Translate this page into:
Involvement of scars in capecitabine induced hand foot syndrome
2 Department of pathology, Prolife Diagnostics, Bhubaneswar, Odisha, India
Correspondence Address:
Bhabani S. T. P. Singh
Palm Heights, A 706, Kalinga Nagar, Bhubaneswar - 751 003, Odisha
India
| How to cite this article: Singh BS, Tripathy T, Kar BR, Singh S. Involvement of scars in capecitabine induced hand foot syndrome. Indian J Dermatol Venereol Leprol 2018;84:85-87 |
Sir,
Hand foot syndrome (HFS) is a cutaneous toxic reaction to several chemotherapeutic drugs, and is characterized by symmetrically distributed erythema, edema with or without blisters, and erosions over palms and soles. Most common drugs implicated are pegylated doxorubicin, capecitabine, 5 fluorouracil, cytarabine, docetaxel, sorafenib, and sunitinib, etc.[1],[2] Involvement of atypical sites such as the scrotum and penis have been reported in the literature.[3] Here, we report a case of capecitabine-induced HFS involving old scars in addition to the classical sites. We were unable to find any previous reports of scar involvement in HFS.
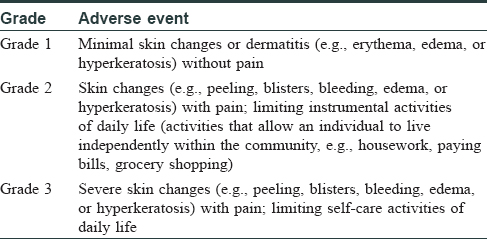
A 52-year-old woman of type IV skin with metastatic intrahepatic cholangiocarcinoma was referred to the dermatology department of the Institute of Medical Sciences and SUM hospital for hyperpigmentation on her palms and soles for 10 days. She had received eight cycles of gemcitabine and oxaliplatin. This period was uneventful from the dermatological perspective. However, due to disease progression, the patient was administered a regimen of capecitabine (850 mg/m2) and irinotecan (topoisomerase I inhibitor) (180 mg/m2). Five days after receiving the second cycle of irinotecan and capecitabine, she noticed sudden onset of painful erythema over her palms and soles following a prodrome of tingling sensation. Over the next 5 days, the erythema turned into hyperpigmentation with blistering on finger tips and toes. The pain was severe enough to limit the patient from carrying out self-care activities. Simultaneously, two old atrophic scars on the patient's left arm showed similar changes as that of the palm and sole with painful tingling sensation followed by erythema and hyperpigmentation. Her medical history was unremarkable. There was no history of any topical application, relief on cooling, any constitutional features, or bone marrow transplantation in the past. No similar episodes were present following exposure to any medications. On cutaneous examination, there was well-demarcated tender erythema to hyperpigmentation over convex areas of palm and soles with desquamation at the tips [Figure - 1]. Similar changes were present confined to two 2 × 2 cm atrophic scars over the left arm [Figure - 2]. Mucosae and nail were normal. Systemic examination did not reveal any abnormalities. Complete blood count showed thrombocytopenia with platelet count of 50,000/μl. From history and clinical findings, a diagnosis of grade 3 HFS caused by capecitabine was made as per the National Cancer Institute criteria [Table - 1].[4] Biopsy from the scar site revealed vacuolar degeneration of the basal layer and increased melanocytes in the epidermis consistent with HFS [Figure - 3]. Capecitabine was stopped followed by gradual resolution of the lesions over a period of 4 weeks.
