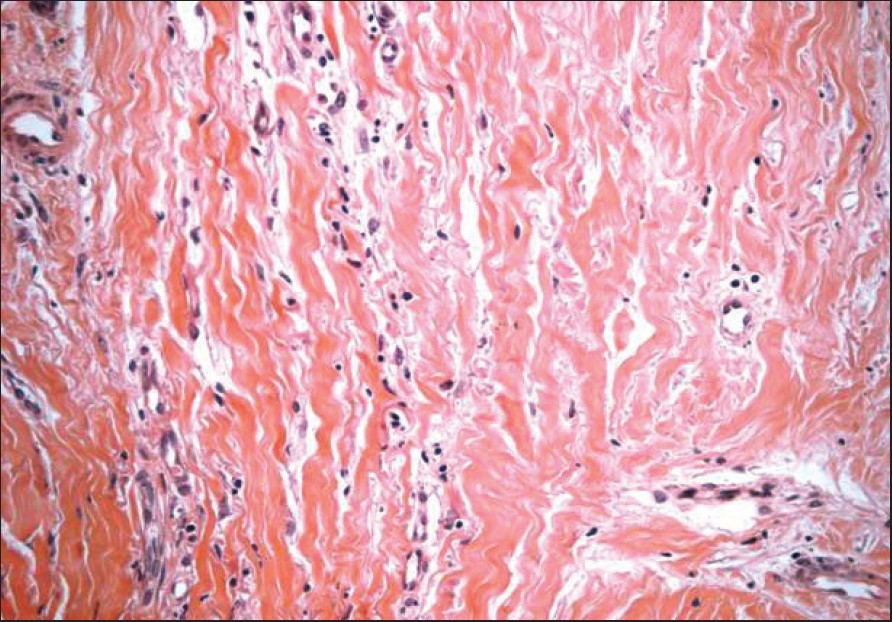 |
| Figure 4: Coarse, eosinophilic collagen fibers lying parallel under the epidermis (H and E, x200) |
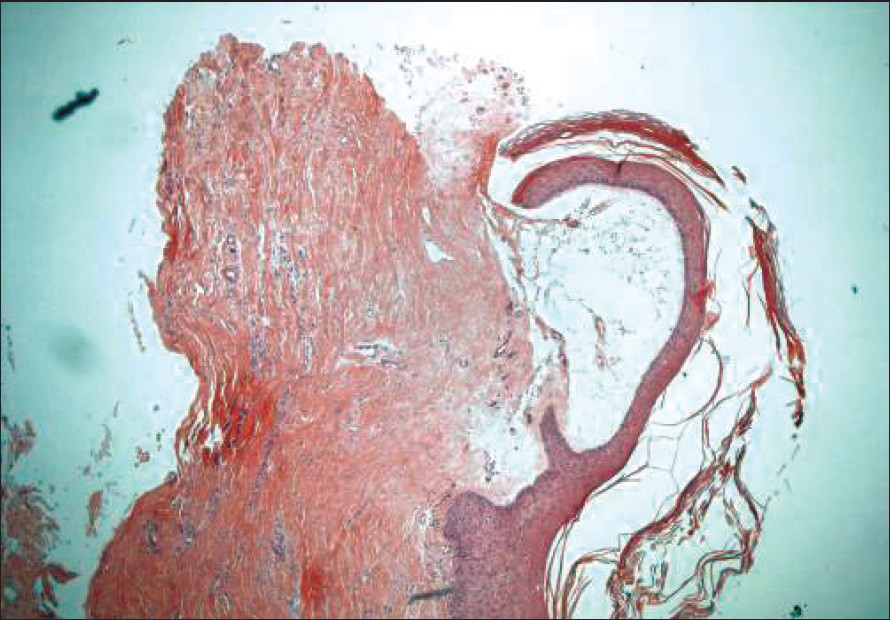 |
| Figure 3: A subepidermal blister is formed on the surface (H and E, x40) |
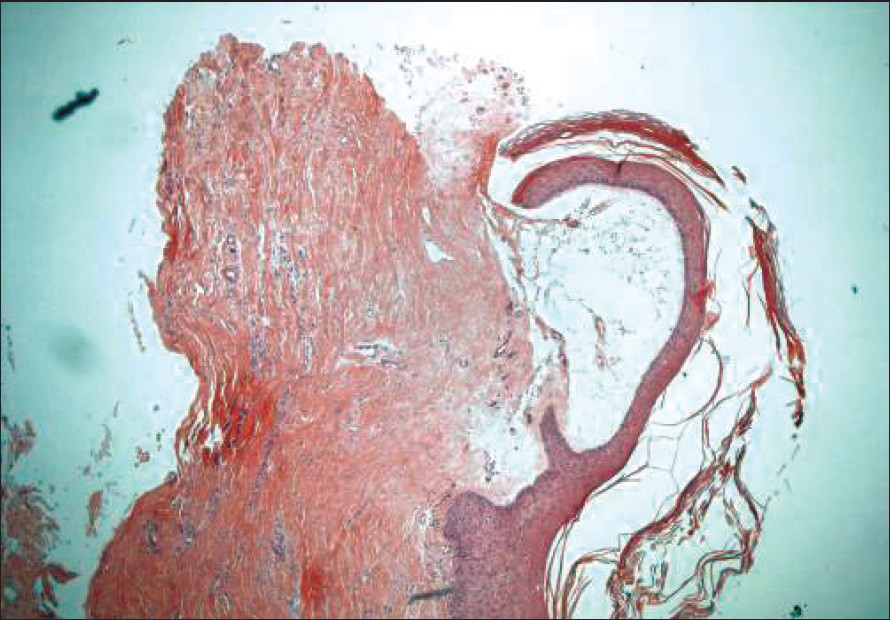 |
| Figure 3: A subepidermal blister is formed on the surface (H and E, x40) |
 |
| Figure 2: Closer view of the tense, shiny skin underlying the vesicles and bullae |
 |
| Figure 2: Closer view of the tense, shiny skin underlying the vesicles and bullae |
 |
| Figure 1: Eroded and crusted bullae overlying the morpheic plaques on the inframammarian and inguinal skin |
 |
| Figure 1: Eroded and crusted bullae overlying the morpheic plaques on the inframammarian and inguinal skin |
Introduction
Bullae occurring in lesions of morphea are uncommon, and the lower extremities are the most common sites of involvement. [1],[2] The cause of bullae formation in morphea is multifactorial [2] ; lymphatic obstruction from the sclerodermatous process is considered the likeliest cause. [3],[4] Bullous morphea may be confused clinically with lichen sclerosus et atrophicus since both diseases may cause bullae in sclerodermatous plaques. [5],[6]
Case Report
