Translate this page into:
Ipsilateral facial paralysis and steroid acne
Corresponding Author:
Berna Aksoy
Dermatology Clinic, VM Medical Park Hospital, Ovacik Discrete, Beside D-100 Highway, No. 36, Başiskele, Kocaeli
Turkey
bmaksoy@mynet.com
| How to cite this article: Aksoy B. Ipsilateral facial paralysis and steroid acne. Indian J Dermatol Venereol Leprol 2017;83:376-378 |
Sir,
Steroid acne is a form of acneiform eruption observed after topical or oral administration of steroids.
A 26-year-old man reported to our clinic with acne, localized to the right half of his face of three months' duration. His medical history revealed that he had suffered from Bell's palsy four months back. He had been treated with vitamin pills and intramuscular injections of dexamethasone 8 mg once daily for 20 days. His facial paralysis improved; however, a month later he developed acne on his face. On dermatological examination, he had widespread comedones, papules and nodules mainly on the right side of the face. He also had mild right facial paresis. He was diagnosed to have steroid acne, localized to the paralyzed side of the face [Figure - 1],[Figure - 2],[Figure - 3]. He was treated with topical isotretinoin gel, erythromycin - benzoyl peroxide combined gel and oral tetracycline. The acne resolved completely after 2 months.
 |
| Figure 1: Severe acne lesions are localized mainly on the right side of the face, that was previously paralyzed (Case 1) |
 |
| Figure 2: In frontal view, acne lesions are seen to be mainly localized on the right side of the face (Case 1) |
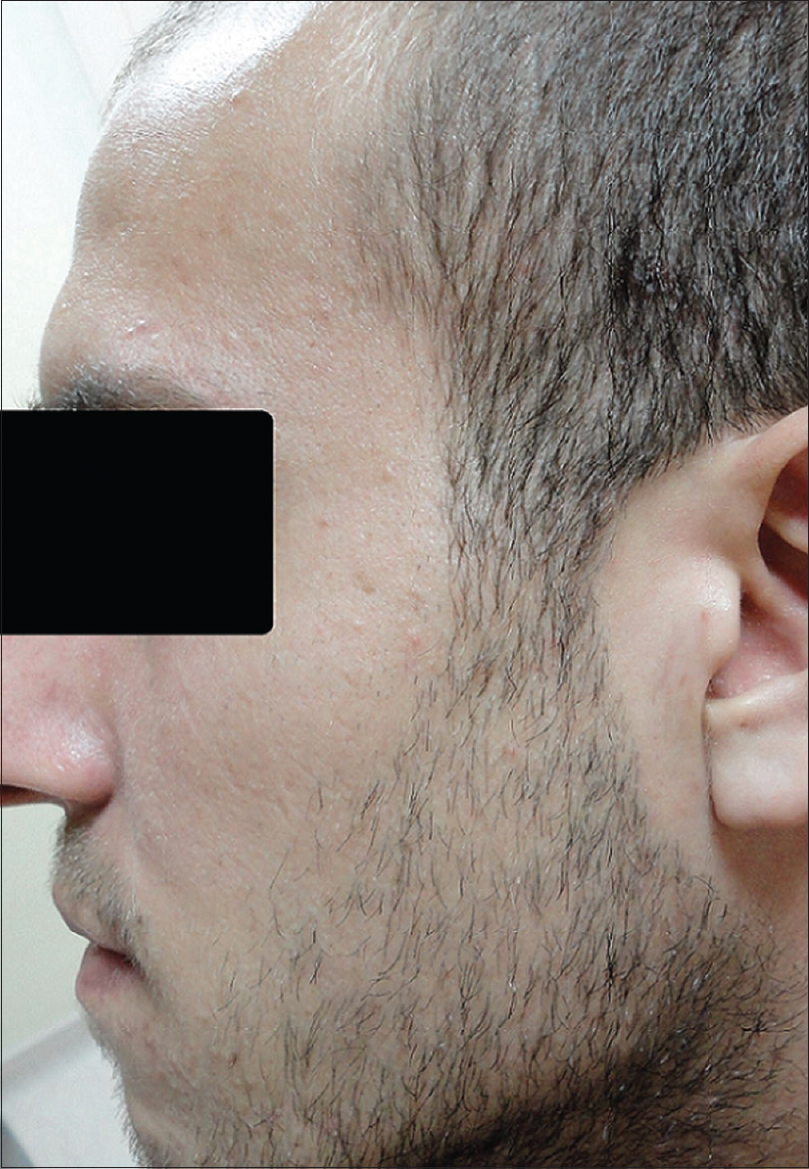 |
| Figure 3: Minimal acne lesions are localized on the other side of the face (Case 1) |
A 31-year-old lady reported with hemi-facial acne, located on the right side of the face, of 5 months ' duration. Her history revealed that she was a hepatitis B carrier and had developed Bell's palsy involving the same side of her face, 6 months ago. She had been treated with oral methylprednisolone 24 mg daily for a month. Her facial paralysis improved; but a month later she developed acne. On dermatological examination, she had papules and erythematous macules mainly on the right side of the face. She was diagnosed to have steroid acne localized to the paralyzed side of the face [Figure - 4],[Figure - 5],[Figure - 6]. She was successfully treated with topical isotretinoin gel and metronidazole cream.
