Translate this page into:
Itraconazole plus 640 nm high-power red-light combination therapy for recalcitrant ulcers associated with Talaromyces marneffei infection
Corresponding author: Dr. Jing Wang Department of Dermatology, The Eighth Affiliated Hospital Sun Yat-sen University, Shenzhen, Guangdong, China. wangj567@mail.sysu.edu.cn
-
Received: ,
Accepted: ,
How to cite this article: Chen MH, Xu J, Xu SM, Song PF, Wang J. Itraconazole plus 640 nm high-power red-light combination therapy for recalcitrant ulcers associated with Talaromyces marneffei infection. Indian J Dermatol Venereol Leprol. 2024;90:266. doi: 10.25259/IJDVL_868_18
Dear Editor,
Talaromyces marneffei (T. marneffei) is a fatal pathogenic fungus that invades the skin of immunocompromised patients, especially those with AIDS. Although early, appropriate antifungal treatment may result in a better prognosis in general, the ulcers in T. marneffei infected patients are difficult to heal. Here, we report three cases of refractory ulcers successfully treated by combining anti-fungal drugs and high-power red-light.
Case 1
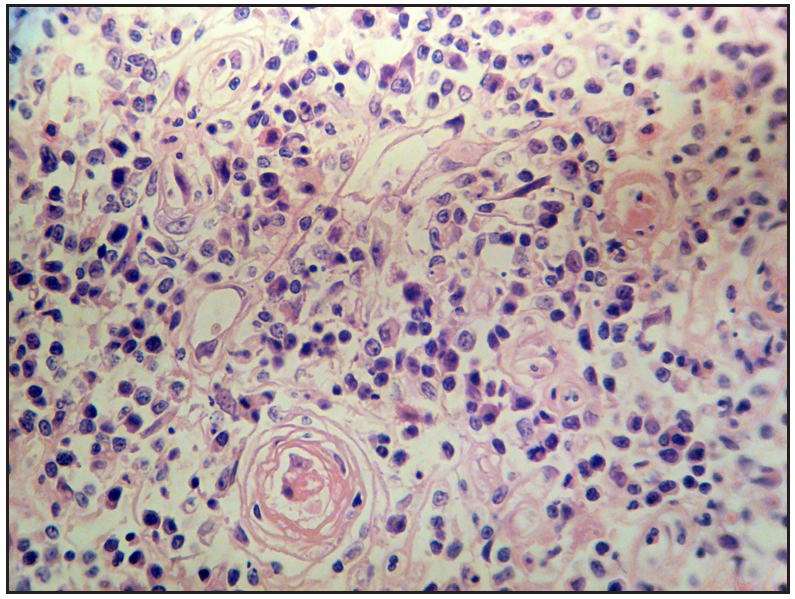
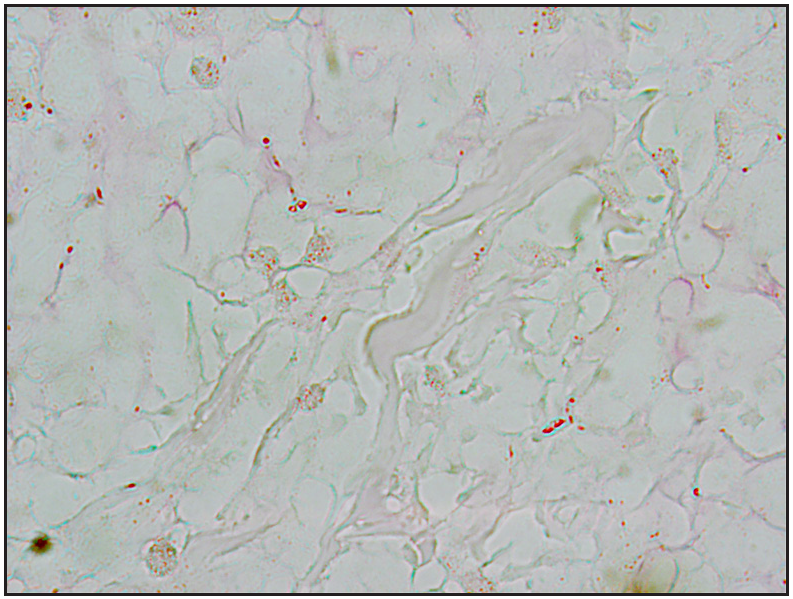
A 40-year-old HIV-positive male patient was admitted to our hospital with a two-year history of generalised necrotic skin rash, itching and ulcers on the buttocks [Figure 1a]. The patient visited a local hospital due to intermittent cough and fever that lasted for two months and received antibiotics. Upon further evaluation, he was diagnosed with systemic T. marneffei infection, AIDS, anaemia and bacterial pneumonia. He was treated with fluconazole 400 mg daily together with antibiotics for four weeks and was also simultaneously started on highly active antiretroviral therapy, which was continued. The fever and lung infection were brought under control, but the gluteal ulcers had worsened. The patient was then transferred to our hospital. Ulcer biopsy slides showed granulomas in the dermis consisting of a large number of eosinophils, some neutrophils, lymphocytes, histiocytes and multinucleate giant cells [Figure 1b]. PAS positive fungal spores were identified in the dermis and subcutaneous tissue [Figure 1c]. The smear from the ulcer didn’t reveal any positive acid-fast bacilli on staining.