A 69-year-old woman presented with a history of generalized morphea diagnosed 9 years earlier; and a 1-month history of pruritic bullae on her inframammarian folds, axillary regions, lower abdomen, upper extremities and inguinal folds. The patient had no Raynaud′s phenomenon, dyspnea or dysphagia. Her current medication included moderate-strength topical steroid creams for the lesions. Physical examination revealed multiple erythematous erosions, hemorrhagic vesicles and eroded bullae with slight scale or crusts overlying hypopigmented, indurated, shiny plaques [Figure - 1],[Figure - 2]. There were no facial telangiectasias or sclerodactyly. Blood count, erythrocyte sedimentation rate, creatinine, liver function tests and serum immunoglobulins were normal except 10% peripheral blood eosinophilia. ANA, anti-Ro, anti-La, Sm, dsDNA, Scl-70 and Borrelia antibody tests were negative. Serum protein electrophoresis increased in gamma-globulin fraction (23.5%; normal: 12-20%).
In skin biopsy, there was a prominent edema in the papillary dermis, resulting in bulla formation [Figure - 3]. Collagen fibers within the dermis were thickened and had an eosinophilic, homogenous appearance. The skin appendages were entrapped within the coarse collagen bundles and were seen atrophic [Figure - 4]. Direct immunofluorescence was negative. According to histologic and clinical features, the diagnosis of bullous morphea was established.