 |
| Figure 4: Acne lesions are seen to be localized mainly on the right side of the face, that was previously paralyzed (Case 2) |
 |
| Figure 5: Frontal view shows acne lesions located on forehead and the right cheek (Case 2) |
 |
| Figure 6: Minimal acne lesions are localized on the left side of the face (Case 2) |
There are previous reports of patients developing acne on the paralysed half of the face.[1],[2] In one case, the eruption developed about 1 month after the commencement of oral steroid therapy for the treatment of facial paralysis, as was the case in our patient.[2] The author tested urinary excretion of 17-hydroxy corticosteroids and 17-ketosteroids and found no abnormality.[2] It was confirmed clinically that the skin colored papules on the face of the patient were closed comedones; and the histologic features were typical of an epidermal cyst.[2] The lesions healed after 6 months of oral minocycline treatment.[2] Burton et al. found that there is mild increase in the excretion of sebum on the paralyzed side of patients with unilateral facial nerve paralysis; however, the difference was not statistically significant when compared with the normal side.[3] They reported a case with acne lesions on the paretic side of forehead and found that sebum excretion rate of paretic side was 1.87 times higher compared to normal side.[3]
Human sebaceous glands are not innervated and thus show function independently of nerve supply. Researchers have been unable to detect any effects of denervation or nerve stimulation on the sebaceous gland.[3] As far as the cheeks and forehead region are concerned, facial nerve fibers innervate superficial facial musculature located deep to the skin. However, sebaceous glands are located in the skin. Hence, neuro-humoral changes associated with loss of facial nerve function cannot affect the sebaceous glands anatomically.
It was previously hypothesized that the lack of muscular movement on the paralyzed side causes a random outflow of sebum, and possibly decreases the local skin temperature.[2] In addition, oral steroids given for facial paralysis makes the follicular epithelium more vulnerable to comedogenic substances in the sebum in acne prone patients.[2],[4] All these factors were proposed to lead to the development of acne on the paralyzed side of the face.[2] Yu et al. showed that steroid acne was actually a form of Pityrosporum folliculitis and it shows good response to oral antifungal treatment.[5]
Both the patients in this report declared that they did not apply any known comedogenic substances to massage the paralyzed side of the face. The effect of systemic immunosuppression and the priming of the follicular epithelium by oral steroids may lead to the overgrowth of Pityrosporum ovale, mainly in the skin of paralyzed side of the face of predisposed individuals. Sebum excretion changes (random outflow, stasis and increased viscosity as a result of decreased local temperature) resulting from the loss of mobility due to facial paralysis may contribute to the overgrowth of lipophilic Pityrosporum fungi. All these pathogenetic factors result in the development of Pityrosporum folliculitis and this manifests itself as steroid acne clinically. It is thought that this is the probable etiopathogenetic mechanism that explains the development of steroid acne affecting mainly the paralyzed side of the face.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient(s) have given their consent for their images and other clinical information to be reported in the journal. The patients understand their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. | Nexmand PH. A case of seborrhea with comedones in conjunction with facial paralysis. Acta Dermatovenerol 1944;25:275-81. [Google Scholar] |
| 2. | Tagami H. Unilateral steroid acne on the paralyzed side of the face. J Dermatol 1983;10:281-2. [Google Scholar] |
| 3. | Burton JL, Cunliffe WJ, Saunders IG, Shuster S. The effect of facial nerve paresis on sebum excretion. Br J Dermatol 1971;84:135-8. [Google Scholar] |
| 4. | Kaidbey KH, Kligman AM. The pathogenesis of topical steroid acne. J Invest Dermatol 1974;62:31-6. [Google Scholar] |
| 5. | Yu HJ, Lee SK, Son SJ, Kim YS, Yang HY, Kim JH. Steroid acne vs. Pityrosporum folliculitis: The incidence of Pityrosporum ovale and the effect of antifungal drugs in steroid acne. Int J Dermatol 1998;37:772-7. [Google Scholar] |
Fulltext Views
7,790
PDF downloads
2,031





