Translate this page into:
Keratosis follicularis spinulosa decalvans in a female
Correspondence Address:
Fiona F Sequeira
Department of Dermatology, St. John's Medical College and Hospital, Koramangala, Bangalore, Karnataka-560 034
India
| How to cite this article: Sequeira FF, Jayaseelan E. Keratosis follicularis spinulosa decalvans in a female. Indian J Dermatol Venereol Leprol 2011;77:325-327 |
Abstract
Keratosis follicularis spinulosa decalvans (KFSD), is a rare follicular syndrome associated with widespread keratosis pilaris and progressive scarring alopecia. This genodermatoses often starts at infancy or early childhood with an X-linked mode of inheritance. Males are predominantly affected and females frequently show no disease or only a mild form. We describe this not so common entity of KFSD in a nine year old female child.Introduction
Keratosis pilaris atrophicans (KPA) is the umbrella term for a group of three rare and distinct clinical entities representing the scarring types of keratosis pilaris. Three categories of KPA include: Keratosis pilaris atrophicans faciei (KPAF), Atrophoderma vermiculatum (AV) and Keratosis follicularis spinulosa decalvans (KFSD). They have the following features in common: keratotic follicular papules, nonpurulent inflammation of variable degree, and atrophic end stages characterized by irreversible hair loss and/or atrophic depressions similar to pitted scars. All of these disorders appear to be hereditary. Although in its characteristic form it is considered as a harmless condition, in many instances the lesion can cause cosmetic problems. No effective therapy is available.
Case Report
A nine year old girl born from a first-degree consanguinous marriage, visited our outpatient department with complaints of rough skin over the scalp since five years and over the body since eight years of age in association with partial loss of scalp and eyebrow hair. At birth, her parents noted the absence of scalp and eyebrow hair, which gradually, over the next three to four years grew to some measure and eventually became scanty. Family history was noncontributory. Physical examination disclosed multiple follicular flesh-colored horny papules over the scalp, eyebrows, cheeks and both upper and lower limbs. A closer view of the scalp, cheek and eyebrow revealed fine scaling and areas of scarring alopecia, punctate atrophy and hair loss of the lateral half of eyebrows [Figure - 1],[Figure - 2],[Figure - 3]. The teeth, nails, palms and soles were found to be normal. She gave no history of photophobia. Ophthalmic examination revealed no abnormal findings
 |
| Figure 1: Scalp showing areas of scarring alopecia and KP lesions |
 |
| Figure 2: Cheeks showing punctate atrophy |
 |
| Figure 3: Bilateral loss of lateral one-third of eyebrows |
Hair microscopy was done to rule out monilethrix and in this case was found to be normal. A punch biopsy specimen from the scalp showed follicular plugging in the epidermis with mild acanthosis, early perifollicular fibrosis with mild lymphocytic infiltrate. The dermis was decreased in thickness with inconspicuous ill-formed sebaceous units. The hair shafts appeared to be normal [Figure - 4]. With all the above findings in hand, a clinical diagnosis of keratosis follicularis spinulosa decalvans was made. Our patient was started on oral azithromycin for five days in view of the infection she had secondary to the excoriation, topical retinoic acid 0.025% on alternate days for the scalp at night and salicylic-steroid lotion during the day. The body was treated with urea and lecithin containing moisturizers. A month later, patient had marked improvement in terms of decreased roughness, increased hair growth and absence of disease progression. She was asked to continue the same topicals and come back for review in a month′s time.