Discussion
The existence of bullous lesions in morphea or systemic scleroderma is rare [1] and has been reported infrequently. [2],[5],[7],[8] Lichen sclerosus et atrophicus (LSA), in which the clinical features are confused with morphea, [6] also forms bullae in the patches. [9] The presence of bullae in LSA is more frequent than in morphea and has a hemorrhagic component. [10] In the literature, there are conflicting reports about the nature and very existence of bullous morphea. Some authors have suggested that there is a close relationship between LSA and morphea, [11],[12] while others considered it as different manifestations of a single disease spectrum. [13],[14] However, Patterson and Ackerman [15] emphasized that the two conditions were entirely separate.
Indeed, the histologic appearances of both diseases differ from each other. The epidermis in morphea shows neither hydropic degeneration of the basal cells nor follicular plugging, and the upper dermis in morphea has elastic fibers and shows no zone of edema. Reticular dermal changes of fibrosis and inflammation of morphea contrast with edema and loss of elastic tissue in LSA. [16]
The etiology of bullous morphea is not certain, and there are several theories to explain the mechanism. Bullae formation was attributed to lymphedema caused by dilated lymphatic vessels, which occurs as a result of lymphatic obstruction from the sclerodermatous process. [3],[4] The tendency for bullae to form on the lower extremities also suggests that lymphatic obstruction, combined with increased hydrostatic pressure, leads to bullae. [2] Pautrier [17] also suggested that vascular changes like arteritis and phlebosclerosis play a role in bullae formation. Our patient had neither dilated lymphatic vessels nor vascular changes histologically. Su and Grene [18] described a patient with bullous morphea profunda whose biopsy showed no lymphatic obstruction, arteritis or phlebitis. O′Leary [19] found a correlation between local trauma and bullae formation. Dauod et al. [2] showed the eosinophil granule component major basic protein (MBP) in the base of morphea bullae and suggested that eosinophils and, particularly, MBP may contribute to tissue destruction and bullae formation in some patients. Previous papers have reported increased peripheral blood eosinophils and tissue eosinophilia in patients with morphea profunda and bullous morphea. [2],[20] Our case had significant peripheral eosinophilia but had no eosinophils in cutaneous tissue. The predilection of the intertriginous regions suggested the role of local trauma and friction as the precipitating factors of bullae formation.
Treatment of bullous morphea is unsatisfactory. It is suggested that salazopyrin has some efficacy. [21] Daoud et al. [2] found variable success with topical triamcinolone and hydroxychloroquine, 200 mg daily, but no improvement despite treatment with D-penicillamine, prednisone, cyclosporine, dapsone, minocycline, topical steroids, penicillin, cyclophosphamide and phenytoin. Since our patient refused systemic therapy, treatment was begun using a potent topical steroid cream. After 6 weeks, the blisters improved while the sclerotic patches persisted.
We conclude that as O′Leary had suggested before, the exact nature of blister formation on morphea lesions is due to friction, which becomes evident in the intertriginous regions of the body.
| 1. |
Odom RB, James WD, Berger TG. Connective tissue diseases. In : Odom RB, James WD, Berger TG, editors. Andrews' disease of the skin. Clinical dermatology. 9 th ed. WB Saunders Company: Philadelphia; 2000. p. 191-200.
th ed. WB Saunders Company: Philadelphia; 2000. p. 191-200.'>[Google Scholar]
|
| 2. |
Daoud MS, Su WP, Leiferman KM, Perniciaro C. Bullous morphea: Clinical, pathological and immunopathologic evaluation of thirteen cases. J Am Acad Dermatol 1994;30:937-43.
[Google Scholar]
|
| 3. |
Synkowski DR, Lobitz WC Jr, Provost TT. Bullous scleroderma. Arch Dermatol 1981;117:135-7.
[Google Scholar]
|
| 4. |
Tuffanelli DL. Lymphangiectasis due to scleroderma. Arch Dermatol 1975;111:1216.
