Translate this page into:
Is this psoriasis or something else?
Corresponding author: Dr. Emel Öztürk Durmaz, Acıbadem Maslak Hospital, Büyükdere Caddesi 40, Maslak 34457, Istanbul, Turkey. emelerkek@yahoo.com
-
Received: ,
Accepted: ,
How to cite this article: Duman DD, Durmaz EÖ, Demirkesen C, Şahin S. Is this psoriasis or something else? Indian J Dermatol Venereol Leprol 2022;88:682-4.
A 38-year-old man presented with a history of intractable itchy eruption on the buttocks, present for the last 6 years. The lesions had gradually spread over time and did not respond to several topical steroids. Dermatological examination revealed a butterfly-shaped erythematous verrucous plaque, involving both buttocks and gluteal cleft [Figure 1], and peripheral guttate red-brown discrete papules [Figure 2]. Histologic examination of a punch biopsy specimen displayed orthokeratosis, follicular plugging, numerous oblique columns of parakeratosis called cornoid lamellae, extending at about 45 degrees from the surface of the epidermis and showing invagination into the epidermis. There was loss of granular layer under the cornoid lamellae and dyskeratotic cells were seen [Figure 3]. A detailed laboratory investigation including hepatitis B and C panels yielded normal findings. A 6-week trial of acitretin at a dose of 30 mg/day, and a 2-month trial of tazarotene 0.1% cream twice daily were futile in eradicating the lesions and alleviating his pruritus.

- Butterfly-shaped hyperkeratotic erythematous plaque, bilaterally and symmetrically situated on the buttocks
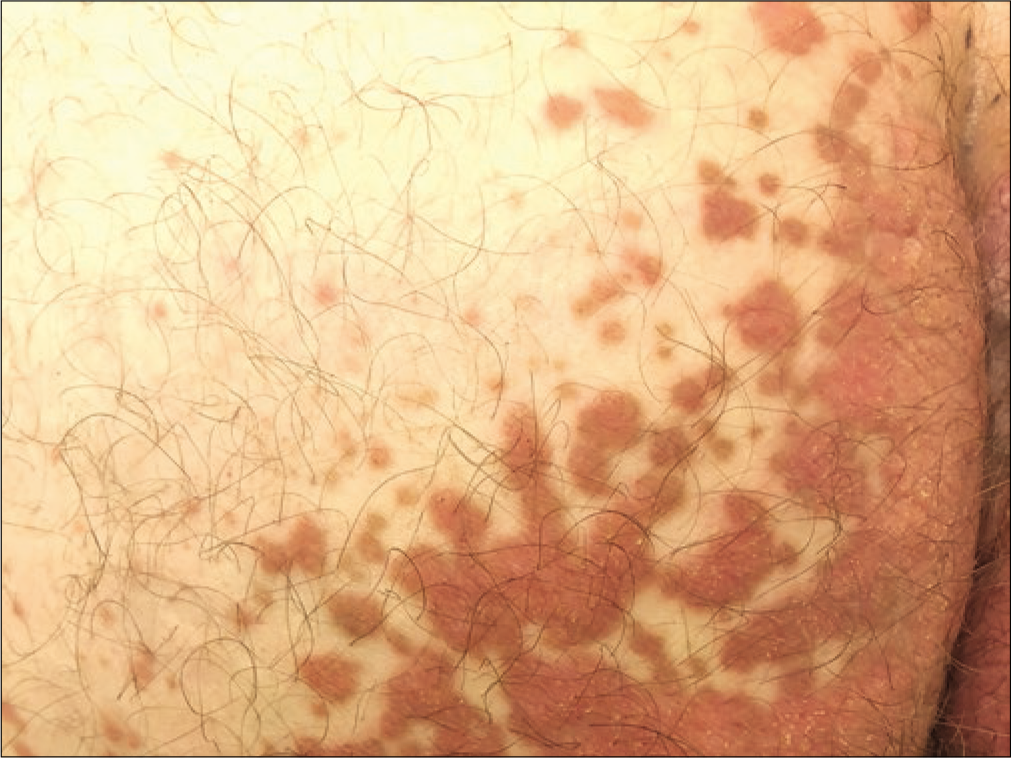
- Red-brown discrete hyperkeratotic papules within the vicinity of main plaque
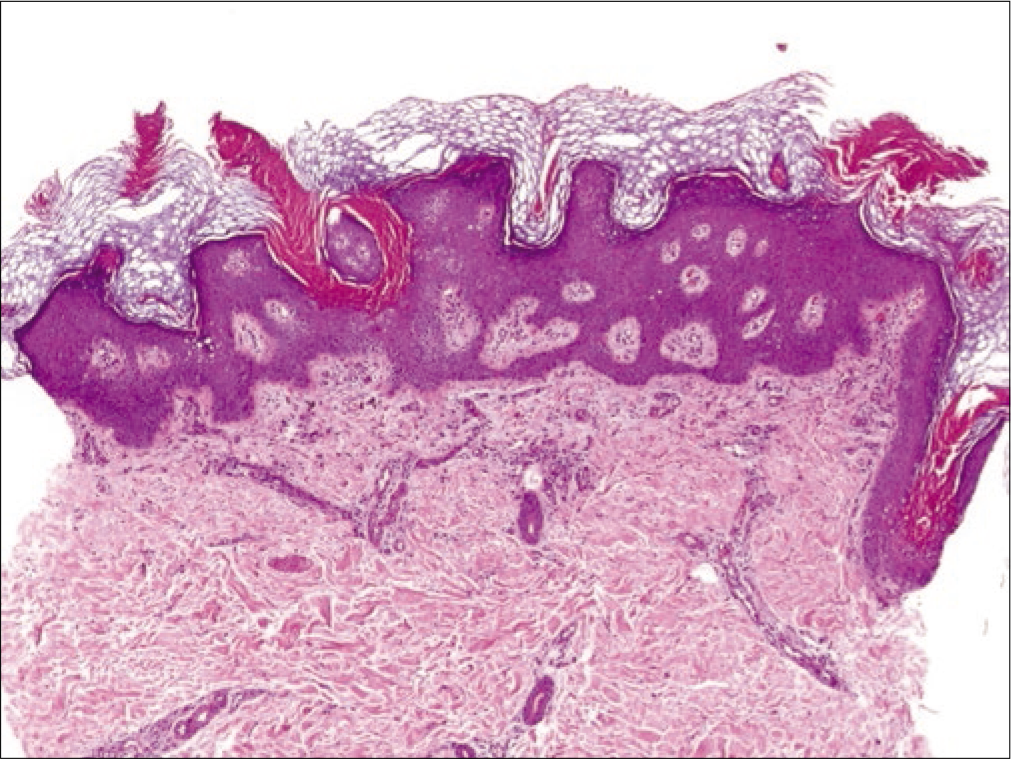
- Multiple oblique columns of parakeratosis, alternating with hyperkeratosis and follicular plugging. Note irregular papillomatous proliferation of the epidermis (H and E, ×400)
Question
What is your diagnosis?