- Case 1- Multiple ulcers over the buttocks, before therapy.
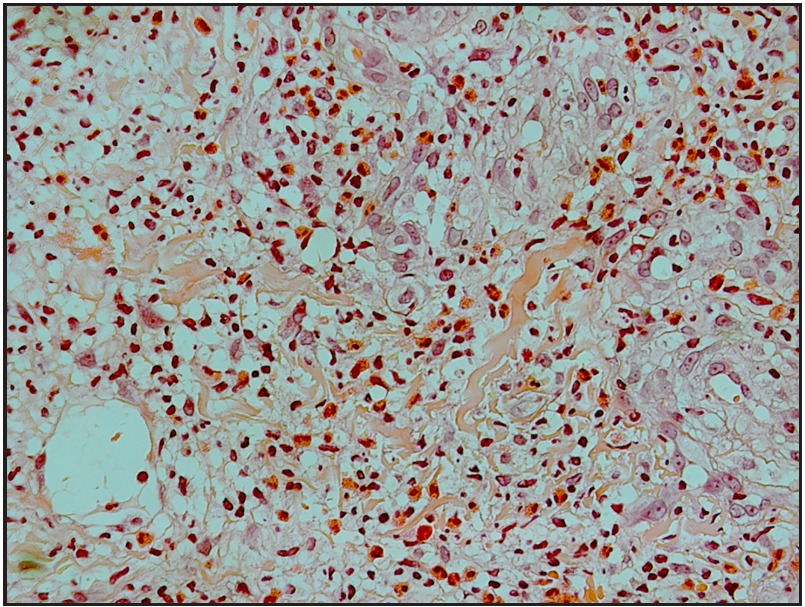
- Histopathology showed infiltration of multiple inflammatory cells, large number of eosinophils and small round or oval fungal spores (H&E, 400×).
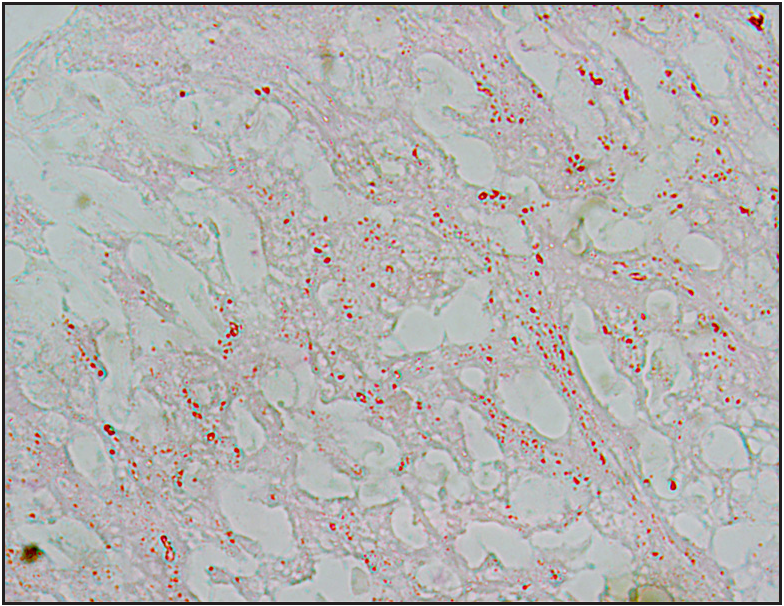
- PAS positive spores (PAS, 400×).