[Google Scholar]
|
| 5. |
Kobayasi T, Willeberg A, Serup J, Ullman S. Generalized morphea with blisters. A case report. Acta Derm Venereol 1990;70:454-6.
[Google Scholar]
|
| 6. |
DeFeo CP. Bullous lichen sclerosus et atrophicus vs scleroderma. Arch Dermatol 1967;95:238-9.
[Google Scholar]
|
| 7. |
Trattner A, David M, Sandbank M. Bullous morphea: A distinct entity? Am J Dermatopathol 1994;16:414-7.
[Google Scholar]
|
| 8. |
Rencic A, Goyal S, Mofid M, Wigley F, Nousari HC. Bullous lesions in scleroderma. Int J Dermatol 2002;541:335-9.
[Google Scholar]
|
| 9. |
Hallel-Halevy D, Grunwald MH, Yerushalmi J, Halevy S. Bullous lichen sclerosus et atrophicus. J Am Acad Dermatol 1998;39:500-1.
[Google Scholar]
|
| 10. |
Tudino ME, Wong AK. Bullous lichen sclerosus et atrophicus on the palms and wrists. Cutis 1984;33:475-6.
[Google Scholar]
|
| 11. |
Jablonska S. Lichen sclerosos et atrophicus and its relation to localized scleroderma. In : Jablonska S, editors. Scleroderma and pseudoscleroderma. 2 nd ed. Polish Medical Publishers: Warsaw, Poland; 1975. p. 566-79.
[Google Scholar]
|
| 12. |
Uitto J, Santa Cruz DJ, Bauer EA, Eisen AZ. Morphea and lichen sclerosus et atrophicus. Clinical and histopathologic studies in patients with combined features. J Am Acad Dermatol 1980;3:271-9.
[Google Scholar]
|
| 13. |
Connelly MG, Winkelmann RK. Coexistence of lichen sclerosus, morphea and lichen planus. Report of four cases and review of the literature. J Am Acad Dermatol 1985;12:844-51.
[Google Scholar]
|
| 14. |
Dalziel K, Reynolds AJ, Holt PJ. Lichen sclerosus et atrophicus with ocular and maxillary complications. Br J Dermatol 1987;116:735-7.
[Google Scholar]
|
| 15. |
Patterson JA, Ackerman AB. Lichen sclerosus et atrophicus is not related to morphea. A clinical and histologic study of 24 patients in whom both conditions were reputed to be present simultaneously. Am J Dermatopathol 1984;6:323-35.
[Google Scholar]
|
| 16. |
Jaworsky C. Connective tissue diseases. In : Elder D, Elenitsas R, Jaworsky C, Johnson B, editors. Lever's histopathology of the skin. 8 th ed. Lippincott-Raven publishers: Philadelphia; 1997. p. 274-8.
th ed. Lippincott-Raven publishers: Philadelphia; 1997. p. 274-8. '>[Google Scholar]
|
| 17. |
Pautrier LM. Sclerodermie a evolution rapide, en plaques multiples. �mportance des lesions vascularies initiales et tardives dans l'etude de la sclerodermie. Bull Soc Fr Dermatol 1929;36:928-38.
[Google Scholar]
|
| 18. |
Su WP, Greene SL. Su WP, Greene SL. Am J Dermatopathol 1986;8:144-7.
[Google Scholar]
|
| 19. |
O'Leary PA. In discussion on morphea. Arch Dermatol Syphilol 1954;70:387-8.
[Google Scholar]
|
| 20. |
Peters MS, Su WP. Eosinophils in lupus panniculitis and morphea profunda. J Cutan Pathol 1991;18:189-92.
[Google Scholar]
|
| 21. |
Micalizzi C, Parodi A, Rebora A. Generalized bullous morphoea. Efficacy of salazopyrin. Clin Exp Dermatol 1996;21:246-7.
[Google Scholar]
|
Fulltext Views
3,641
PDF downloads
2,422





