Translate this page into:
Isolated plantar cerebriform collagenoma
2 Department of Pathology, Maulana Azad Medical College, Delhi, India
Correspondence Address:
Deepshikha Khanna
C 68 Z 4 Dilshad Garden, Delhi
India
| How to cite this article: Khanna D, Goel K, Khurana N. Isolated plantar cerebriform collagenoma. Indian J Dermatol Venereol Leprol 2012;78:666 |
Sir,
A 9-year-old girl presented to pediatric dermatology department with raised lesion over the right foot associated with on and off discomfort present since infancy. Examination revealed a raised white colored mass 3 × 2.5 cm in size with well-defined irregular margins on the plantar surface of right foot. The lesion had a velvety surface with numerous gyri and grooves giving it a cerebriform surface [Figure - 1]. Systemic examination was unremarkable and skeletal survey did not reveal any exostosis. Histopathological examination showed mild acanthosis and papillomatosis. Dermis showed presence of thick collagen bundles arranged haphazardly extending to and replacing the subcutis [Figure - 2]a. Masson′s trichrome stain confirmed excess of collagen bundles [Figure - 2]b. Elastic fibers were markedly reduced and acid mucopolysaccharides were not increased.
 |
| Figure 1: Whitish cerebriform mass over the plantar surface of foot |
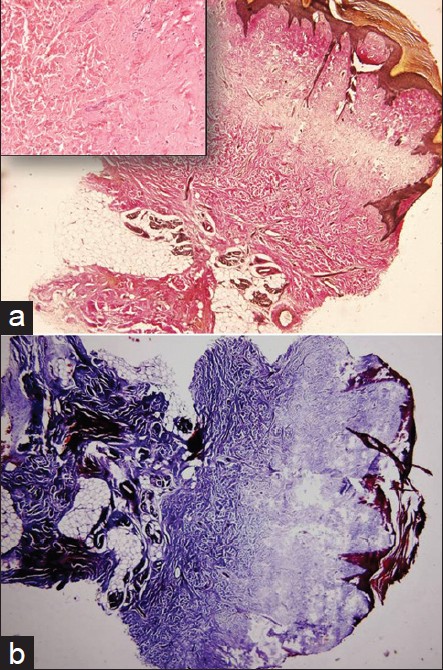 |
| Figure 2: (a) Thick collagen bundles extending to and replacing the subcutis (H and E, ×40). Inset reveals thick collagen bundles (H and E, ×250) (b) Dense blue color on Masson's trichrome stain depicting fibrosis extending into subcutaneous fat lobules. (Masson's trichrome, ×40) |
Connective tissue nevi are circumscribed hamartomatous malformations in which one or more components of dermis are altered. Based on the predominant tissue involved, these may be classified as collagenomas (collagen), elastomas (elastin), or nevus mucinosis (proteoglycans). Collagenomas may be isolated, either sporadic or hereditary, or syndromic as in Tuberous sclerosis or Proteus syndrome (PS). Histologically, there is increase in collagen fibers that are arranged haphazardly in the dermis. Elastic fiber stains show normal or diminished elastic fibers. There is no increase in fibroblasts or mucopolysaccharides.
Plantar cerebriform collagenoma (PCC), also termed as paving stone nevus, is a type of isolated collagenoma that presents in childhood as variably sized flesh colored cerebriform mass on the sole and constitutes one of the specific criterion for diagnosis of PS. PCC is a type of cerebriform connective tissue nevus (CCTN). The latter is found most commonly on the soles, and occasionally on the hands and the nares or medial puncta of eyes. [1] Isolated PCC are very rare and there are only five reports of isolated PCC in literature to the best of our knowledge. [2],[3],[4],[5],[6]
PS comprises of asymmetrical overgrowth of any part of the body, exostosis, cranial hyperostosis, verrucous epidermal nevi, vascular malformations, and lipoma like hamartomas. Diagnosis of PS requires presence of various specific and all general criteria that include mosaic distribution, progressive course, and sporadic occurrence. Presentation of PS is often variable and the findings seen commonly like epidermal nevus and vascular malformations may also be associated with other syndromes such as neurofibromatosis, Klippel-Trenaunay syndrome, Bannayan syndrome, and Mafucci syndrome. However, CCTN is not found in any of these syndromes and is the only specific criterion that alone in association with general criteria is sufficient to make a diagnosis of PS.
Patients with mild PS have lesser proportion of their body affected rather than substantial areas with mild disease. As a result some patients exhibiting very limited phenotype with isolated findings may remain undiagnosed. Though PTEN tumor suppressor gene abnormalities have been described in the past, it is postulated that PS is caused by mutation leading to somatic mosaicism that would otherwise be lethal in the nonmosaic state. [1] Botella-Estrada et al. suggested that patients with localized findings such as isolated PCC may represent a specific PS group where the somatic mutation occurred later in fetal development. [2] Luo et al. reported a female patient with delayed and mild form of PS in whom clinical features began to appear at 15 years of age while diagnosis of PS was made when the patient was 30 years old. They have speculated the possibility of female hormones resulting in mild and delayed onset disease. Their patient did not have progressive and disproportionate overgrowth that is the hallmark of PS. [7] Interestingly, barring one case, all isolated PCCs have been reported in females.. In addition, all these patients had relatively smaller lesions (maximum size 4 × 5 cm) as compared with the large and extensive PCC covering the entire foot in patients with PS. [2],[3],[4],[5],[6]
It is possible that isolated PCC may be just one end of the continuum of PS spectrum and a delayed somatic mutation further suppressed by female sex hormones resulted in limited phenotype with isolated manifestations like PCC in these patients. Long-term follow-up to assess the natural history in cases with characteristic findings presenting alone may reveal delayed onset of other manifestations and diagnosis as PS in some of these patients. This may in turn help to identify a specific PS group with a benign clinical course. In future, prognostics factors such as size or gender may be delineated in patients with isolated findings to identify a subgroup that may require long-term follow-up for PS.
| 1. |
Biesecker L. The challenges of Proteus syndrome: Diagnosis and management. Eur J Hum Genet 2006;14:1151-7.
[Google Scholar]
|
| 2. |
Botella-Estrada R, Alegre V, Sanmartin O, Ros C, Aliaga A. Isolated plantar cerebriform collagenoma. Arch Dermatol 1991;127:1589-90.
[Google Scholar]
|
| 3. |
Martinez W, Arnal F, Capdevila A, Almagro M. Isolated plantar cerebriform collagenoma. Pediatr Dermatol 1994;11:84-5.
[Google Scholar]
|
| 4. |
Choi JC, Lee MW, Chang SE, Choi JH, Sung KJ, Moon KC, et al. Isolated plantar collagenoma. Br J Dermatol 2002;146:164-5.
[Google Scholar]
|
| 5. |
Nico MM, Valente NY, Machado KA. Isolated plantar collagenoma. Acta Derm Venereol 2003;83:144.
[Google Scholar]
|
| 6. |
Nelson AA, Ruben BS. Isolated plantar collagenoma not associated with Proteus syndrome. J Am Acad Dermatol 2008;58:497-9.
[Google Scholar]
|
| 7. |
Luo S, Feng Y, Zheng Y, Peng Z, Wang G. Mild and delayed-onset Proteus syndrome. Eur J Dermatol 2007;17:172-3.
[Google Scholar]
|
Fulltext Views
3,486
PDF downloads
2,793