Case 2
A 29-year-old HIV positive male patient had multiple large ulcers on the perianal, glans penis and sacral regions [Figure 2a] and had an intermittent fever since three months. Laboratory investigations showed that he CD4+ T-cell count was 29/µl. T. marneffei was identified in blood cultures. Histology from the ulcer showed granulomas and PAS positive fungal spores [Figures 2b and 2c]. Diagnosed with T. marneffei infection and AIDS, he was then given highly active antiretroviral therapy including cotrimoxazole and fluconazole 400 mg daily for 10 weeks. New ulcers still continued to appear gradually.

- Case 2- Before therapy.
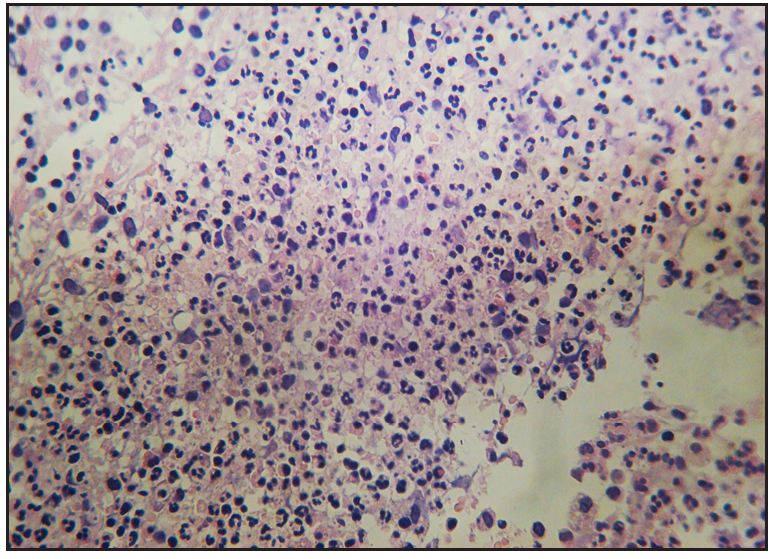
- Histopathology showed infiltration of the inflammatory cells. Most of the cells were lymphoid cells with small number of eosinophils (H&E, 200×).
- A few PAS positive spores: allanto-like with abjunctions (PAS, 400×).
Case 3
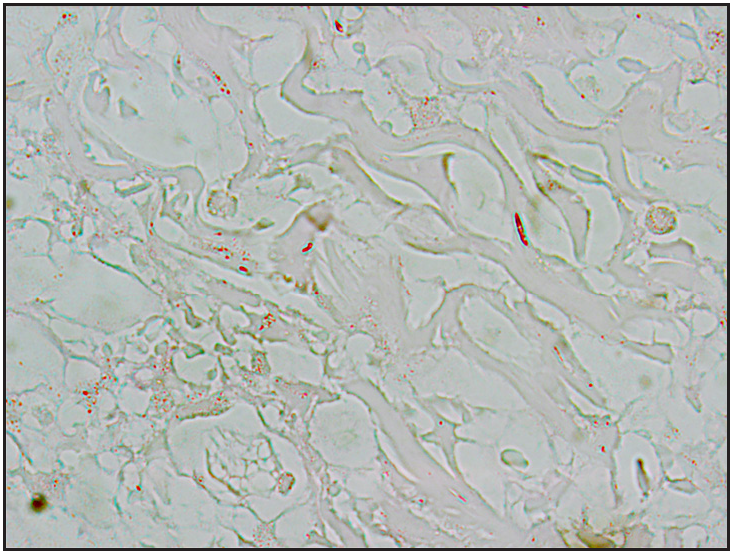
A 76-year-old male patient presented with a nontender, slowly growing, ulcerative plaque and nodule on his right foot [Figure 3a]. A physical examination found ipsilateral inguinal lymphadenopathy. He had lost five kilograms of body weight over nine months. Erythromycin, gentamycin and fluconazole were administered with little effect. The routine examination of blood, urine, stool, liver and renal functions was normal. T. marneffei was identified in fungal cultures from both blood and skin biopsy tissues. The pus swab culture reported enterococcus faecalis. The ulcer skin biopsy showed granulomas and PAS positive fungal spores [Figures 3b and 3c]. He was then diagnosed with a T. marneffei infection.

- Before the treatment: large ulcer and multiple nodules on the foot.