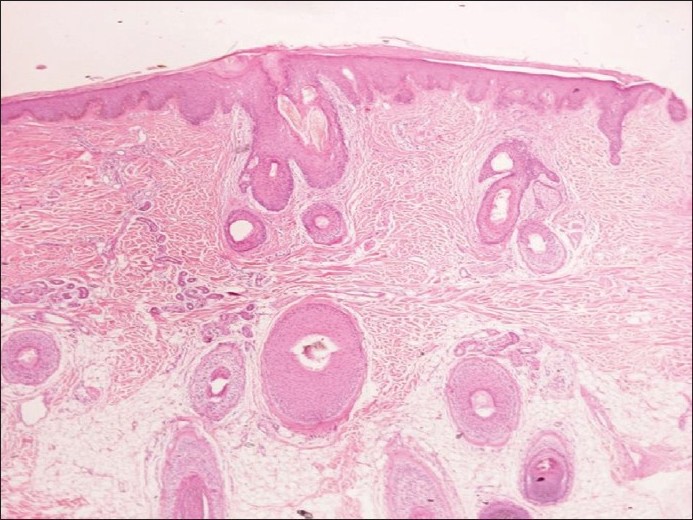 |
| Figure 4: Microscopy-follicular plugging in the epidermis with mild acanthosis, early perifollicular fibrosis with mild lymphocytic infiltrate (H and E, ×200) |
Discussion
Keratosis follicularis spinulosa decalvans, a relatively rare disorder, was first described by Macleod, [1] however, it was Siemens who first used this descriptive term in 1926. [2] It has a X-linked mode of inheritance mapped to a locus at Xp 22.13 - p 22.2. [3] However, the condition has also been seen in families in which the pattern of transmission suggests an autosomal dominant inheritance. [4] Some authors used the appellation of folliculitis spinulosa decalvans (FSD) to define the autosomal dominant form, which could be differentiated from the commoner X-linked one by more pronounced follicular inflammation, particularly evident on the scalp. [5] In general, men are more severely affected while female heterozygotes may exhibit a milder phenotype in families with an X-linked dominant inheritance. [6] The process of lyonization (non-random X inactivation) may explain expression of KFSD in women. A study done by Aten et al., showed that KFSD patients carry mutations in the MBTPS2 gene, and that this affects the normal function of the protein by lowering MBTPS2 activity. MBTPS2 is required for cleavage of sterol regulatory element-binding proteins. [7]
The condition begins in infancy with numerous horny follicular plugs and milia on the nose and cheeks and later on the eyebrows, scalp, neck, and body. Scarring alopecia of the scalp, eyebrows, and eyelashes becomes apparent in childhood and progresses until puberty. Associated features include palmoplantar keratoderma, with predilection for the calcaneal region, and the unusual sign of high cuticles (or long cuticles). [6] The ocular abnormalities include photophobia, keratitis, conjunctivitis, congenital glaucoma and lenticular cataract. [2] Less commonly reported features are atopy, deafness, mental retardation, acne keloidalis nuchae and tufted hair folliculitis , aminoaciduria and woolly hair. [8],[9],[10],[11]
KFSD simulates the ichthyosis follicularis alopecia photophobia (IFAP) syndrome. The latter is characterized by non-scarring alopecia, extensive KP, severe photophobia and corneal dystrophy. [12],[13] The presence of scarring alopecia in our patients favors the diagnosis of KFSD over the IFAP syndrome. The other follicular conditions that it needs to be differentiated from are lichen planopilaris and lichen spinulosus. The former is characterized by atrophic or scarring patches on the scalp with complete loss of follicular orifices. The surrounding marginal hair follicles and residual small hairy islands within the patch reveal perifollicular erythematous macules and scale. Acuminate keratotic plugs can be frequently observed in the margins of the expanding area of alopecia. [14] The latter, a rare and benign disorder is characterized by follicular keratotic papules involving the neck, buttocks, abdomen, trochanteric regions, knees and extensor surfaces of the arms. Lichen spinulosus has a predilection for acral areas unlike keratosis pilaris, which is frequently limited to the upper aspects of the arms and legs. The horny spine that is characteristic of lichen spinulosus can be removed, leaving behind a tiny funnel-like orifice in the papule, whereas an entire individual lesion can be removed with the plug in keratosis pilaris. [15]
So far no effective therapy is known to work for KFSD. Frequent application of topical keratolytic agents and emollients improve skin texture. [4] Antibiotics such as tetracyclines, sulfonamides (dapsone), macrolides, penicillins and rifampin have been used at therapeutic doses and found to be ineffective. [4],[16] Topical and intralesional corticosteroids were tried but caused transient improvement. Etretinate and isotretinoin have also been used but with variable results. [4],[17] It is likely that retinoids, which are useful in disorders of keratinization, act by downregulating the process of follicular hyperkeratosis and inflammation. Laser-assisted hair removal with the long-pulse non-Q-switched ruby laser has been found to be useful in progressive or recalcitrant KFSD. [18]
| 1. |
Macleod JM. Three cases of ichthyosis follicularis associated with baldness. Br J Dermatol 1909;21:165-89.
