Translate this page into:
Intriguing plaque on the glans penis of a young man
Corresponding author: Dr. Rishabh Singhal, Department of Dermatology, Krishna Vishwa Vidyapeeth, KVV, Malkapur, Karad, District Satara, India. rishabhsinghal30@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Singhal R, Nikam BP, Kale MS, Jamale VP. Intriguing plaque on the glans penis of a young man. Indian J Dermatol Venereol Leprol. 2024;90:388-89. doi: 10.25259/IJDVL_508_2023
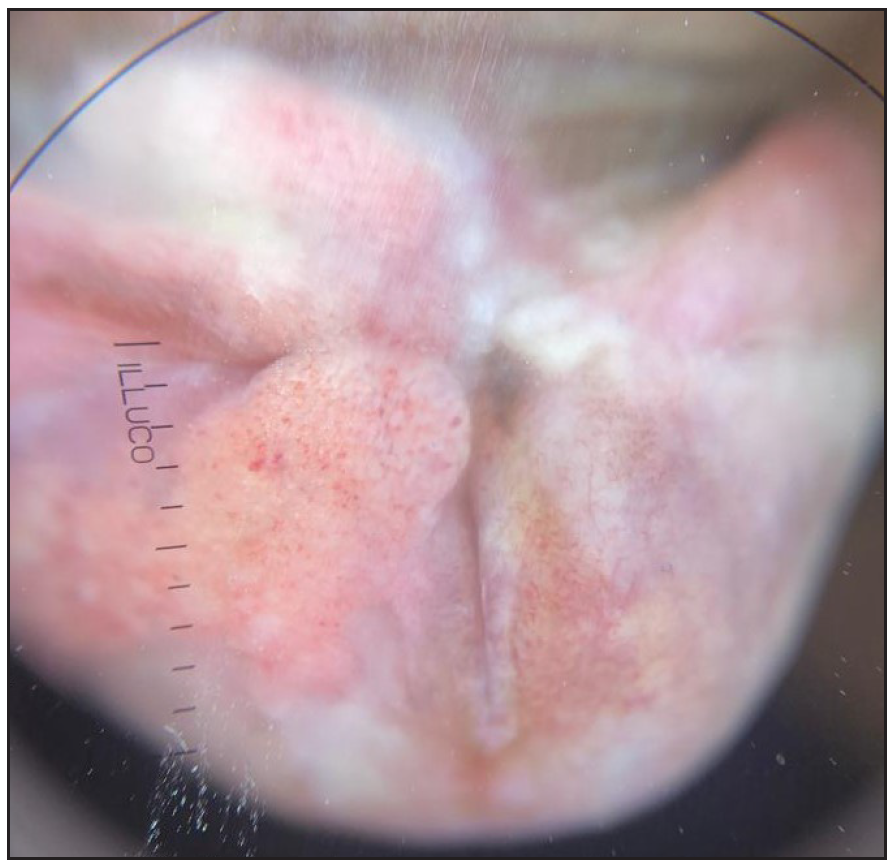
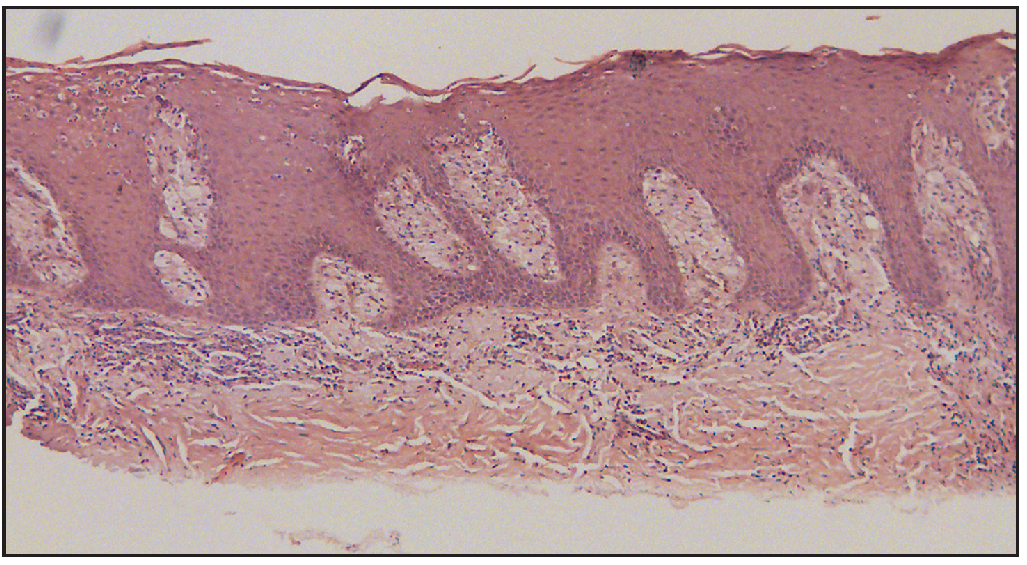
A 19-year-old man presented with a solitary, irregularly raised lesion on the glans penis, extending to the frenulum. It started as an erythematous papule, which slowly progressed to the present size of approximately 2 × 3cm over a period of 2 months. On examination, there was a solitary erythematous plaque with a verrucous surface [Figure 1] that was non-tender and non-itchy. There was no history of sexual exposure. Dermoscopy showed a whitish area with a pinkish red background, hairpin vessels and some yellow areas [Figure 2]. Routine hematological and biochemical investigations were all within normal limits. VDRL, HIV, HBsAg and HCV tests were also non-reactive. The histopathology of the lesion has been depicted in Figures 3a and 3b.