Diagnosis
Porokeratosis ptychotropica.
Discussion
Porokeratosis ptychotropica represents a novel, rare, under-recognized and a distinct form of porokeratosis. The term “ptychotropica” is derived from the Greek words ‘ptyche’ denoting fold and ‘trope’ denoting turning, and alludes to flexural localization of the disorder. For mysterious reasons, porokeratosis ptychotropica has a predilection for adult males.1 Nevertheless, it has also been documented in children.2 The majority of reported cases are sporadic. However, familial cases, suggesting an autosomal dominant inheritance, have been described.3
Classical clinical presentation of porokeratosis ptychotropica consists of slowly enlarging, pruritic, bilaterally symmetrical, verrucous plaques in a butterfly motif, usually involving the natal cleft and buttocks. The lesions tend to coalesce centrally and expand gradually over time, with the formation of peripheral satellite, red-brown hyperkeratotic papules. Occasionally, verrucous papules and plaques may extend to involve the penis, scrotum, vulva and thighs. Itching and discomfort are the most important complaints elicited.1,3
The definitive diagnosis of porokeratosis ptychotropica is a challenge and may be delayed for several years or even decades.1 We believe that, owing to misdiagnoses, the actual prevalence of the disorder may be much higher than suggested by the relevant literature. In our case, the disorder simulated psoriasis and neurodermatitis, and definitive diagnosis could only be established 6 years after the onset. This case taught us that persistent psoriasiform and verrucous gluteal plaques should be biopsied in order to exclude porokeratosis ptychotropica.
Skin biopsy is the gold standard for diagnosis. Histologically, porokeratosis ptychotropica harbours multiple cornoid lamellae, responsible for the hyperkeratotic and verruciform clinical appearance. The presence of numerous cornoid lamellae also distinguishes this disorder from the classical porokeratosis of Mibelli, where the cornoid lamellae are only a few in number and exist only at the periphery.1,3
The etiology of porokeratosis ptychotropica is an enigma. The role of human papillomavirus infection has not been proven.4 Both genetic and environmental factors have been implicated, including ultraviolet light exposure, infections, drugs, immunosuppression and repeated trauma (friction with clothing, scratching, sweating). Trauma may exacerbate the disorder by inducing a Koebner-like effect, with the development of look-alike lesions. 1 It has been conjectured that porokeratosis ptychotropica is the end stage of a local proliferation of porokeratosis of Mibelli-like lesions, prompted by koebnerization and/or lichenification.5 Recently, the first case of porokeratosis ptychotropica transforming into invasive squamous cell carcinoma has been reported by Mazori et al.4 Because of such an impending risk, close long-term follow up of affected patients has been recommended.3,4
Treatment options in porokeratosis ptychotropica are generally impeded by temporary, disappointing or futile outcomes, and are eventually followed by recurrences.1 The favorable effects, if ever attained, are only partial and comprise symptomatic relief and flattening of the lesions. Our patient has not responded to oral acitretin and topical tazarotene. So far, complete remission has only been observed with dermatome slicing.1 Surgical excision might be a convenient option in small lesions.2,3
There is increasing evidence implicating that porokeratoses are related to aberrant terminal differentiation of keratinocytes, connected to postzygotic mosaic somatic mutations in enzymes of the mevalonate pathway. The resultant defect is in cholesterol biosynthesis which might judiciously be treated with topical or systemic inhibitors of 3-hydroxy-3-methyl-glutaryl-coenzyme A reductase enzyme.2 Thus, the future holds promise for therapeutic optimism in porokeratoses.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- Genitogluteal porokeratosis: A clinical review. Clin Cosmet Investig Dermatol. 2018;11:219-29.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical course of porokeratosis ptychotropica over 7 years in an otherwise healthy child. Pediatr Dermatol. 2020;37:248-50.
- [CrossRef] [PubMed] [Google Scholar]
- Verrucous porokeratosis of the gluteal cleft (porokeratosis ptychotropica): A rare disorder easily misdiagnosed. J Cutan Pathol. 2010;37:802-7.
- [CrossRef] [PubMed] [Google Scholar]
- Transformation of porokeratosis ptychotropica into invasive squamous cell carcinoma. Int J Dermatol. 2017;56:679-80.
- [CrossRef] [PubMed] [Google Scholar]
- Porokeratosis ptychotropica: A rare variant with discrete lesions. Australas J Dermatol. 2015;56:e28-9.
- [CrossRef] [PubMed] [Google Scholar]





