Translate this page into:
Keratosis follicularis spinulosa decalvans
Correspondence Address:
Anuj Bhatnagar
Department of Dermatology, Armed Forces Medical College, Pune - 411 040, Maharashtra
India
| How to cite this article: Verma R, Bhatnagar A, Vasudevan B, Kumar S. Keratosis follicularis spinulosa decalvans. Indian J Dermatol Venereol Leprol 2016;82:214-216 |
Sir,
Keratosis follicularis spinulosa decalvans (KFSD) is a rare, usually X-linked recessive disorder presenting with progressive cicatricial alopecia of the scalp and eyebrows. Males are more commonly affected. Treatment with emollients, keratolytics and retinoids may be helpful.
A 15-year-old boy, fifth child of a non-consanguineous marriage, presented to us with complaints of recurrent, raised, scaly, itchy lesions over the scalp of 7 years duration. Symptoms started 7 years back when his mother noticed some red, raised lesions on a few areas over the scalp. Lesions were mildly itchy and oozy at times. Gradually, the lesions increased in size and number to involve the forehead, nape of the neck and eyebrows. Later, he noticed a reduction in hair density of the scalp and eyebrows. He had several exacerbations and remissions since then. There was no significant response to treatment from various doctors. His siblings and other family members were unaffected.
On examination, there was patchy involvement of the scalp, nape of the neck, forehead and supraorbital ridges in the form of multiple, discrete to confluent erythematous papules and scaly plaques of varying sizes [Figure - 1]a and b and [Figure - 2]a. Multiple variably sized patches of scarring alopecia were present on the scalp, predominantly over the occipital and temporal areas. Scarring alopecia involving the lateral half of both eyebrows was seen [Figure - 1]c and d. Multiple tiny follicular papules were present on the axilla and back [Figure - 2]b and c. Bilaterally symmetrical plantar keratoderma was also present [Figure - 2]d. Mild scaling was seen in the inguinal region. Investigations revealed a mild leukocytosis of 12,600/cumm (normal range: 4000-11,000/cumm) and eosinophilia with an absolute eosinophil count of 3150/cumm (normal: 450/cumm). Serum IgE was 4654 U/ml (normal: 150-1000 U/ml). Pus culture showed growth of Staphylococcus aureus. Stool for ova was negative.
 |
| Figure 1: Characteristic skin lesions of keratosis follicularis spinulosa decalvans: (a) Erythematous papules on scalp, forehead and eyebrows with scaling, (b) lateral view of the same, (c) scarring alopecia of scalp with shiny atrophic skin and scarring alopecia of left eyebrow, (d) similar changes on right eyebrow |
 |
| Figure 2: (a) Characteristic follicular papules on nape of neck, (b) follicular papules on back, (c) follicular papules in axilla with scanty hair, (d) plantar keratoderma |
Skin biopsy from the scalp revealed acanthosis with hyperkeratosis over the hair follicle epithelium with inflammatory changes in the dermis [Figure - 3]. Characteristic follicular plugging and a moderate inflammatory infiltrate, especially around appendages and vessels were present. The infiltrate was mainly lymphocytic in nature. The patient was treated with 12.5 mg of acitretin and emollients after an initial course of antibiotics. Significant resolution of lesions was observed after 8 weeks. Oral retinoids were continued for a total of 16 weeks. No recurrence was seen in 6 months and he is still on regular follow-up [Figure - 4].
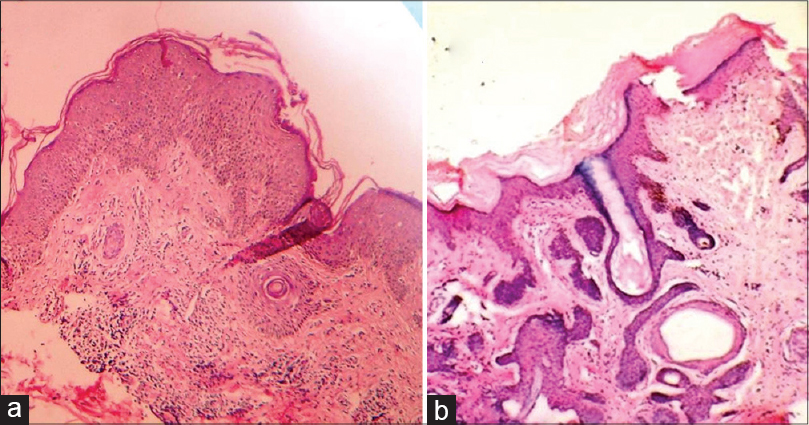 |
| Figure 3: (a) Follicular plugging, nodular infiltrates in dermis and papillary dermal inflammation H and E, ×100, (b) Follicular plug with hyperkeratosis H and E, ×400 |
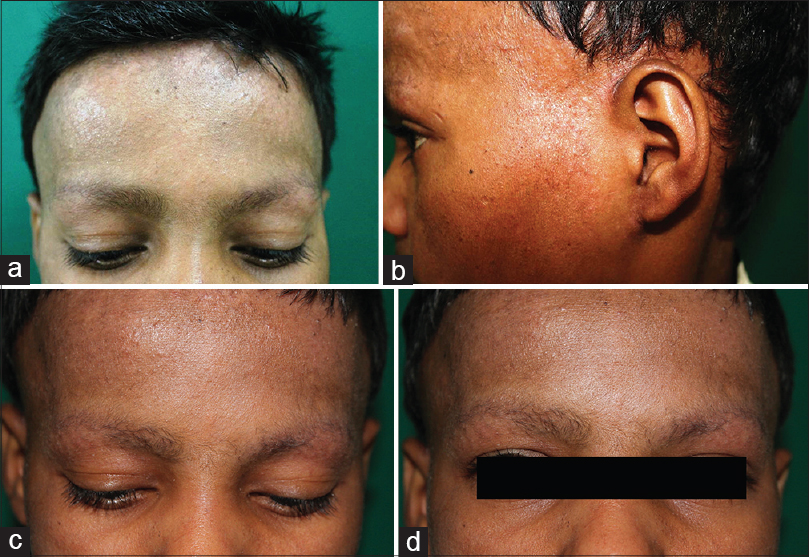 |
| Figure 4: Regression of skin lesions on follow-up: (a) Forehead revealing the papules, (b) reduced scaling with persistent scarring alopecia of the parieto-temporal area with a few follicular papules still present, and (c and d) reduced scaling with persistence of scarring alopecia of eyebrows |
