Translate this page into:
Is cyclosporine a good option for the treatment of subcutaneous panniculitis-like T-cell lymphoma associated with hemophagocytic syndrome?
2 Department of Pathology, Hospital Universitario 12 de Octubre, Instituto de Investigacion I + 12, Universidad Complutense, Madrid, Spain
Correspondence Address:
Raquel Arag�n-Miguel
Avenida de Cordoba S/N, Madrid
Spain
| How to cite this article: Arag�n-Miguel R, Calleja-Algarra A, Velasco-Tamariz V, Garrido M, Ortiz-Romero P, Maro�as-Jim�nez L. Is cyclosporine a good option for the treatment of subcutaneous panniculitis-like T-cell lymphoma associated with hemophagocytic syndrome?. Indian J Dermatol Venereol Leprol 2019;85:656-659 |
Sir,
Subcutaneous panniculitis-like T-cell lymphoma is a rare mature T-cell lymphoma which generally has an indolent clinical behavior. But sometimes it may be associated with hemophagocytic syndrome which leads to a rapidly progressive course.[1] We report a patient with subcutaneous panniculitis-like T-cell lymphoma and secondary hemophagocytic syndrome who responded successfully to oral cyclosporine.
A 26-year-old woman from the Philippines presented with painful, nodular lesions of size ranging from 1 to 3 cm on her limbs, abdomen, and lower back of one month duration. [Figure - 1]a and [Figure - 1]b.
 |
| Figure 1: |
She had associated high-grade fever and myalgia but no other symptoms like arthralgia. Laboratory tests showed abnormal liver function with elevated aspartate aminotransferase, gamma-glutamyltransferase, alkaline phosphatase, lactate dehydrogenase, and ferritin. Her CD25 was 3588 pg/mL (normal range: 0–1900 pg/mL). Investigations revealed mild anemia, leukopenia, and lymphopenia. An infectious origin was ruled out by performing urine, sputum, stool and blood culture, tuberculin test, tests for antibodies against HBV, HCV, HIV, syphilis, CMV, measles, and EBV in serum, chest and sacroiliac x-ray, and computed tomography scan of chest, abdomen and pelvis. Histopathological examination revealed a dense infiltrate of pleomorphic lymphoid cells with large nuclei and lymphocytoclasia around the adipocytes. There were no pathological changes in dermis and epidermis [Figure - 1]c and [Figure - 1]d. Lymphocytes expressed CD3, CD8, perforin, and granzyme but not TIA 1 or CD4 [Figure - 1]e, [Figure - 1]f, [Figure - 1]g, [Figure - 1]h. Both histopathological and immunohistochemical findings were consistent with subcutaneous panniculitis-like T-cell lymphoma. Bone marrow aspiration cytology showed an increase in the phagocytic mononuclear system with evidence of hemophagocytosis. 18 F-fluorodeoxyglucose positron emission tomography/computed tomography highlighted multiple pathological and generalized uptakes especially over the limbs, abdominal wall, and right breast. Ultrasonography showed splenomegaly. A final diagnosis of subcutaneous panniculitis-like T-cell lymphoma with hemophagocytic syndrome was made and the patient was started on oral dexamethasone 12 mg daily. Clinical and biochemical criteria of hemophagocytic syndrome resolved within 1 week, but the patient developed steroid induced hallucinations and amnesia. Hence dexamethasone was withdrawn. Magnetic resonance imaging of brain was normal. Cyclosporine A was initiated at a dose of 125 mg/day (3 mg/kg of weight) which the patient tolerated and after 6 months of treatment, the dose was tapered gradually. The disease is now well controlled with 25mg/day of cyclosporine A.