 |
| Figure 1a: Hyperpigmentation on palms with desquamation at tips |
 |
| Figure 1b: Hyperpigmentation on soles with desquamation at tips |
 |
| Figure 2: Hyperpigmentation confined to scar site |
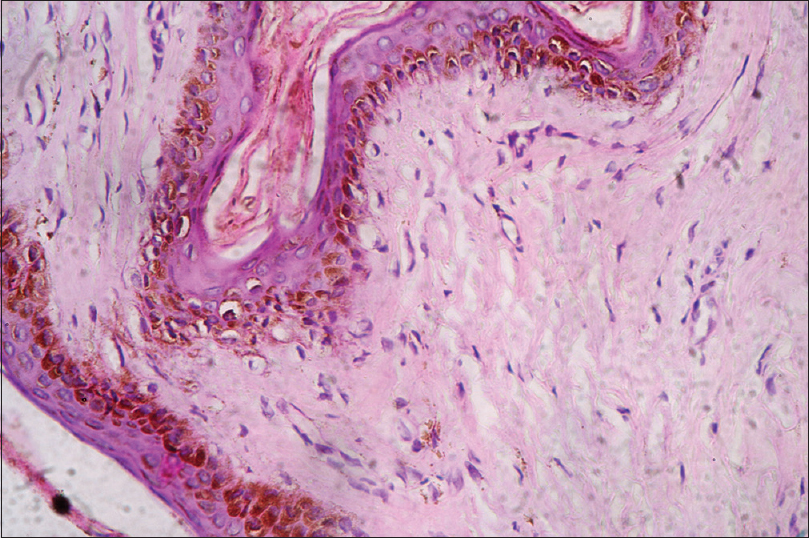 |
| Figure 3: Focal vacuolar degeneration of basal layer with increased epidermal melanocytes and melanin drop out into dermis. (H and E, ×40) |
HFS or palmoplantar dysesthesia was first reported in 1974 to be caused by mitotane (adrenal cytotoxic agent). HFS is seen in more than 50% of patients receiving capecitabine.[1] Epidermis shows scattered necrotic keratinocytes with basal layer vacuolar degeneration. Severe lesions can also have full thickness epidermal necrosis. There are various theories explaining the pathogenesis of HFS. The chemotherapeutic drugs secreted through sweat ducts accumulate and cause local direct damage to the keratinocytes. This theory explains the localization of the cutaneous changes to the hands and feet.[5] Some hypothesize increased expression of metabolizing enzyme thymidine phosphorylase that converts capecitabine to 5 fluorouracil and increases toxic injury to the tissue.[5] According to some authors, inflammation due to chemotherapy induced overexpression of cyclooxygenase 2 and capillary damage due to mechanical pressure on the hands and feet contribute to the pathogenesis of this entity.[5]
The index case had two atrophic scars possibly from Bacillus Calmette Guerin and small pox vaccination, showing features consistent with HFS. There was a prodrome of burning pain with sharply demarcated erythema confined to the scar site. Subsequent hyperpigmentation and desquamation occurred in coherence with the palms and soles. This finding raises questions about the established theories of pathogenesis and warrants further research. Scarring causes loss of sweat ducts, thereby ruling out the possibility of direct tissue damage caused by chemotherapeutics secreted through sweat. Compromised capillary circulation in scars could be one possible hypothesis. Whether scar tissues express excess thymidine phosphorylase needs to be studied.
We propose that scars need to be examined as a supportive evidence to HFS. Whether scar involvement in HFS categorizes the patient into higher grade of severity, as seen in our case, also needs large scale studies.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient has given her consent for her images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Degen A, Alter M, Schenck F, Satzger I, Völker B, Kapp A, et al. The hand-foot-syndrome associated with medical tumor therapy-Classification and management. J Dtsch Dermatol Ges 2010;8:652-61.
[Google Scholar]
|
| 2. |
Lal HS. Hand and foot syndrome secondary to capecitabine. Indian J Dermatol Venereol Leprol 2014;80:427-30.
[Google Scholar]
|
| 3. |
Lee YJ, Lee HJ, Jeong KC, Kang JG, Lee SH, Kim YT, et al. An unusual presentation of hand-foot syndrome at the hidden area: The scrotum and penis. Acta Oncol 2009;48:636-7.
[Google Scholar]
|
| 4. |
Common Terminology Criteria for Adverse Events (CTCAE) Vers. 4.0, NCI, NIH, USDHHS, Washington, DC. Available from: https://www.eortc.be/services/doc/ctc/CTCAE_4.03_2010-06-14_QuickReference_5x7.pdf. [Last updated on 2009 May 28; Last accessed on 2017 Mar 16].
[Google Scholar]
|
| 5. |
Clark AS, Vahdat LT. Chemotherapy-induced palmar-plantar erythrodysesthesia syndrome: Etiology and emerging therapies. Support Cancer Ther 2004;1:213-8.
[Google Scholar]
|
Fulltext Views
2,763
PDF downloads
1,434