- Irregularly raised pinkish red plaque on the ventral aspect of glans penis
- Prominent pinhead vessels over a yellowish base seen on gently placing the dermoscope
- Epidermal hyperplasia (H&E, 100X)
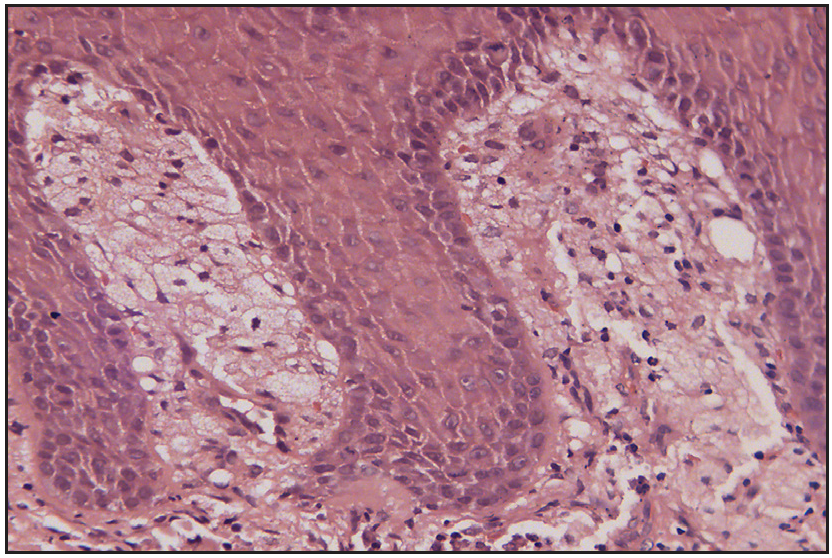
- Multiple foamy histiocytes present within the dermal papillae (H&E, 400X)
Question
What is your diagnosis?
Answer
Verruciform genital-associated xanthoma
Discussion
Verruciform xanthoma (VX) is a warty or cauliflower-like benign lesion, usually occurring in the oral mucosa. It is typically asymptomatic and ranges in size from 2 mm to 1.5 cm with a normal/pale/white/red colour.1
Very few cases of VX occurring extra orally have been reported. The penis, scrotum and vulva are some sites where extraoral lesions have been reported. VX in genital locations has recently been referred to as verruciform genital associated (VeGAs) xanthomas.2 Kraemer et al reported the first case of VeGAs xanthoma in 1981. There has been a male preponderance in the cases of VeGAs xanthomas. To date, only 33 cases of verruciform xanthoma on the penis have been reported.3 The age of onset of the lesions ranged from 8 to 85 years, with a mean of 54.5 years. Some of the common differential diagnoses of verruciform genital-associated xanthoma include erythroplasia of Queyrat, leukoplakia going into lichen sclerosus, verrucous carcinoma, verruca simplex and condyloma acuminata.2
Extraoral lesions are frequently associated with other conditions such as lymphedema, epidermal nevi, congenital hemidysplasia with ichthyosiform erythroderma and limb defects syndrome.3
The exact etiopathogenesis of verruciform xanthoma remains elusive even today. Some of the potential etiologic reasons for verruciform xanthoma include local trauma, persistent inflammation, candida infection and cancer in situ.3
The most widely recognised explanation proposes that macrophages with CCR2 molecules are recruited by activated T-lymphocytes brought on by chronic inflammation, and that this upregulates the expression of macrophage scavenger receptor on them. The low-density lipoproteins from the epithelial cells are recognised by these macrophages, which then capture, internalise and oxidise them to produce foam cells.3 The absence of human papilloma virus in in situ hybridisation findings recently has ruled out viral etiology for these lesions.3
Dermoscopy typically shows pinhead blood vessels over a yellowish base with a whitish rim when placing the dermoscope gently over the lesion. However, upon increasing the pressure, there’s reduction in the pinhead vessels with concomitant enhancement of the areas.4 This feature has been described as characteristically associated with verruciform genital associated xanthoma.
The final diagnosis of verruciform xanthoma is made on histopathological examination. Acanthotic epidermis, uniformly elongated rete ridges and foamy histiocytes throughout the dermal papillae are the features characteristically associated with VX. The foam cells exhibit CD68 antigen and p positivity, indicating the presence of glycogen granules in cells of the monocyte–macrophage lineage.2 S100, CK8, CK19, CK14 and pan keratin have been noted to stain negatively for the xanthoma cells.5
The treatment of the VX lesion involves local surgical excision, which is almost always curative without recurrence.5 Imiquimod, an imidazoquinolinone, has potent anti-viral and anti-tumour activity and has shown a good response in one case of verruciform genital-associated xanthoma. The current case was treated with imiquimod 5% cream every alternate day. However, he developed ulceration and imiquimod was stopped. He then underwent surgical excision that led to complete resolution of the lesion.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using the AI.
References
- Verruciform xanthoma: A view on the concepts of its etiopathogenesis. J Oral MaxillofacPathol. 2013;17:392.
- [Google Scholar]
- Vegas (verruciform genital-associated) xanthoma: A comprehensive literature review. Dermatol Ther (Heidelb). 2017;7:65-79.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Verruciform xanthoma of the penis: A rare case with an unusual clinical morphology. Indian J Dermatol VenereolLeprol. 2018;84:600.
- [Google Scholar]
- Verruciform xanthoma: Report of three patients with comparative dermoscopic study. Clin Exp Dermatol. 2015;40:156-9.
- [CrossRef] [PubMed] [Google Scholar]
- Rare case of large verrucous xanthoma of oral cavity managed with nasolabial flap and review of literature. Oral Maxillofac Surg Cases. 2020;6:100170.
- [Google Scholar]