- Histopathology showed inflammatory cells infiltration (H&E, 400×).
- PAS positive spores: small round or oval red particles 2–3 µm in size (PAS, 400×).
The recalcitrant ulcers in patients with severe cutaneous T. marneffei infections are difficult to treat. Two of the three patients were treated with fluconazole 400 mg daily, but the ulcers showed no noticeable improvement. Therefore, we devised a therapy combining antifungal medication with high-power red-light radiation. Itraconazole was given 200 mg orally twice daily for at least 4 weeks, followed by 200 mg orally daily for at least 24 weeks. While taking itraconazole, the case two patient was treated with high-power 640 nm visible LED red light (Lifotronic Technology Co. Ltd) with 120 mw/cm2 density and 216 J/cm2 energy density (30 minutes) daily. Case 1 and 3 patients received the same red-light treatment twice daily. Within 7 days, the combination therapy elicited good response in all three patients, with lesional healing, reduced oedema and exudation. The ulcers showed improvement in 1–2 weeks and healed in 4–8 weeks [Figures 4a, 4b and 4c]. No adverse effects were observed in any of the three patients during the combined therapy.

- Case 1- After 8 weeks of combination therapy; the ulcer has healed.

- Four weeks after therapy: the ulcer healed.

- Ten weeks after therapy: the ulcer and nodules resolved.
T. marneffei usually causes opportunistic infections and is endemic in South-East Asia.1 Early diagnosis and prompt, effective management are important to avoid life-threatening systemic mycosis. The typical clinical manifestations include fever, anaemia, weight loss, lung infection, hepatic involvement and lymphadenopathy.2 The characteristic skin lesions such as umbilicated papules or nodules with a necrotic centre, resembling those seen in molluscum contagiosum, are the most common symptoms of cutaneous T. marneffei infection.3 In line with other reports, ulcers are the earliest manifestation associated with T. marneffei.4 In addition, patients with cutaneous T. marneffei infection are more likely to have combined bacterial infections, resulting in refractory large ulcers. In this scenario, antifungal monotherapy has limited efficacy.
A high-dose antifungal agent is usually effective for T. marneffei infections. The minimum inhibitory concentrations of the commonly used medicines, ranking from lowest to highest, are voriconazole, itraconazole, terbinafine, amphotericin-B and fluconazole.5 For our patients, itraconazole 400 mg per day was more efficient than the previous treatments. For AIDS patients with T. marneffei, highly active antiretroviral therapy together with antifungal therapy should be initiated early.1 After initiating antiretroviral therapy, immunosuppression may improve. Under this condition, the antifungal therapy becomes more effective and the antifungal prophylactic regimen aiming to reduced risk of T. marneffei relapse might be discontinued sooner.
Previous reports showed that skin ulcers and infections benefit from low-level light/laser therapy.6 The benefits may be explained by the improved blood flow and neovascularization, decreased inflammatory cell levels, induction of anti-inflammatory cytokines, chemokines and other mediators. It may also restore the collagenesis/collagenase balance, which accelerates wound healing.6 In our experience, in all these three cases, the new therapy, which combined an anti-fungal drug and a high-power red-light, drastically improved the ulcers. However, the exact mechanism underlying the accelerated wound healing and fungicidal effect of the combination therapy remains to be determined.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflict of interest.
References
- Penicillium marneffei infectionin AIDS. Patholog Res Int. 2011;2011:764293.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- Penicillium marneffei infection: an emerging disease in mainland China. Mycopathologia. 2013;175:57-67.
- [CrossRef] [PubMed] [Google Scholar]
- A retrospective review on successful management of Penicillium marneffei infections in patients with advanced HIV in Hospital Sungai Buloh. Med J Malaysia. 2012;67:66-70.
- [CrossRef] [PubMed] [Google Scholar]
- Penicillium marneffei infection presenting as vulv-ulcer in an HIV-infected woman. Eur J Med Res. 2011;16:425-6.
- [CrossRef] [PubMed] [PubMed Central] [Google Scholar]
- In vitro antifungal drug susceptibilities of Penicillium marneffei from China. J Infect Chemother. 2013;19:776-8.
- [CrossRef] [PubMed] [Google Scholar]
- Organic light emitting diode improves diabetic cutaneous wound healing in rats. Wound Repair Regen. 2015;23:104-14.
- [CrossRef] [PubMed] [Google Scholar]