Keratosis follicularis spinulosa decalvans is a rare type of scarring alopecia described initially by Macleod, characterized by lymphocytic predominance in histological sections. [1],[2],[3] This condition, along with keratosis atrophicans facei and atrophoderma vermiculatum represent closely related disorders. Though usually inherited in an X-linked recessive pattern, autosomal forms and sporadic cases have also been frequently reported. Family history of similar disorders may not always be evident. The condition usually begins at an early age with generalized keratosis pilaris and gradually progresses to scarring alopecia along with ocular changes such as photophobia and corneal dystrophy. [4] The alopecia may be patchy and limited, or even widespread. Exacerbation at puberty with the eruption of pustules, crusting and extensive scaling on the scalp may occur. Therapy is generally symptomatic. Among treatment options, topical keratolytics, emollients and Vitamin A derivatives have been known to show some benefit. [5],[6] Therapy is most beneficial when administered early in childhood. In the pustular variant, systemic antibiotics have been used to improve pustular flares.
Our patient had all the classical features of keratosis follicularis spinulosa decalvans with the exception of eye changes. He also had laboratory features suggestive of an atopic diathesis which is a well-known association. [7] Other reported associations include Noonan′s syndrome, deafness, cutis laxa, large pinnae, clinodactyly and aminoaciduria. [8] Plantar keratoderma in our case was mild and diffuse but focal plantar keratoderma is known to be an association. [9] In this case, seborrheic dermatitis was a close differential diagnosis. However, the presence of follicular papules on the scalp, nape of the neck and rest of the body along with scarring alopecia, especially of the eyebrows and involvement beyond hairline helped to exclude this condition. Lichen planopilaris was ruled out due to the presence of eyebrow involvement, follicular papules on the nape of the neck and extensive scaling. Histopathology was helpful in ruling out some of the other differential diagnoses and was supportive of keratosis follicularis spinulosa decalvans, where the diagnosis is mainly clinical.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
| 1. |
Sequeira FF, Jayaseelan E. Keratosis follicularis spinulosa decalvans in a female. Indian J Dermatol Venereol Leprol 2011;77:325-7.
[Google Scholar]
|
| 2. |
Macleod JM. Three cases of ichthyosis follicularis associated with baldness. Br J Dermatol 1909;21:165-89.
[Google Scholar]
|
| 3. |
Sellheyer K, Bergfeld WF. Histopathologic evaluation of alopecias. Am J Dermatopathol 2006;28:236-59.
[Google Scholar]
|
| 4. |
Reddy BS, Thadeus J, Garg BR, Rathnakar C. Keratosis follicularis spinulosa decalvans. Indian J Dermatol Venereol Leprol 1995;61:106-8.
[Google Scholar]
|
| 5. |
Maheswari UG, Chaitra V, Mohan SS. Keratosis follicularis spinulosa decalvans: A rare cause of scarring alopecia in two young Indian girls. Int J Trichology 2013;5:29-31.
[Google Scholar]
|
| 6. |
Richard G, Harth W. Keratosis follicularis spinulosa decalvans. Therapy with isotretinoin and etretinate in the inflammatory stage. Hautarzt 1993;44:529-34.
[Google Scholar]
|
| 7. |
Rand R, Baden HP. Keratosis follicularis spinulosa decalvans. Report of two cases and literature review. Arch Dermatol 1983;119:22-6.
[Google Scholar]
|
| 8. |
Britton H, Lustig J, Thompson BJ, Meyer S, Esterly NB. Keratosis follicularis spinulosa decalvans. An infant with failure to thrive, deafness, and recurrent infections. Arch Dermatol 1978;114:761-4.
[Google Scholar]
|
| 9. |
Stevanovic DV. Keratosis follicularis spinulosa decalvans with birefringent hairs. An association with variable keratoderma. Dermatol Monatsschr 1988;174:736-40.
[Google Scholar]
|
Fulltext Views
7,789
PDF downloads
2,565