Even at the end of 12 months the patient is in clinical remission. Hemophagocytic syndrome is an uncommon hematologic disorder characterized by at least five of the following eight findings: fever >38.5°C, splenomegaly, cytopenias, hypertriglyceridemia, hemophagocytosis in bone marrow, spleen, lymph node, or liver, low or absent NK cell activity and elevated soluble CD25 and ferritin.[2]
According to published literature, the presence of hemophagocytic syndrome might change the management approach and outcome in subcutaneous panniculitis-like T-cell lymphoma. Systemic steroids and other immunosuppressive agents are considered the first line treatment for noncomplicated subcutaneous panniculitis - like T-cell lymphoma although radiotherapy, surgery, and stem-cell transplantation can also be used in selective patients. Subcutaneous panniculitis-like T-cell lymphoma which is resistant, progressive or complicated by hemophagocytic syndrome is traditionally treated with multiagent chemotherapeutic regimens such as cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP).[1]
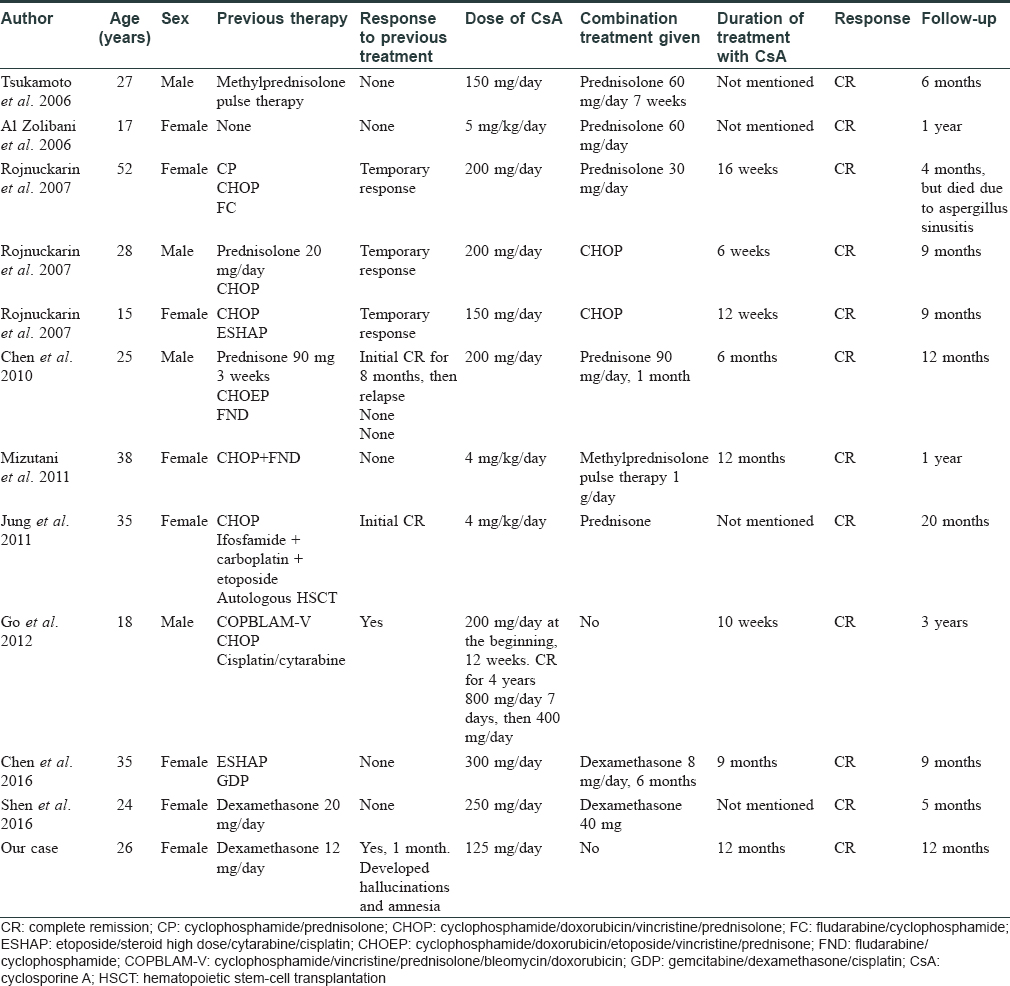
Since 2006, 11 patients with subcutaneous panniculitis-like T-cell lymphoma associated with hemophagocytic syndrome have been treated with oral cyclosporine [Table - 1] with good outcome.[3],[4] One of them was directly started on a combination treatment of cyclosporine A with high doses of prednisolone and had complete resolution,[3] while two patients who had no response with systemic corticosteroids alone achieved complete remission on combining with cyclosporine A.[4],[5] In the remaining patients, cyclosporine A was used after relapse or resistance to chemotherapy or following autologous hematopoietic stem-cell transplantation.[4]
Our experience and recently published data suggest that the occurrence of hemophagocytic syndrome does not necessarily mean a more rapidly progressive disease and worse prognosis in all patients with subcutaneous panniculitis-like T-cell lymphoma. Response and long term remission with oral cyclosporine highlights the need to avoid too aggressive therapies. Future prospective studies with large number of patients are necessary to confirm this hypothesis.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form, the patient has given her consent for her images and other clinical information to be reported in the journal. The patient understands that her name and initials will not be published and due efforts will be made to conceal identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Willemze R, Jansen PM, Cerroni L, Berti E, Santucci M, Assaf C, et al. Subcutaneous panniculitis-like T-cell lymphoma: Definition, classification, and prognostic factors: An EORTC cutaneous lymphoma group study of 83 cases. Blood 2008;111:838-45.
[Google Scholar]
|
| 2. |
Jordan MB, Allen CE, Weitzman S, Filipovich AH, McClain KL. How I treat hemophagocytic lymphohistiocytosis. Blood 2011;118:4041-52.
[Google Scholar]
|
| 3. |
Al Zolibani AA, Al Robaee AA, Qureshi MG, Al Nosian H. Subcutaneous panniculitis-like T-cell lymphoma with hemophagocytic syndrome successfully treated with cyclosporin A. Skinmed 2006;5:195-7.
[Google Scholar]
|
| 4. |
Chen CC, Teng CL, Yeh SP. Relapsed and refractory subcutaneous panniculitis-like T-cell lymphoma with excellent response to cyclosporine: A case report and literature review. Ann Hematol 2016;95:837-40.
[Google Scholar]
|
| 5. |
Shen G, Dong L, Zhang S. Subcutaneous panniculitis-like T cell lymphoma mimicking early-onset nodular panniculitis. Am J Case Rep 2016;17:429-33.
[Google Scholar]
|
Fulltext Views
3,489
PDF downloads
2,656