[Google Scholar]
|
| 2. |
Rand R, Baden HP. Keratosis follicularis spinulosa decalvans- Report of two cases and literature review. Arch Dermatol 1983;199:22-6.
[Google Scholar]
|
| 3. |
Porteous ME, Strain L, Logie LJ, Herd RM, Benton EC. Keratosis follicularis spinulosa decalvans: Confirmation of linkage to Xp22.13-p22.2. J Med Genet 1998;35:336-7.
[Google Scholar]
|
| 4. |
Baden HP, Byers HR. Clinical findings, cutaneous pathology, and response to therapy in 21 patients with keratosis pilaris atrophicans. Arch Dermatol 1994;130:469-75.
[Google Scholar]
|
| 5. |
Oranje AP, Van Osch LD, Oosterwijk JC. Keratosis pilaris atrophicans. Arch Dermatol 1994;130:500-2.
[Google Scholar]
|
| 6. |
Van Osch LD, Oranje AP, Keukens FM, van Voorst Vader PC, Veldman E. Keratosis follicularis spinulosa decalvans: A family study of seven male cases and six female carriers. J Med Genet 1992;29:36-40.
[Google Scholar]
|
| 7. |
Aten E, Brasz LC, Bornholdt D, Hooijkaas IB, Porteous ME, Sybert VP, et al. Keratosis follicularis spinulosa decalvans is caused by mutations in MBTPS2. Hum Mutat 2010;31:1125-33.
[Google Scholar]
|
| 8. |
Britton H, Lustig J, Thompson BJ, Meyer S, Esterly NB. Keratosis follicularis spinulosa decalvans: An infant with failure to thrive, deafness and recurrent infections. Arch Dermatol 1978;114:761-4.
[Google Scholar]
|
| 9. |
Grosshans E, Heid E, Stoll C. Keratosis follicularis spinulosa decalvans and amino-aciduria. Ann Dermatol Venereol 1978;105:433-8.
[Google Scholar]
|
| 10. |
Lacarrubba F, Dall'Oglio F, Rossi A, Schwartz RA, Micali G. Familial keratosis follicularis spinulosa decalvans associated with woolly hair. Int J Dermatol 2007;46:840-3.
[Google Scholar]
|
| 11. |
Janjua SA, Iftikhar N, Pastar Z, Hosler GA. Keratosis follicularis spinulosa decalvans associated with acne keloidalis nuchae and tufted hair folliculitis. Am J Clin Dermatol 2008;9:137-40.
[Google Scholar]
|
| 12. |
Herd RM, Benton EC. Keratosis follicularis spinulosa decalvans: Report of a new pedigree. Br J Dermatol 1996;134:138-42.
[Google Scholar]
|
| 13. |
Eramo LR, Esterly NB, Zieserl EJ, Stock EL, Herrmann J. Ichthyosis follicularis with alopecia and photophobia. Arch Dermatol 1985;121:1167-74.
[Google Scholar]
|
| 14. |
Mehregan DA, Van Hale HM, Muller SA. Lichen planopilaris: Clinical and pathologic study of forty-five patients. J Am Acad Dermatol 1992;27:935-42.
[Google Scholar]
|
| 15. |
Boyd AS. Lichen spinulosus: Case report and overview. Cutis 1989;43:557-60.
[Google Scholar]
|
| 16. |
Bellet JS, Kaplan AL, Selim MA, Olsen EA. Keratosis follicularis spinulosa decalvans in a family. J Am Acad Dermatol 2008;58:499-502.
[Google Scholar]
|
| 17. |
Alfadley A, Al Hawsawi K, Hainau B, Al Aboud K. Two brothers with keratosis follicularis spinulosa decalvans. J Am Acad Dermatol 2002;47:S275-8.
[Google Scholar]
|
| 18. |
Chui CT, Berger TG, Price VH, Zachary CB. Recalcitrant scarring follicular disorders treated by laser-assisted hair removal: A preliminary report. Dermatol Surg 1999;25:34-7.
[Google Scholar]
|
Fulltext Views
5,329
PDF downloads
1,453





